Ann Hepatobiliary Pancreat Surg.
2021 Nov;25(4):523-527. 10.14701/ahbps.2021.25.4.523.
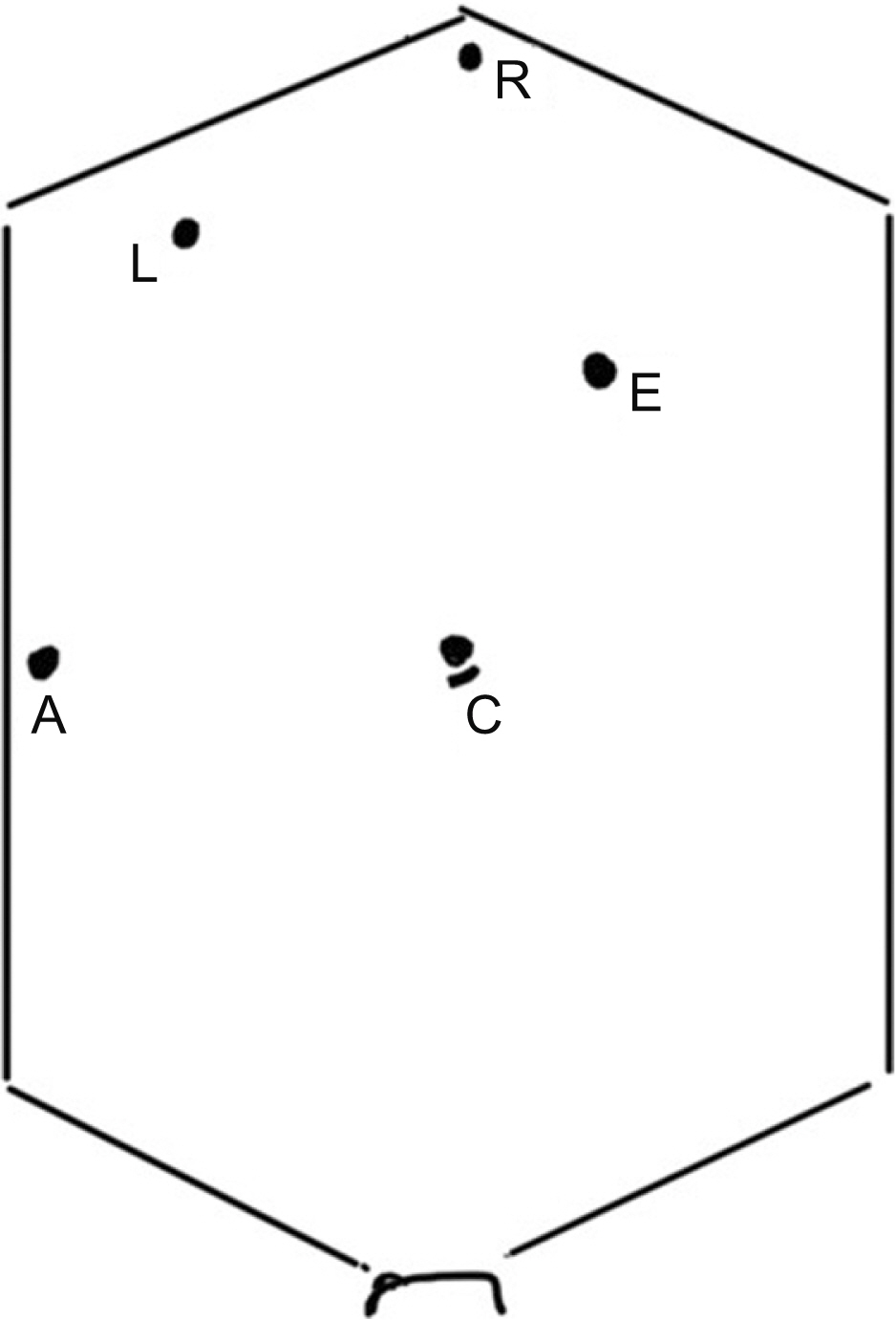
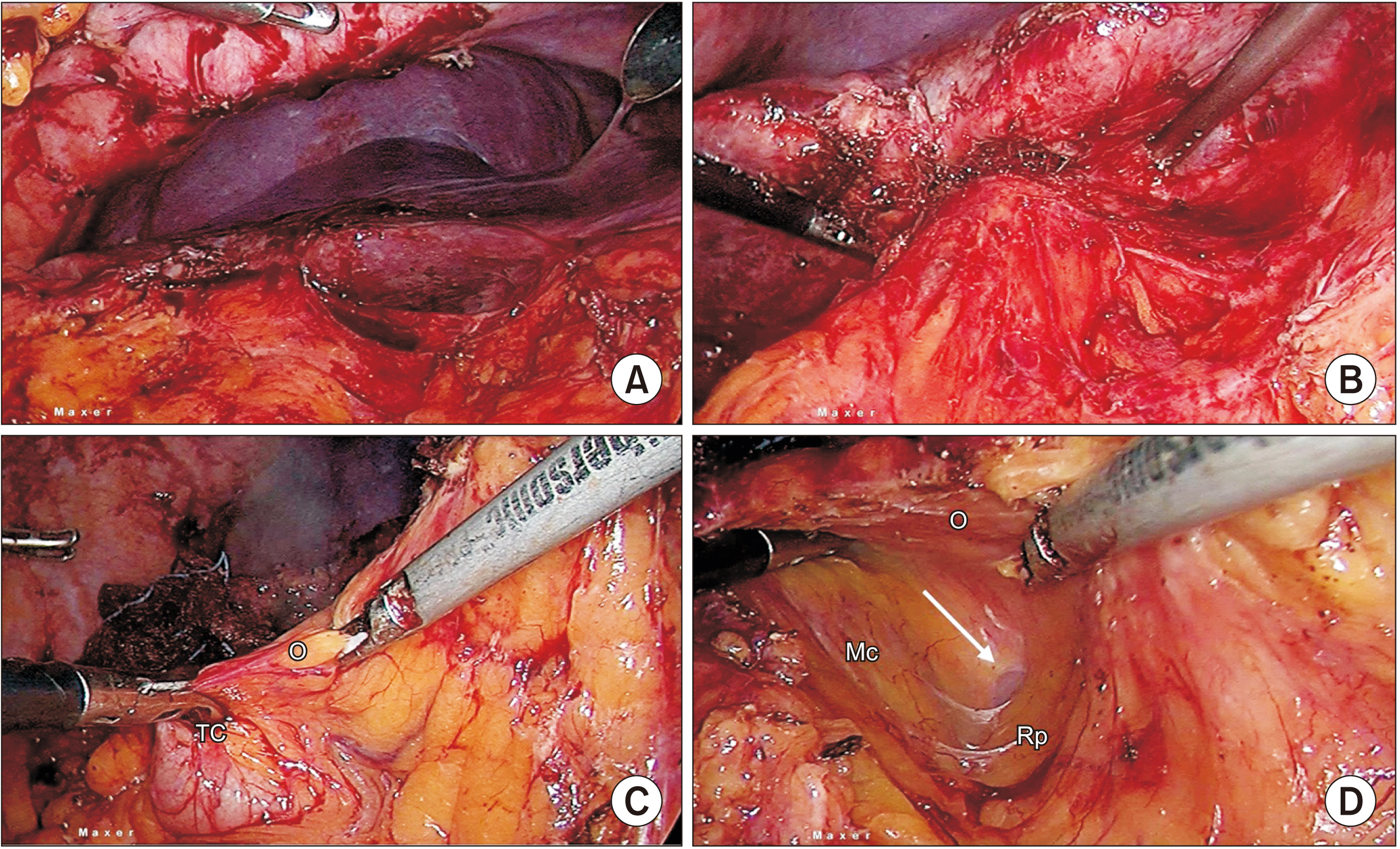
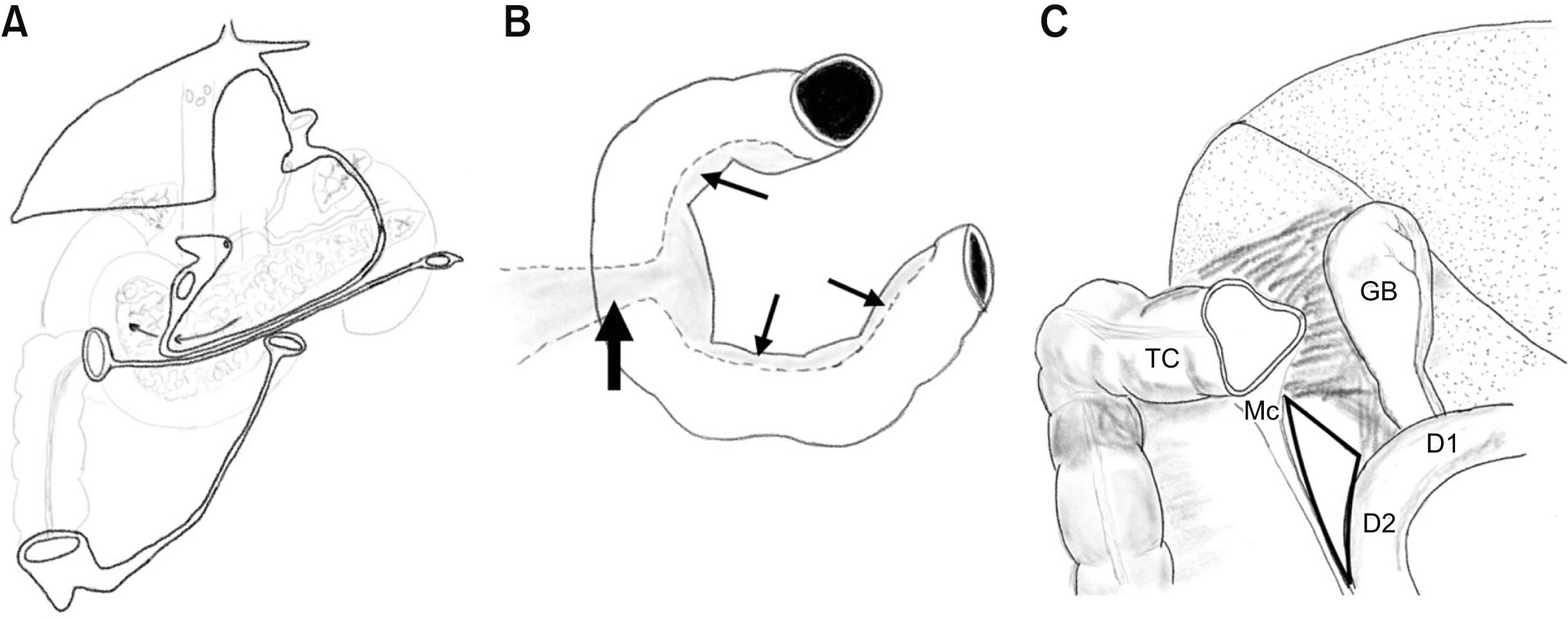
Laparoscopic ‘D2 first’ approach for obscure gallbladders
- Affiliations
-
- 1Department of Surgical Gastroenterology and MIS, Sahasra Hospitals, Bangalore, India
- KMID: 2523057
- DOI: http://doi.org/10.14701/ahbps.2021.25.4.523
Abstract
- Laparoscopic cholecystectomy has a reported incidence of 4%–15% of conversion to an open procedure and one of the main reasons behind the conversion is a gallbladder (GB) wrapped with dense adhesions. It is prudent to convert the procedure to an open operation in patients with particularly dense adhesions when the GB is not visible, preventing safe dissection which carries a potential risk of duodenal or colonic injury. The technique described, namely laparoscopic ‘D2 first’ approach, enables the completion of laparoscopic procedure in patients with ‘obscure’ GBs.
Figure
Reference
-
1. Kala S, Verma S, Dutta G. 2014; Difficult situations in laparoscopic cholecystectomy: a multicentric retrospective study. Surg Laparosc Endosc Percutan Tech. 24:484–487. DOI: 10.1097/SLE.0b013e31829cebd8. PMID: 24710259.2. Sugrue M, Coccolini F, Bucholc M, Johnston A. 2019; Intra-operative gallbladder scoring predicts conversion of laparoscopic to open cholecystectomy: a WSES prospective collaborative study. World J Emerg Surg. 14:12. DOI: 10.1186/s13017-019-0230-9. PMID: 30911325. PMCID: PMC6417130.
Article3. Genc V, Sulaimanov M, Cipe G, Basceken SI, Erverdi N, Gurel M, et al. 2011; What necessitates the conversion to open cholecystectomy? A retrospective analysis of 5164 consecutive laparoscopic operations. Clinics (Sao Paulo). 66:417–420. DOI: 10.1590/S1807-59322011000300009. PMID: 21552665. PMCID: PMC3072001.
Article4. Santos BF, Brunt LM, Pucci MJ. 2017; The difficult gallbladder: a safe approach to a dangerous problem. J Laparoendosc Adv Surg Tech A. 27:571–578. DOI: 10.1089/lap.2017.0038. PMID: 28350258.
Article5. Abelson JS, Afaneh C, Rich BS, Dakin G, Zarnegar R, Fahey TJ 3rd, et al. 2015; Advanced laparoscopic fellowship training decreases conversion rates during laparoscopic cholecystectomy for acute biliary diseases: a retrospective cohort study. Int J Surg. 13:221–226. DOI: 10.1016/j.ijsu.2014.12.016. PMID: 25511478.
Article6. Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). The SAGES safe cholecystectomy program - strategies for minimizing bile duct injuries: adopting a universal culture of safety in cholecystectomy [Internet]. Available from: http://www.sages.org/safe-cholecystectomy-program/. Los Angeles: Society of American Gastrointestinal and Endoscopic Surgeons;2014. cited 2021 May 22.7. Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. 2016; Subtotal cholecystectomy-"fenestrating" vs "reconstituting" subtypes and the prevention of bile duct injury: definition of the optimal procedure in difficult operative conditions. J Am Coll Surg. 222:89–96. DOI: 10.1016/j.jamcollsurg.2015.09.019. PMID: 26521077.8. Cengiz Y, Dalenbäck J, Edlund G, Israelsson LA, Jänes A, Möller M, et al. 2010; Improved outcome after laparoscopic cholecystectomy with ultrasonic dissection: a randomized multicenter trial. Surg Endosc. 24:624–630. DOI: 10.1007/s00464-009-0649-2. PMID: 19688393.
Article9. Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, et al. 2020; Safe cholecystectomy multi-society practice guideline and state of the art consensus conference on prevention of bile duct injury during cholecystectomy. Ann Surg. 272:3–23. DOI: 10.1097/SLA.0000000000003791. PMID: 32404658.10. Osayi SN, Wendling MR, Drosdeck JM, Chaudhry UI, Perry KA, Noria SF, et al. 2015; Near-infrared fluorescent cholangiography facilitates identification of biliary anatomy during laparoscopic cholecystectomy. Surg Endosc. 29:368–375. DOI: 10.1007/s00464-014-3677-5. PMID: 24986018. PMCID: PMC4415528.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic subtotal cholecystectomy in difficult gallbladder: Our experience in a tertiary care center
- Hemorrhagic Small Bowel Tumor Diagnosed with Using Capsule Endoscopy and It was Treated with Laparoscopic Surgery: Report of a Case
- Comparison of totally laparoscopic and laparoscopic-assisted approach in gastrectomy with D2 lymphadenectomy for advanced gastric cancer after neoadjuvant chemotherapy: a retrospective comparative study
- Short-term Surgical Outcomes after Laparoscopic D2 Lymphadenectomy in Patients with Distal Gastric Cancer
- The Laparoscopic Approach for Gastric Remnant Cancer