Ann Hepatobiliary Pancreat Surg.
2025 May;29(2):192-198. 10.14701/ahbps.25-010.
Usefulness of intraoperative choledochoscopy in laparoscopic subtotal cholecystectomy for severe cholecystitis
- Affiliations
-
- 1Department of Biliary Minimally Invasive Surgery, Affiliated Zhongshan Hospital of Dalian University, Dalian, China
- KMID: 2568268
- DOI: http://doi.org/10.14701/ahbps.25-010
Abstract
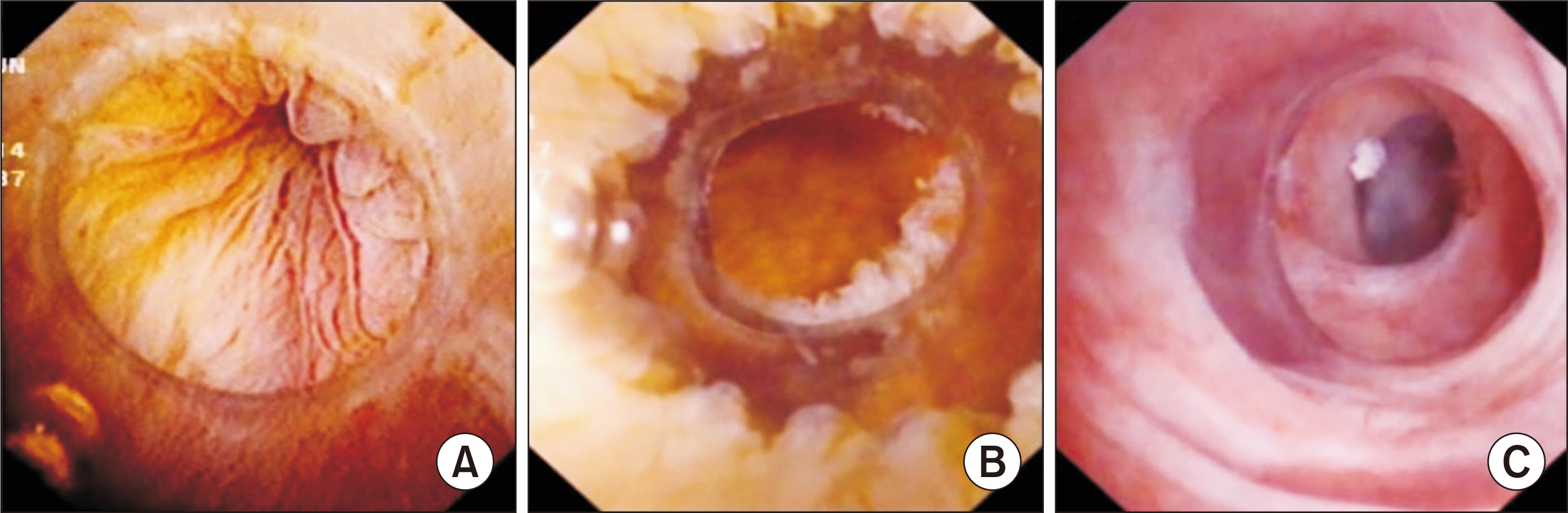
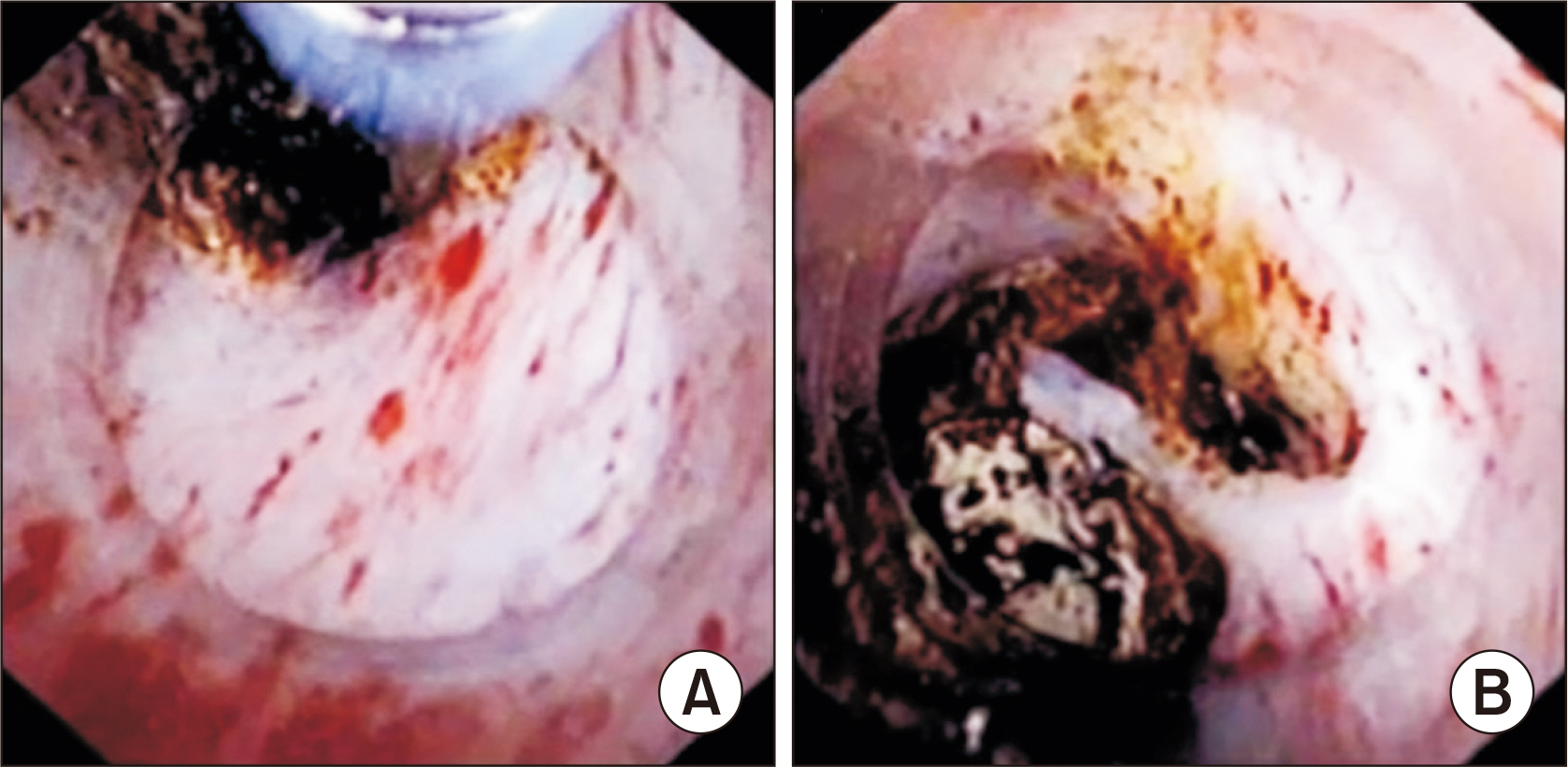
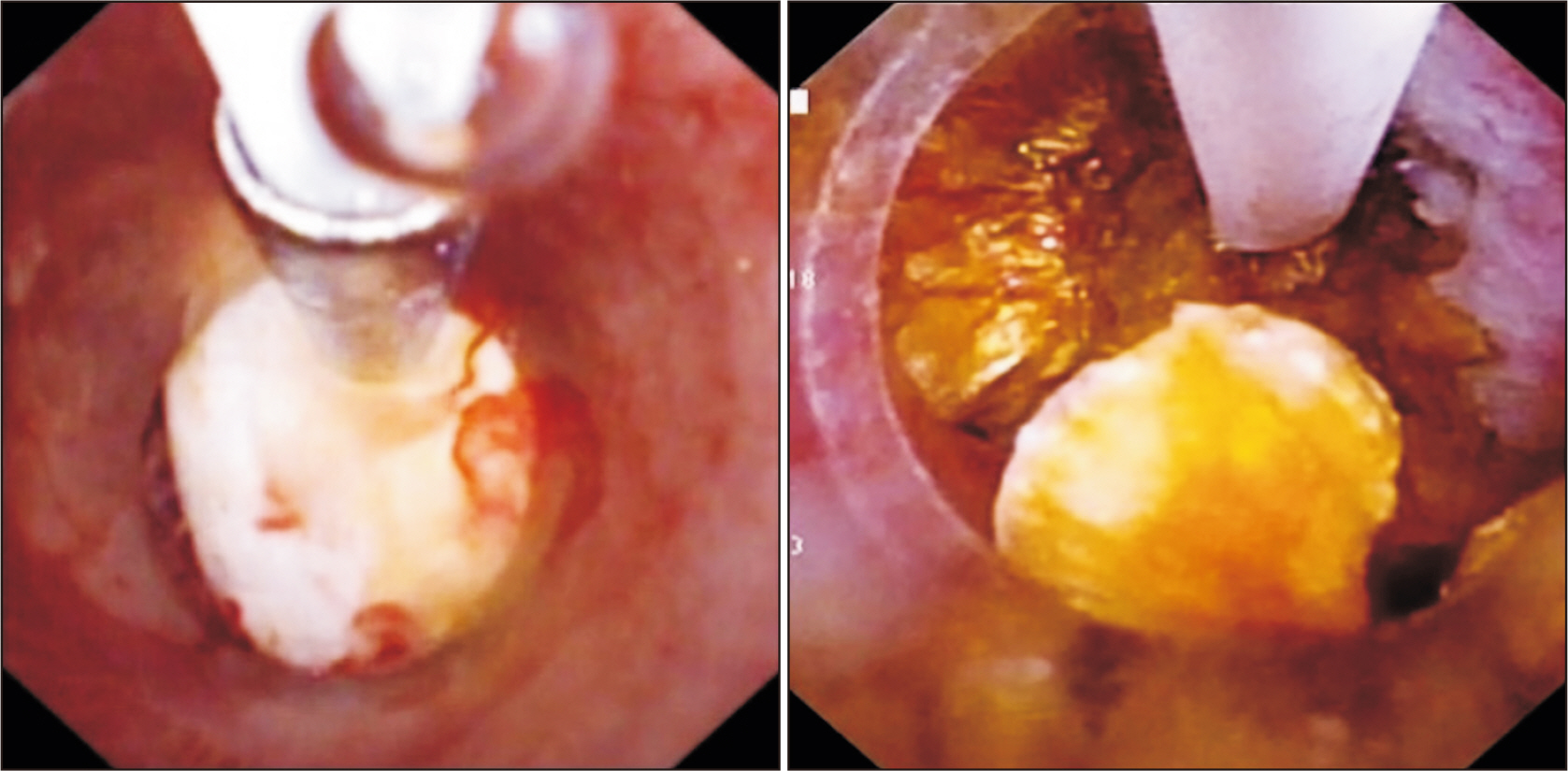
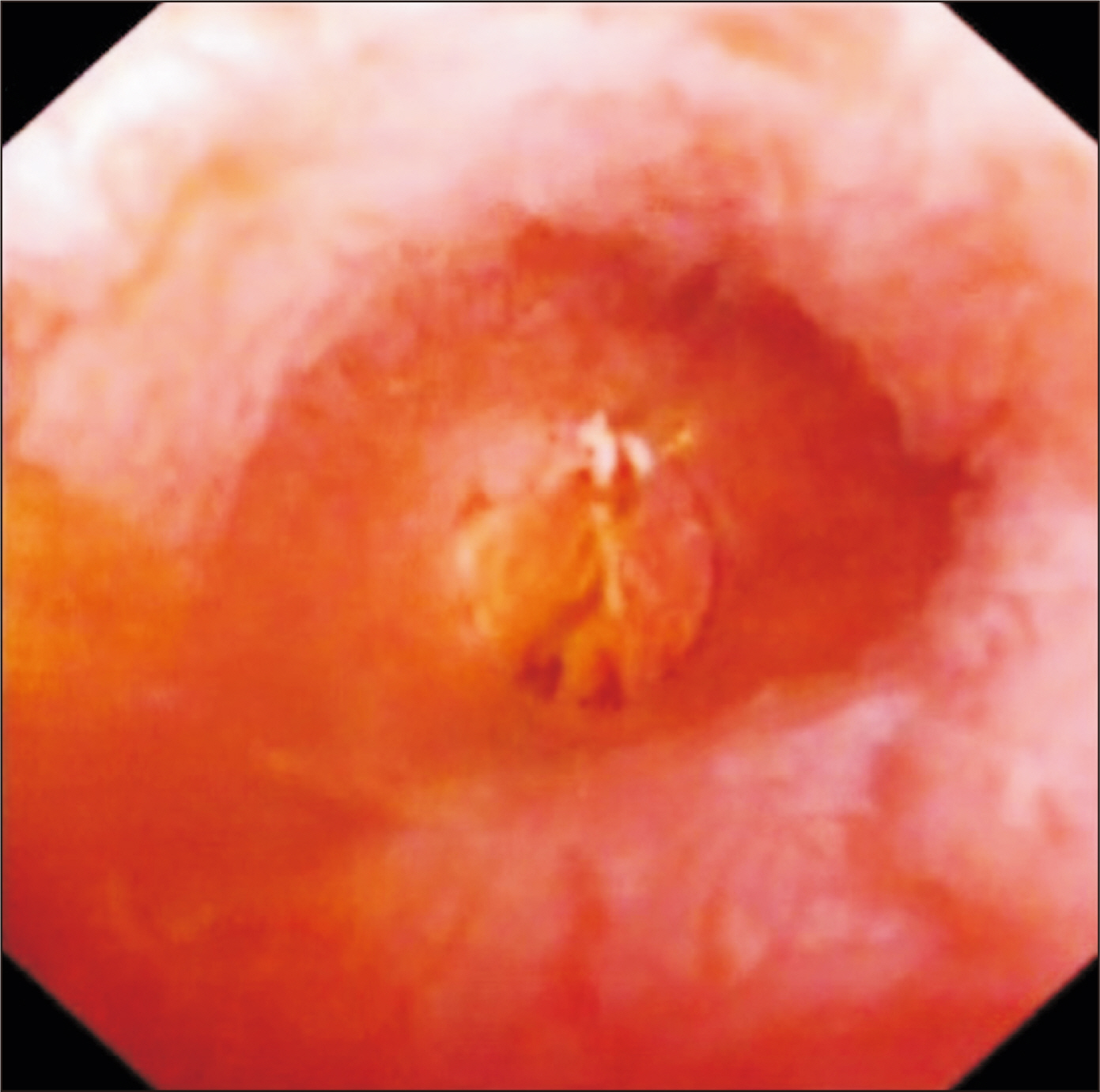
- Laparoscopic subtotal cholecystectomy (LSC) has been a safe and viable alternative to conversion to laparotomy in cases of severe cholecystitis. The objective of this study is to determine the utility of intraoperative choledochoscopy in LSC for the exploration of the gallbladder, cyst duct, and subsequent stone clearance of the cystic duct in cases of severe cholecystitis. A total of 72 patients diagnosed with severe cholecystitis received choledochoscopy-assisted laparoscopic subtotal cholecystectomy (CALSC). A choledochoscopy was performed to explore the gallbladder cavity and/or cystic duct, and to extract stones using a range of techniques. The clinical records, including the operative records and outcomes, were subjected to analysis. No LSC was converted to open surgery, and no bile duct or vascular injuries were sustained. All stones within the cystic duct were removed by a combination of techniques, including high-frequency needle knife electrotomy, basket, and electrohydraulic lithotripsy. A follow-up examination revealed the absence of residual bile duct stones, with the exception of one common bile duct stone, which was extracted via endoscopic retrograde cholangiopancreatography. In certain special cases, CALSC may prove to be an efficacious treatment for the management of severe cholecystitis. This technique allows for optimal comprehension of the situation within the gallbladder cavity and cystic duct, facilitating the removal of stones from the cystic duct and reducing the residue of the non-functional gallbladder remnant.
Figure
Reference
-
References
1. Davidoff AM, Pappas TN, Murray EA, Hilleren DJ, Johnson RD, Baker ME, et al. 1992; Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 215:196–202. DOI: 10.1097/00000658-199203000-00002. PMID: 1531913. PMCID: PMC1242421.2. Mercado MA, Chan C, Orozco H, Tielve M, Hinojosa CA. 2003; Acute bile duct injury. The need for a high repair. Surg Endosc. 17:1351–1355. DOI: 10.1007/s00464-002-8705-1. PMID: 12811664.3. Henneman D, da Costa DW, Vrouenraets BC, van Wagensveld BA, Lagarde SM. 2013; Laparoscopic partial cholecystectomy for the difficult gallbladder: a systematic review. Surg Endosc. 27:351–358. DOI: 10.1007/s00464-012-2458-2. PMID: 22806521.
Article4. Ji W, Li LT, Li JS. 2006; Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat Dis Int. 5:584–589.5. Kuwabara J, Watanabe Y, Kameoka K, Horiuchi A, Sato K, Yukumi S, et al. 2014; Usefulness of laparoscopic subtotal cholecystectomy with operative cholangiography for severe cholecystitis. Surg Today. 44:462–465. DOI: 10.1007/s00595-013-0626-1. PMID: 23736889. PMCID: PMC3923106.
Article6. Michalowski K, Bornman PC, Krige JE, Gallagher PJ, Terblanche J. 1998; Laparoscopic subtotal cholecystectomy in patients with complicated acute cholecystitis or fibrosis. Br J Surg. 85:904–906. DOI: 10.1046/j.1365-2168.1998.00749.x. PMID: 9692560.
Article7. Chowbey P, Sharma A, Goswami A, Afaque Y, Najma K, Baijal M, et al. 2015; Residual gallbladder stones after cholecystectomy: a literature review. J Minim Access Surg. 11:223–230. DOI: 10.4103/0972-9941.158156. PMID: 26622110. PMCID: PMC4640007.
Article8. Shingu Y, Komatsu S, Norimizu S, Taguchi Y, Sakamoto E. 2016; Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc. 30:526–531. DOI: 10.1007/s00464-015-4235-5. PMID: 26091984.
Article9. Haldeniya K, R KS, Raghavendra A, Singh PK. 2024; Laparoscopic subtotal cholecystectomy in difficult gallbladder: our experience in a tertiary care center. Ann Hepatobiliary Pancreat Surg. 28:214–219. DOI: 10.14701/ahbps.23-168. PMID: 38409679. PMCID: PMC11128793.
Article10. Gupta V, Sharma AK, Kumar P, Gupta M, Gulati A, Sinha SK, et al. 2019; Residual gall bladder: an emerging disease after safe cholecystectomy. Ann Hepatobiliary Pancreat Surg. 23:353–358. DOI: 10.14701/ahbps.2019.23.4.353. PMID: 31825001. PMCID: PMC6893054.
Article11. Singh A, Kapoor A, Singh RK, Prakash A, Behari A, Kumar A, et al. 2018; Management of residual gall bladder: a 15-year experience from a north Indian tertiary care centre. Ann Hepatobiliary Pancreat Surg. 22:36–41. DOI: 10.14701/ahbps.2018.22.1.36. PMID: 29536054. PMCID: PMC5845609.
Article12. Pernice LM, Andreoli F. 2009; Laparoscopic treatment of stone recurrence in a gallbladder remnant: report of an additional case and literature review. J Gastrointest Surg. 13:2084–2091. DOI: 10.1007/s11605-009-0913-8. PMID: 19415394.
Article13. Supit C, Supit T, Mazni Y, Basir I. 2017; The outcome of laparoscopic subtotal cholecystectomy in difficult cases - a case series. Int J Surg Case Rep. 41:311–314. DOI: 10.1016/j.ijscr.2017.10.054. PMID: 29132116. PMCID: PMC5684444.
Article14. Quoraishi S, Ahmed J, Ponsford A, Rasheed A. 2017; Lessons learnt from a case of extracorporeal shockwave lithotripsy for a residual gallbladder stone. Int J Surg Case Rep. 32:43–46. DOI: 10.1016/j.ijscr.2017.02.001. PMID: 28235649. PMCID: PMC5322175.
Article15. Kim Y, Wima K, Jung AD, Martin GE, Dhar VK, Shah SA. 2017; Laparoscopic subtotal cholecystectomy compared to total cholecystectomy: a matched national analysis. J Surg Res. 218:316–321. DOI: 10.1016/j.jss.2017.06.047. PMID: 28985867.
Article16. Shin M, Choi N, Yoo Y, Kim Y, Kim S, Mun S. 2016; Clinical outcomes of subtotal cholecystectomy performed for difficult cholecystectomy. Ann Surg Treat Res. 91:226–232. DOI: 10.4174/astr.2016.91.5.226. PMID: 27847794. PMCID: PMC5107416.
Article17. Jara G, Rosciano J, Barrios W, Vegas L, Rodríguez O, Sánchez R, et al. 2017; Laparoscopic subtotal cholecystectomy: a surgical alternative to reduce complications in complex cases. Cir Esp. 95:465–470. DOI: 10.1016/j.ciresp.2017.07.013. PMID: 28918963.
Article18. van Dijk AH, Donkervoort SC, Lameris W, de Vries E, Eijsbouts QAJ, Vrouenraets BC, et al. 2017; Short- and long-term outcomes after a reconstituting and fenestrating subtotal cholecystectomy. J Am Coll Surg. 225:371–379. DOI: 10.1016/j.jamcollsurg.2017.05.016. PMID: 28606484.
Article19. Slater M, Midya S, Booth M. 2021; Re-interventions and re-admissions in a 13-year series following use of laparoscopic subtotal cholecystectomy. J Minim Access Surg. 17:28–31. DOI: 10.4103/jmas.JMAS_124_19. PMID: 31571673. PMCID: PMC7945629.
Article20. Hubert C, Annet L, van Beers BE, Gigot JF. 2010; The "inside approach of the gallbladder" is an alternative to the classic Calot's triangle dissection for a safe operation in severe cholecystitis. Surg Endosc. 24:2626–2632. DOI: 10.1007/s00464-010-0966-5. PMID: 20336321.
Article21. Segal MS, Huynh RH, Wright GO. 2017; case report: modified laparoscopic subtotal cholecystectomy: an alternative approach to the "difficult gallbladder". Am J Case Rep. 18:186–189. DOI: 10.12659/AJCR.900646. PMID: 28220035. PMCID: PMC5331888.
Article22. Matsumura T, Komatsu S, Komaya K, Ando K, Arikawa T, Ishiguro S, et al. 2018; Closure of the cystic duct orifice in laparoscopic subtotal cholecystectomy for severe cholecystitis. Asian J Endosc Surg. 11:206–211. DOI: 10.1111/ases.12449. PMID: 29235252.
Article23. Hashimoto M, Matsuda M, Watanabe G. 2010; Intraoperative ultrasonography for reducing bile duct injury during laparoscopic cholecystectomy. Hepatogastroenterology. 57:706–709.24. Elshaer M, Gravante G, Thomas K, Sorge R, Al-Hamali S, Ebdewi H. 2015; Subtotal cholecystectomy for "difficult gallbladders": systematic review and meta-analysis. JAMA Surg. 150:159–68. DOI: 10.1001/jamasurg.2014.1219. PMID: 25548894.
Article25. Navaratne L, Al-Musawi J, Mérida AA, Vilaça J, Isla AM. 2018; Trans-infundibular choledochoscopy: a method for accessing the common bile duct in complex cases. Langenbecks Arch Surg. 403:777–783. DOI: 10.1007/s00423-018-1698-6. PMID: 30058037.
Article26. Yang YL, Zhang C, Wu P, Ma YF, Li JY, Zhang HW, et al. 2016; Choledochoscopic high-frequency needle-knife electrotomy for treatment of anastomotic strictures after Roux-en-Y hepaticojejunostomy. BMC Gastroenterol. 16:54. DOI: 10.1186/s12876-016-0465-9. PMID: 27153771. PMCID: PMC4858855.
Article27. Yang YL, Zhang C, Zhao G, Wu P, Ma YF, Zhang HW, et al. 2015; Choledochoscopic high-frequency needle-knife electrotomy as an effective treatment for intrahepatic biliary strictures. J Gastroenterol Hepatol. 30:1438–1443. DOI: 10.1111/jgh.12951. PMID: 25765565.
Article28. Santos BF, Brunt LM, Pucci MJ. 2017; The difficult gallbladder: a safe approach to a dangerous problem. J Laparoendosc Adv Surg Tech A. 27:571–578. DOI: 10.1089/lap.2017.0038. PMID: 28350258.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy
- The Comparative Analysis of Therapeutic Results between a Laparoscopic Cholecystectomy and an Open cholecystectomy in Acute Cholecystitis
- Usefulness of Preoperative Percutaneous Transhepatic GB Drainge on Laparoscopic Cholecystectomy in Patients with Acute Cholecystitis
- Laparoscopic cholecystectomy for acute cholecystitis: Any time is a good time
- The Meaning of Open Cholecystectomy for Acute Cholecystitis