Ann Hepatobiliary Pancreat Surg.
2024 May;28(2):214-219. 10.14701/ahbps.23-168.
Laparoscopic subtotal cholecystectomy in difficult gallbladder: Our experience in a tertiary care center
- Affiliations
-
- 1Department of Surgical Gastroenterology and HPB Unit, National Institute of Medical Sciences and Research, NIMS University, Jaipur, India
- KMID: 2555931
- DOI: http://doi.org/10.14701/ahbps.23-168
Abstract
- Backgrounds/Aims
Open cholecystectomy is becoming obsolete and laparoscopic cholecystectomy has become the treatment of choice in gallstone diseases. Difficult gallbladders are encountered whenever there is a frozen calot’s triangle, obliterated cystic plate, or both. Rather than converting to open procedure, there has been a growing preference for laparoscopic subtotal cholecystectomy (LSC) during difficult gallbladders. This study aimed to assess the advantages, indications, and viability of LSC in difficult gallbladders.
Methods
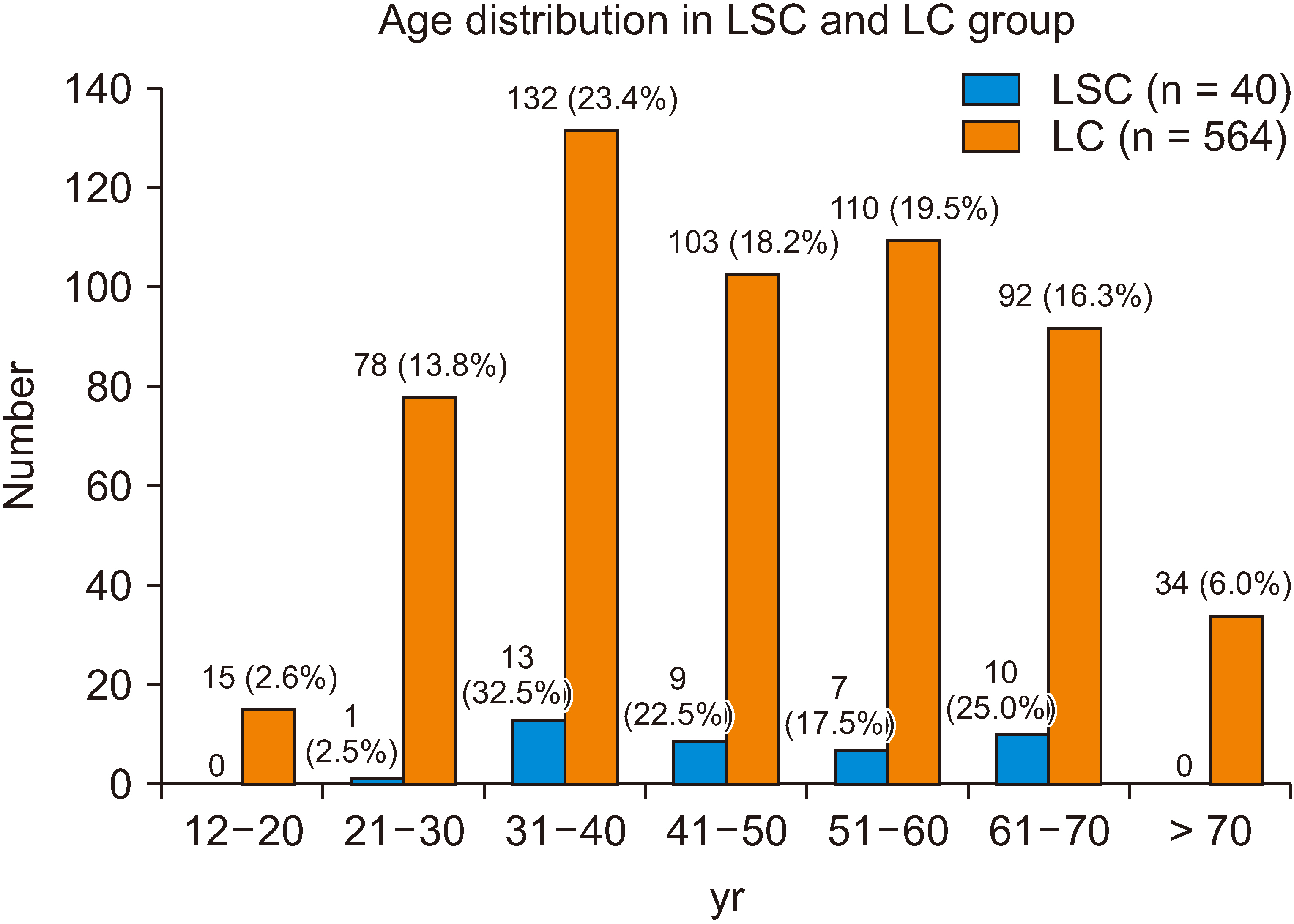
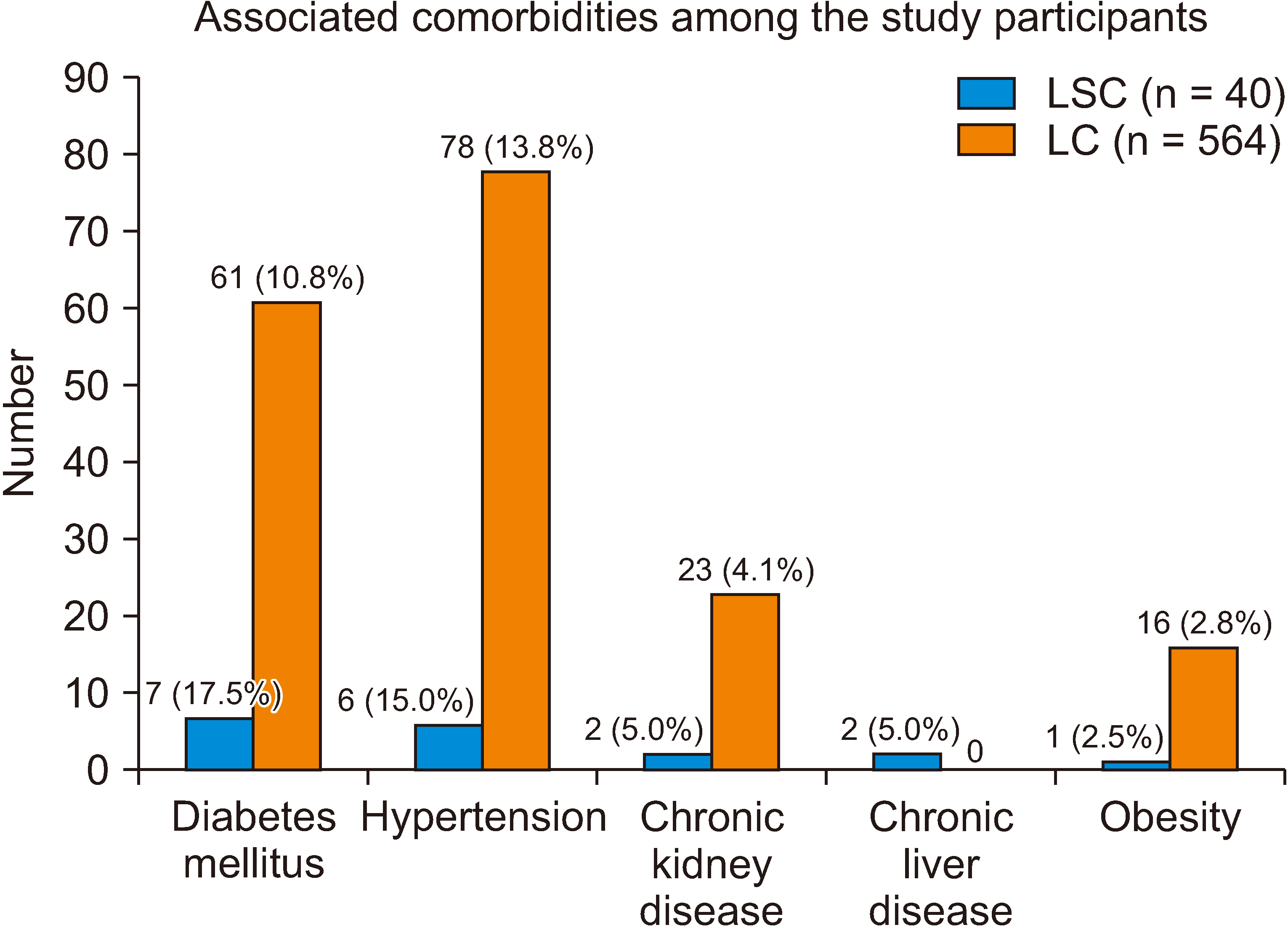
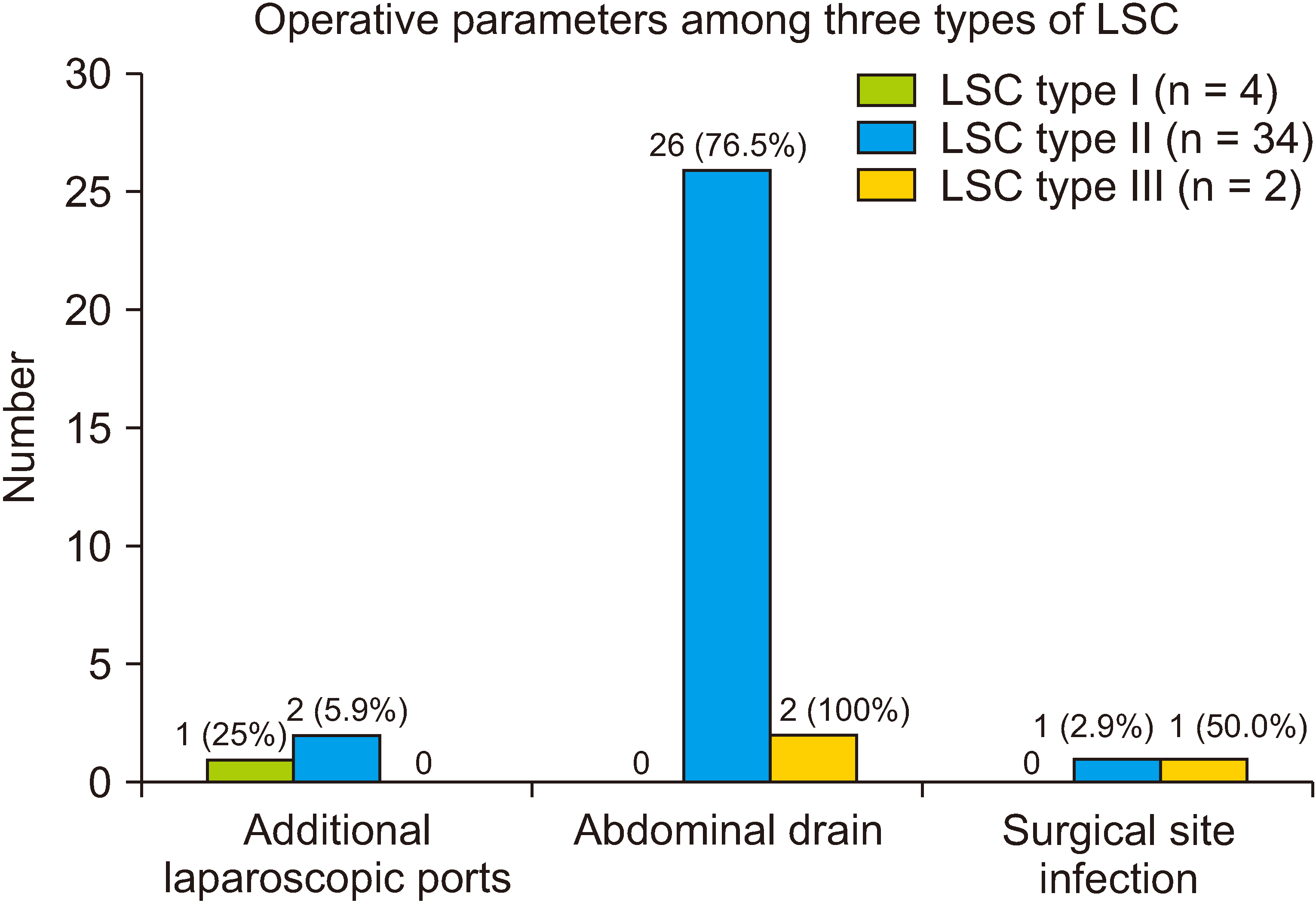
The study included patients undergoing laparoscopic cholecystectomy in NIMS Hospital, Jaipur, from January 2021 to January 2023. Data of the patients who underwent LSC for difficult gallbladders included demographics, comorbidities, operative time, conversion to open cholecystectomy, length of hospital stay, and complications. LSC was classified into three types depending on the part of the gallbladder remnant.
Results
A total of 728 patients underwent laparoscopic cholecystectomy. Among them, 41 patients (5.6%) were attempted for LSC. However, one patient was converted to an open procedure and the rest 40 underwent LSC. LSC was divided into 3 types, 4 patients underwent LSC type I, 34 patients underwent type II, and 2 patients type III. The average operating time and postoperative length of hospital stay were 86.2 minutes and 2.1 days, respectively. Two patients had surgical site infection. No patient had a bile leak and none required intensive care unit care.
Conclusions
LSC is a safe and feasible option for use in difficult gallbladders.
Keyword
Figure
Cited by 1 articles
-
Usefulness of intraoperative choledochoscopy in laparoscopic subtotal cholecystectomy for severe cholecystitis
Rui-Hui Zhang, Xiang-Nan Wang, Yue-Feng Ma, Xue-Qian Tang, Mei-Ju Lin, Li-Jun Shi, Jing-Yi Li, Hong-Wei Zhang
Ann Hepatobiliary Pancreat Surg. 2025;29(2):192-198. doi: 10.14701/ahbps.25-010.
Reference
-
References
1. Unisa S, Jagannath P, Dhir V, Khandelwal C, Sarangi L, Roy TK. 2011; Population-based study to estimate the prevalence and determine risk factors of gallbladder diseases in the rural Gangetic basin of North India. HPB (Oxford). 13:117–125. DOI: 10.1111/j.1477-2574.2010.00255.x. PMID: 21241429. PMCID: PMC3044346.
Article2. Unisa S, Jagannath P, Dhir V, Khandelwal C, Sarangi L, Roy TK. 2011; Population-based study to estimate the prevalence and determine risk factors of gallbladder diseases in the rural Gangetic basin of North India. HPB (Oxford). 13:117–125.
Article3. Elshaer M, Gravante G, Thomas K, Sorge R, Al-Hamali S, Ebdewi H. 2015; Subtotal cholecystectomy for "difficult gallbladders": systematic review and meta-analysis. JAMA Surg. 150:159–168. DOI: 10.1001/jamasurg.2014.1219. PMID: 25548894.
Article4. Salky BA, Edye MB. 1998; The difficult cholecystectomy: problems related to concomitant diseases. Semin Laparosc Surg. 5:107–114. DOI: 10.1177/155335069800500205. PMID: 9594037.
Article5. Laws HL. 1998; The difficult cholecystectomy: problems during dissection and extraction. Semin Laparosc Surg. 5:81–91. DOI: 10.1177/155335069800500203. PMID: 9594035.
Article6. Gode D, Palanivelu C, Syed ZQ. 2014; New variants of laparoscopic subtotal cholecystectomy in management of acute cholecystitis. Int J Med Sci Public Health. 3:397–400. DOI: 10.5455/ijmsph.2014.300120141.
Article7. Henneman D, da Costa DW, Vrouenraets BC, van Wagensveld BA, Lagarde SM. 2013; Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review. Surg Endosc. 27:351–358. DOI: 10.1007/s00464-012-2458-2. PMID: 22806521.
Article8. Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. 1993; Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 165:9–14. DOI: 10.1016/S0002-9610(05)80397-6. PMID: 8418705.
Article9. Strasberg SM. 2008; Error traps and vascular-biliary injury in laparoscopic and open cholecystectomy. J Hepatobiliary Pancreat Surg. 15:284–292. DOI: 10.1007/s00534-007-1267-9. PMID: 18535766.
Article10. Törnqvist B, Waage A, Zheng Z, Ye W, Nilsson M. 2016; Severity of acute cholecystitis and risk of iatrogenic bile duct injury during cholecystectomy, a population-based case-control study. World J Surg. 40:1060–1067. DOI: 10.1007/s00268-015-3365-1. PMID: 26669783.
Article11. Henneman D, da Costa DW, Vrouenraets BC, van Wagensveld BA, Lagarde SM. 2013; Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review. Surg Endosc. 27:351–358. DOI: 10.1007/s00464-012-2458-2. PMID: 22806521.
Article12. Boyd K, Bradley NA, Cannings E, Shearer C, Wadhawan H, Wilson MSJ, et al. 2022; Laparoscopic subtotal cholecystectomy; change in practice over a 10-year period. HPB (Oxford). 24:759–763. DOI: 10.1016/j.hpb.2021.10.003. PMID: 34776369.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Squamous Cell Carcinoma of Gallbladder after Laparoscopic Cholecystectomy
- Chinical Comparison of the Traditional Versus Laparoscopic Surgery in Cholecystectomy for Cholelithiasis
- Necrotizing Gallbladder Torsion Masking as Acalculous Cholecystitis: A Review of Two Cases Treated with Successful Laparoscopic Cholecystectomy
- A case of porcelain gallbladder
- Usefulness of intraoperative choledochoscopy in laparoscopic subtotal cholecystectomy for severe cholecystitis