Ann Hepatobiliary Pancreat Surg.
2023 Aug;27(3):271-276. 10.14701/ahbps.22-127.
Laparoscopic cholecystectomy for acute cholecystitis: Any time is a good time
- Affiliations
-
- 1Department of Surgical Gastroenterology, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India
- 2Department of Surgical Gastroenterology, Apollo Hospitals, Bhubaneswar, Odisha, India
- KMID: 2545721
- DOI: http://doi.org/10.14701/ahbps.22-127
Abstract
- Backgrounds/Aims
Laparoscopic cholecystectomy within one week of acute cholecystitis is considered safe and advantageous. Surgery beyond first week is reserved for non-resolving attack or complications. To compare clinical outcomes of patients undergoing laparoscopic cholecystectomy in the first week and between two to six weeks of an attack of acute cholecystitis.
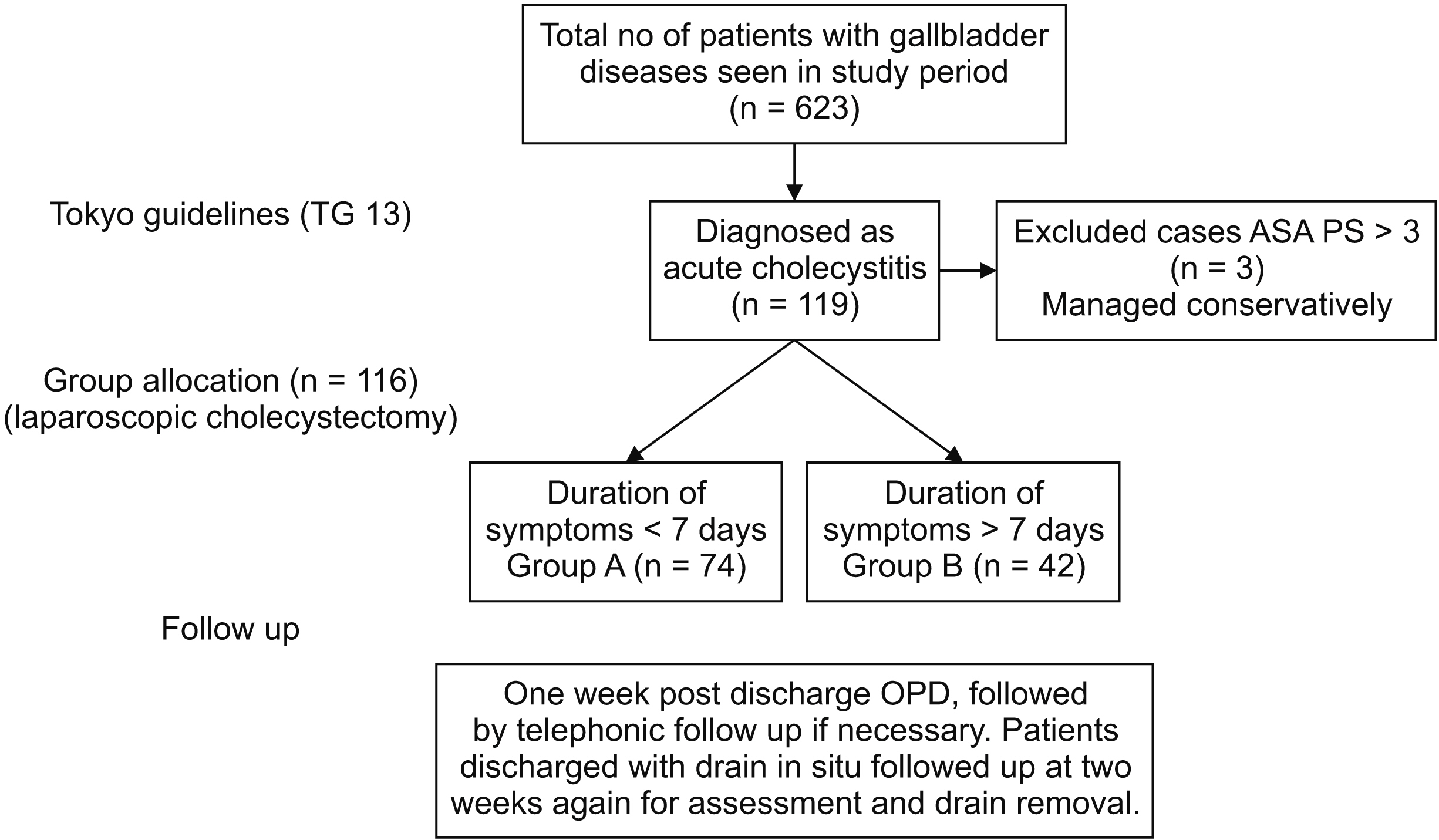
Methods
In an analysis of a prospectively maintained database, all patients who underwent laparoscopic cholecystectomy for acute cholecystitis were divided into two groups: group A, operated within one week; and group B, operated between two to six weeks of an attack. Main variables studied were mean operative time, conversion to open cholecystectomy, morbidity profile, and duration of hospital stay.
Results
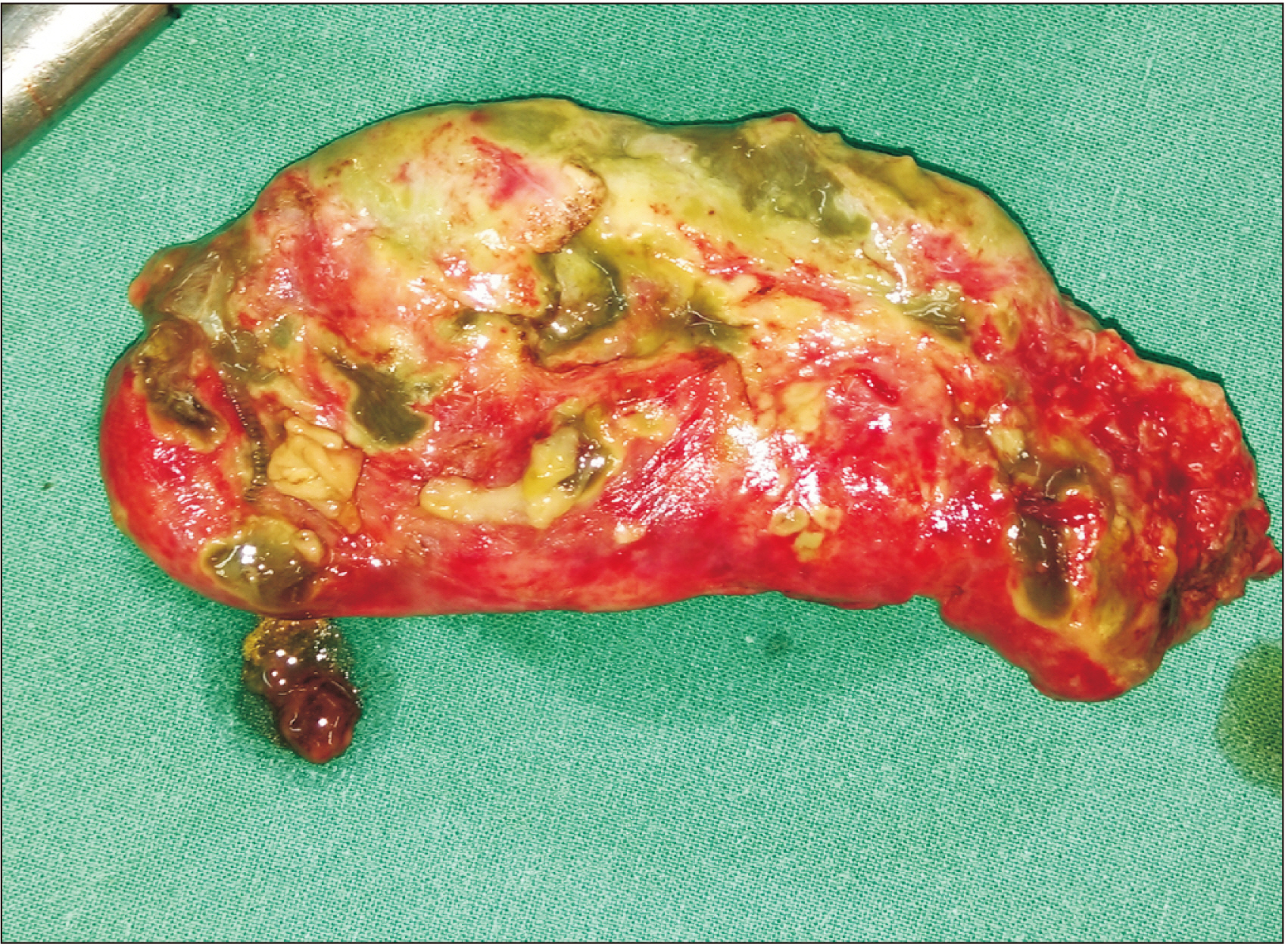
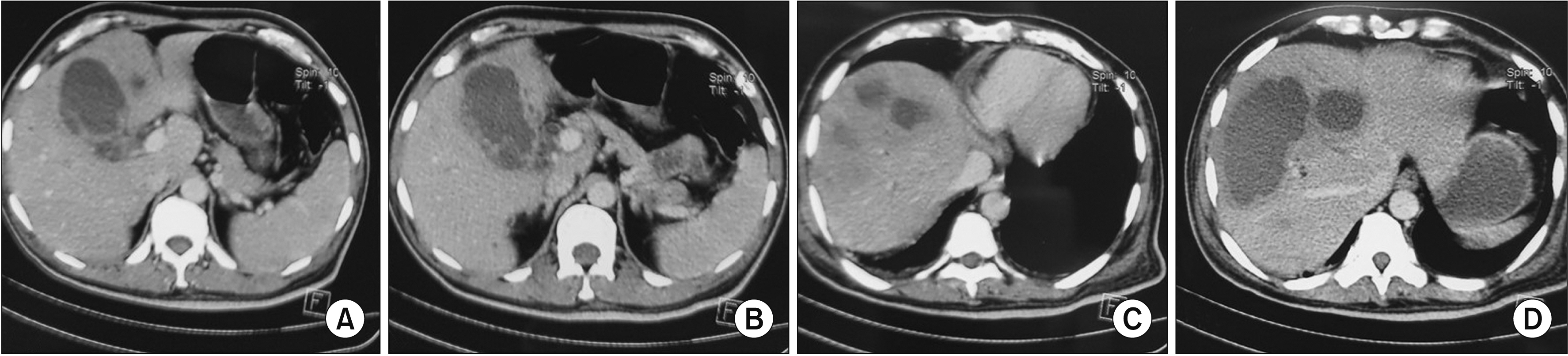
A total of 116 patients (74 in group A and 42 in group B) were included. Mean interval between onset of symptoms & surgery was five days (range, 1–7 days) in group A and 12 days (range, 8–20 days) in group B. Operative time and incidence of subtotal cholecystectomy were higher in group B (statistically not significant). Mean postoperative stay was 2 days in group A and 3 days in group B. Laparoscopy was converted to open cholecystectomy in two patients in each group. There was no incidence of biliary injury. One patient in group B died during the postoperative period due to continued sepsis and multiorgan failure.
Conclusions
In tertiary care setting, with adequate surgical expertise, laparoscopic cholecystectomy can be safely performed in patients with acute cholecystitis irrespective of the time of presentation.
Figure
Cited by 1 articles
-
Comparison between percutaneous transhepatic gallbladder drainage and upfront laparoscopic cholecystectomy in patients with moderate-to-severe acute cholecystitis: a propensity score-matched analysis
Okjoo Lee, Yong Chan Shin, Youngju Ryu, So Jeong Yoon, Hongbeom Kim, Sang Hyun Shin, Jin Seok Heo, Woohyun Jung, Chang-Sup Lim, In Woong Han
Ann Surg Treat Res. 2023;105(5):310-318. doi: 10.4174/astr.2023.105.5.310.
Reference
-
1. The role of laparoscopic cholecystectomy (L.C.). 1993; Guidelines for clinical application. Society of American Gastrointestinal Endoscopic Surgeons (SAGES). Surg Endosc. 7:369–370. DOI: 10.1007/BF00725963. PMID: 8351617.2. Catena F, Ansaloni L, Bianchi E, Di Saverio S, Coccolini F, Vallicelli C, et al. 2013; The ACTIVE (Acute Cholecystitis Trial Invasive Versus Endoscopic) Study: multicenter randomized, double-blind, controlled trial of laparoscopic versus open surgery for acute cholecystitis. Hepatogastroenterology. 60:1552–1556. PMID: 24634923.3. Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Syst Rev. 2013; (6):CD005440. DOI: 10.1002/14651858.CD005440.pub3. PMID: 23813477.4. Banz V, Gsponer T, Candinas D, Güller U. 2011; Population-based analysis of 4113 patients with acute cholecystitis: defining the optimal time-point for laparoscopic cholecystectomy. Ann Surg. 254:964–970. DOI: 10.1097/SLA.0b013e318228d31c. PMID: 21817893.5. Gutt CN, Encke J, Köninger J, Harnoss JC, Weigand K, Kipfmüller K, et al. 2013; Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg. 258:385–393. DOI: 10.1097/SLA.0b013e3182a1599b. PMID: 24022431.6. Jensen KK, Roth NO, Krarup PM, Bardram L. 2019; Surgical management of acute cholecystitis in a nationwide Danish cohort. Langenbecks Arch Surg. 404:589–597. DOI: 10.1007/s00423-019-01802-0. PMID: 31297607.7. Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018; 25:55–72. Erratum in: J Hepatobiliary Pancreat Sci 2019;26:534. DOI: 10.1002/jhbp.516. PMID: 29045062.8. Ansaloni L, Pisano M, Coccolini F, Peitzmann AB, Fingerhut A, Catena F, et al. 2016; 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg. 11:25. Erratum in: World J Emerg Surg 2016;11:52. DOI: 10.1186/s13017-016-0088-z. PMID: 27822294. PMCID: PMC5097400.9. Hirota M, Takada T, Kawarada Y, Nimura Y, Miura F, Hirata K, et al. 2007; Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 14:78–82. DOI: 10.1007/s00534-006-1159-4. PMID: 17252300. PMCID: PMC2784516.10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. 1987; A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40:373–383. DOI: 10.1016/0021-9681(87)90171-8. PMID: 3558716.11. American Society of Anesthesiologists (ASA). ASA physical status classification system [Internet]. Available from: https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system. American Society of Anesthesiologists;2014. cited 2023 Jan 1.12. Strasberg SM, Hertl M, Soper NJ. 1995; An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 180:101–125. PMID: 8000648.13. Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. 2016; Subtotal cholecystectomy-"fenestrating" vs "reconstituting" subtypes and the prevention of bile duct injury: definition of the optimal procedure in difficult operative conditions. J Am Coll Surg. 222:89–96. DOI: 10.1016/j.jamcollsurg.2015.09.019. PMID: 26521077.14. Senapati PS, Bhattarcharya D, Harinath G, Ammori BJ. 2003; A survey of the timing and approach to the surgical management of cholelithiasis in patients with acute biliary pancreatitis and acute cholecystitis in the UK. Ann R Coll Surg Engl. 85:306–312. DOI: 10.1308/003588403769162404. PMID: 14594533. PMCID: PMC1964333.15. Livingston EH, Rege RV. 2004; A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg. 188:205–211. DOI: 10.1016/j.amjsurg.2004.06.013. PMID: 15450821.16. Navez B, Ungureanu F, Michiels M, Claeys D, Muysoms F, Hubert C, et al. 2012; Surgical management of acute cholecystitis: results of a 2-year prospective multicenter survey in Belgium. Surg Endosc. 26:2436–2445. DOI: 10.1007/s00464-012-2206-7. PMID: 22407152.17. Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR. 2010; Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. 97:141–150. Erratum in: Br J Surg 2010;97:624. DOI: 10.1002/bjs.6870. PMID: 20035546.18. Hartwig W, Büchler MW. 2014; Acute cholecystitis: early versus delayed surgery. Adv Surg. 48:155–164. DOI: 10.1016/j.yasu.2014.05.008. PMID: 25293613.19. Nassar AHM, Ng HJ, Wysocki AP, Khan KS, Gil IC. 2021; Achieving the critical view of safety in the difficult laparoscopic cholecystectomy: a prospective study of predictors of failure. Surg Endosc. 35:6039–6047. DOI: 10.1007/s00464-020-08093-3. PMID: 33067645. PMCID: PMC8523408.20. Sutcliffe RP, Hollyman M, Hodson J, Bonney G, Vohra RS, Griffiths EA. 2016; Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective U.K. database of 8820 patients. HPB (Oxford). 18:922–928. DOI: 10.1016/j.hpb.2016.07.015. PMID: 27591176. PMCID: PMC5094477.21. Hu ASY, Menon R, Gunnarsson R, de Costa A. 2017; Risk factors for conversion of laparoscopic cholecystectomy to open surgery - a systematic literature review of 30 studies. Am J Surg. 214:920–930. DOI: 10.1016/j.amjsurg.2017.07.029. PMID: 28739121.22. Overby DW, Apelgren KN, Richardson W, Fanelli R. 2010; SAGES guidelines for the clinical application of laparoscopic biliary tract surgery. Surg Endosc. 24:2368–2386. DOI: 10.1007/s00464-010-1268-7. PMID: 20706739.23. Tan JK, Goh JC, Lim JW, Shridhar IG, Madhavan K, Kow AW. 2017; Same admission laparoscopic cholecystectomy for acute cholecystitis: is the "golden 72 hours" rule still relevant? HPB (Oxford). 19:47–51. DOI: 10.1016/j.hpb.2016.10.006. PMID: 27825751.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Comparative Analysis of Therapeutic Results between a Laparoscopic Cholecystectomy and an Open cholecystectomy in Acute Cholecystitis
- What is the Optimal Timing for Laparoscopic Cholecystectomy in Acute Cholecystitis
- Laparoscopic Cholecystectomy in the Second Trimester of Pregnancy
- Optimal Time of Laparoscopic Cholecystectomy in Acute Cholecystitis
- Application of Laparoscopic Cholecystectomy in Acute Cholecystitis