Ann Surg Treat Res.
2021 Dec;101(6):360-367. 10.4174/astr.2021.101.6.360.
The impact of Model for End-Stage Liver Disease score on deceased donor liver transplant outcomes in low volume liver transplantation center: a retrospective and singlecenter study
- Affiliations
-
- 1Department of Surgery, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- KMID: 2522935
- DOI: http://doi.org/10.4174/astr.2021.101.6.360
Abstract
- Purpose
In June 2016, the Model for End-Stage Liver Disease (MELD) score was employed in South Korea instead of the Child-Turcotte-Pugh (CTP) score. This study compared the outcomes of deceased donor liver transplantation (DDLT) before and after the MELD system application.
Methods
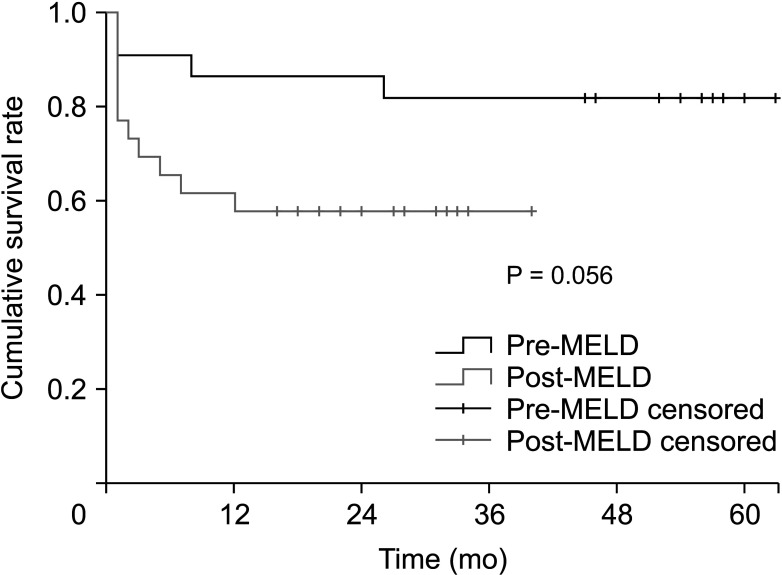
This retrospective study reviewed 48 patients who underwent DDLT for end-stage liver disease at a single tertiary referral center between January 2014 and December 2018. The patients were categorized into the pre-MELD (22 patients) and post-MELD (26 patients) groups. The demographics, postoperative outcomes, and overall survival time were evaluated between the 2 groups.
Results
The 2 groups had no differences in age, sex, ABO type, etiology for liver transplantation, CTP-score, operation time, cold ischemic time, and amount of red blood cell transfusion, although their MELD score differed significantly (postMELD group, 36.2 ± 4.9; pre-MELD group, 27.7 ± 11.8; P < 0.001). The post-MELD group has longer intensive care unit stay (11.2 ± 9.5 days vs. 5.7 ± 4.5 days, P = 0.018) and hospital stay than the pre-MELD group (36.8 ± 26 days vs. 22.8 ± 9.3 days, P = 0.016). The 1-year survival rate was lower in the post-MELD group (61.5% vs. 86.4%, P = 0.029).
Conclusion
After MELD allocation, patients with high MELD scores had increased DDLT and consequently required a longer recovery time, which could negatively affect survival. According to the experience of a small-volume center, these problems were related to both severe organ shortages in South Korea and MELD allocation.
Keyword
Figure
Reference
-
1. Hong G, Lee KW, Suh S, Yoo T, Kim H, Park MS, et al. The model for end-stage liver disease score-based system predicts short term mortality better than the current Child-Turcotte-Pugh score-based allocation system during waiting for deceased liver transplantation. J Korean Med Sci. 2013; 28:1207–1212. PMID: 23960449.
Article2. Min SI, Ahn C, Han DJ, Kim SI, Chung SY, Lee SK, et al. To achieve national self-sufficiency: recent progresses in deceased donation in Korea. Transplantation. 2015; 99:765–770. PMID: 25226175.3. Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology. 2000; 31:864–871. PMID: 10733541.
Article4. Kim MS. Modification of emergency status in deceased donor liver allocation: evidence for Korean Model of End-stage Liver Disease (MELD) system. J Korean Soc Transplant. 2016; 30:51–58.
Article5. Dutkowski P, Oberkofler CE, Béchir M, Müllhaupt B, Geier A, Raptis DA, et al. The model for end-stage liver disease allocation system for liver transplantation saves lives, but increases morbidity and cost: a prospective outcome analysis. Liver Transpl. 2011; 17:674–684. PMID: 21618688.
Article6. Lee JA, Choi GS, Kim JM, Kwon CHD, Joh JW. Comparison study of outcomes of deceased donor liver transplantation before and after Korean model for End-Stage Liver Disease (MELD) system: single center experience. J Korean Soc Transplant. 2018; 32:7–11.
Article7. Dunn W, Jamil LH, Brown LS, Wiesner RH, Kim WR, Menon KV, et al. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology. 2005; 41:353–358. PMID: 15660383.
Article8. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.9. Freeman RB Jr, Gish RG, Harper A, Davis GL, Vierling J, Lieblein L, et al. Model for end-stage liver disease (MELD) exception guidelines: results and recommendations from the MELD Exception Study Group and Conference (MESSAGE) for the approval of patients who need liver transplantation with diseases not considered by the standard MELD formula. Liver Transpl. 2006; 12(12 Suppl 3):S128–S136. PMID: 17123284.
Article10. Kwon TJ, Kang W, Gwak GY, Paik YH, Choi MS, Lee JH, et al. Outcome of patients with severe alcoholic hepatitis after Model for End-Stage Liver Disease-based allocation system implementation in Korea. Korean J Transplant. 2021; 35:24–32.
Article11. Lee J, Kim DG, Lee JY, Lee JG, Joo DJ, Kim SI, et al. Impact of Model for End-stage Liver Disease Score-based allocation system in Korea: a nationwide study. Transplantation. 2019; 103:2515–2522. PMID: 30985735.
Article12. Cywinski JB, Mascha EJ, You J, Sessler DI, Kapural L, Argalious M, et al. Pre-transplant MELD and sodium MELD scores are poor predictors of graft failure and mortality after liver transplantation. Hepatol Int. 2011; 5:841–849. PMID: 21484127.
Article13. Heo SJ, Ju YH, Noh EJ, Kim KM, Son YK, Jung SW, et al. A study on the performance of the Donat ion Improvement Program in Korea. Korean J Transplant. 2021; 35:77–85.14. Park HS, Lee JM, Hong K, Han ES, Hong SK, Choi Y, et al. Impact of Model for End-Stage Liver Disease allocation system on outcomes of deceased donor liver transplantation: a single-center experience. Ann Hepatobiliary Pancreat Surg. 2021; 25:336–341. PMID: 34402433.
Article15. Cho WH. Causes of donation failure and improvement measures analyzed based on data from domestic deceased donors in 2019. Korean J Transplant. 2020; 34:219–230.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Deceased Donor Liver Transplantation for Alcoholic Liver Disease in Korea in MELD Era
- Liver transplantation: a 10-year low-volume transplant center experience in Kazakhstan
- Simultaneous liver-kidney transplantation: a single-center experience in Korea
- Impact of the introduction of the model for end-stage liver disease system on the low volume liver transplant centers: a multicenter study
- A study on differences in deceased donor liver transplantation before and after the introduction of the model for end-stage liver disease system: three low volume centers, multi-center trial