Ann Surg Treat Res.
2021 Dec;101(6):340-349. 10.4174/astr.2021.101.6.340.
Predictive factors of high comprehensive complication index in colorectal cancer patients using Enhanced Recovery After Surgery protocol: role as a safety net in early discharge
- Affiliations
-
- 1Division of Colorectal Surgery, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Colorectal Surgery, Department of Surgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2522932
- DOI: http://doi.org/10.4174/astr.2021.101.6.340
Abstract
- Purpose
This study was performed to evaluate complications using comprehensive complication index (CCI) in colorectal cancer patients with implementation of the Enhanced Recovery After Surgery (ERAS) protocol, and to investigate the predictive factors associated with high morbidity rates. It can be used as a safety net in determining the timing of discharge.
Methods
A total of 335 consecutive patients who underwent elective colorectal cancer surgery between January 2017 and December 2017 at a single tertiary center were enrolled. Postoperative complications were defined as occurring within 30 days after surgery. The predictive factor analysis for the high CCI group was also performed.
Results
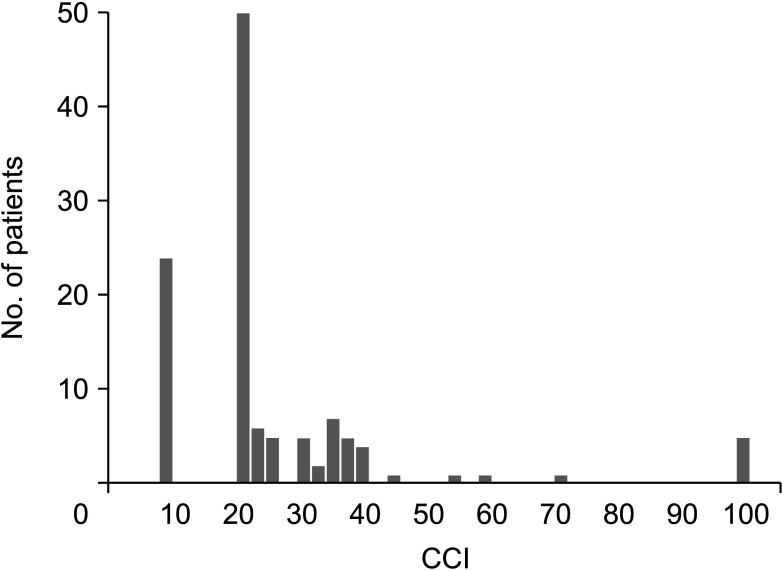
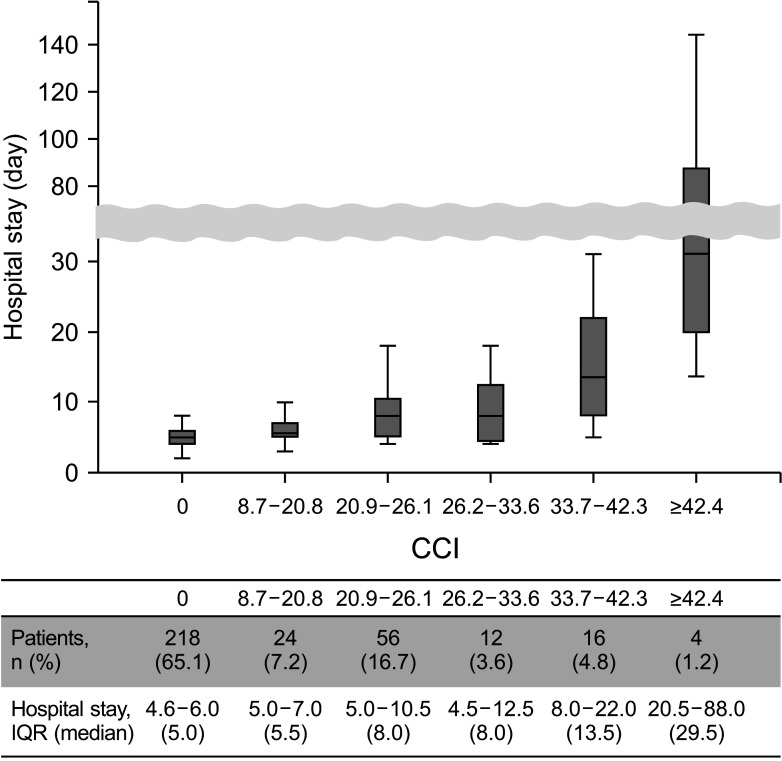
In total, 116 patients experienced postoperative complications. Wound-related complications and postoperative ileus were the most common. The mean CCI for overall colorectal cancer surgery was 9.1 ± 16.7. Patients featuring low CCI (<26.2) were 297 (88.7%) and high CCI were 38 (11.3%). In multivariable analysis, obstructive colorectal cancer (odds ratio, 3.278; 95% confidence interval, 1.217–8.829; P = 0.019) and CRP value on postoperative day (POD) 3–4 (odds ratio, 1.152; 95% confidence interval, 1.036–1.280; P < 0.010) were significant predictors for high CCI.
Conclusion
The clinical usefulness of CCI in colorectal cancer patients with the ERAS protocol was verified, and it can be used for surgical quality control. More cautious care is needed and the timing of discharge should be carefully determined for patients with obstructive colorectal cancer or POD 3–4 CRP of ≥6.47 mg/dL.
Keyword
Figure
Reference
-
1. van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013; 14:210–218. PMID: 23395398.
Article2. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005; 6:477–484. PMID: 15992696.3. Mavros MN, de Jong M, Dogeas E, Hyder O, Pawlik TM. Impact of complications on long-term survival after resection of colorectal liver metastases. Br J Surg. 2013; 100:711–718. PMID: 23364914.
Article4. Yamashita S, Sheth RA, Niekamp AS, Aloia TA, Chun YS, Lee JE, et al. Comprehensive complication index predicts cancer-specific survival after resection of colorectal metastases independent of RAS mutational status. Ann Surg. 2017; 266:1045–1054. PMID: 27735824.
Article5. Liu VX, Rosas E, Hwang J, Cain E, Foss-Durant A, Clopp M, et al. Enhanced recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017; 152:e171032. PMID: 28492816.
Article6. Kim MK, Kim JG, Lee G, Won DD, Lee YS, Kye BH, et al. Comparison of the effects of an ERAS program and a single-port laparoscopic surgery on postoperative outcomes of colon cancer patients. Sci Rep. 2019; 9:11998. PMID: 31427651.
Article7. Hughes MJ, Hackney RJ, Lamb PJ, Wigmore SJ, Christopher Deans DA, Skipworth RJ. Prehabilitation before major abdominal surgery: a systematic review and meta-analysis. World J Surg. 2019; 43:1661–1668. PMID: 30788536.
Article8. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.9. Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013; 258:1–7. PMID: 23728278.10. Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013; 56:667–678. PMID: 23575408.11. Feng F, Li XH, Shi H, Wu GS, Zhang HW, Liu XN, et al. Fast-track surgery combined with laparoscopy could improve postoperative recovery of low-risk rectal cancer patients: a randomized controlled clinical trial. J Dig Dis. 2014; 15:306–313. PMID: 24597608.
Article12. Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014; 38:1531–1541. PMID: 24368573.
Article13. Lee CS, Won DD, Oh SN, Lee YS, Lee IK, Kim IH, et al. Prognostic role of pre-sarcopenia and body composition with long-term outcomes in obstructive colorectal cancer: a retrospective cohort study. World J Surg Oncol. 2020; 18:230. PMID: 32859211.
Article14. Verheyden C, Orliac C, Millet I, Taourel P. Large-bowel obstruction: CT findings, pitfalls, tips and tricks. Eur J Radiol. 2020; 130:109155. PMID: 32711335.
Article15. Casadei-Gardini A, Scarpi E, Ulivi P, Palladino MA, Accettura C, Bernardini I, et al. Prognostic role of a new inflammatory index with neutrophil-to-lymphocyte ratio and lactate dehydrogenase (CII: Colon Inflammatory Index) in patients with metastatic colorectal cancer: results from the randomized Italian Trial in Advanced Colorectal Cancer (ITACa) study. Cancer Manag Res. 2019; 11:4357–4369. PMID: 31191000.16. Mazaki J, Katsumata K, Kasahara K, Tago T, Wada T, Kuwabara H, et al. Neutrophil-to-lymphocyte ratio is a prognostic factor for colon cancer: a propensity score analysis. BMC Cancer. 2020; 20:922. PMID: 32977767.
Article17. Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010; 147:339–351. PMID: 20004450.
Article18. Kim TH, Suh YS, Huh YJ, Son YG, Park JH, Yang JY, et al. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric Cancer. 2018; 21:171–181. PMID: 28597328.
Article19. Tu RH, Lin JX, Li P, Xie JW, Wang JB, Lu J, et al. Comprehensive complication index predicts cancer-specific survival of patients with postoperative complications after curative resection of gastric cancer. Gastroenterol Res Pract. 2018; 2018:4396018. PMID: 30581463.
Article20. Clinical Outcomes of Surgical Therapy Study Group. Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350:2050–2059. PMID: 15141043.
Article21. Hübner M, Diana M, Zanetti G, Eisenring MC, Demartines N, Troillet N. Surgical site infections in colon surgery: the patient, the procedure, the hospital, and the surgeon. Arch Surg. 2011; 146:1240–1245. PMID: 21768407.22. Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, et al. Wound infection after elective colorectal resection. Ann Surg. 2004; 239:599–607. PMID: 15082963.
Article23. Venara A, Neunlist M, Slim K, Barbieux J, Colas PA, Hamy A, et al. Postoperative ileus: pathophysiology, incidence, and prevention. J Visc Surg. 2016; 153:439–446. PMID: 27666979.
Article24. Borchert DH, Federlein M, Müller VA, Wagenpfeil S, Eisele RM. Comprehensive complication index for NOTES procedures: results from a randomized controlled trial and comparison to published NOTES complication data. Surg Endosc. 2015; 29:2928–2933. PMID: 25539692.
Article25. Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: a review. JAMA Surg. 2017; 152:292–298. PMID: 28097305.26. Slankamenac K, Nederlof N, Pessaux P, de Jonge J, Wijnhoven BP, Breitenstein S, et al. The comprehensive complication index: a novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann Surg. 2014; 260:757–763. PMID: 25379846.27. Spannenburg L, Sanchez Gonzalez M, Brooks A, Wei S, Li X, Liang X, et al. Surgical outcomes of colonic stents as a bridge to surgery versus emergency surgery for malignant colorectal obstruction: a systematic review and meta-analysis of high quality prospective and randomised controlled trials. Eur J Surg Oncol. 2020; 46:1404–1414. PMID: 32418754.
Article28. Cheynel N, Cortet M, Lepage C, Benoit L, Faivre J, Bouvier AM. Trends in frequency and management of obstructing colorectal cancers in a well-defined population. Dis Colon Rectum. 2007; 50:1568–1575. PMID: 17687610.
Article29. Yang XF, Pan K. Diagnosis and management of acute complications in patients with colon cancer: bleeding, obstruction, and perforation. Chin J Cancer Res. 2014; 26:331–340. PMID: 25035661.30. Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br J Surg. 1994; 81:1270–1276. PMID: 7953385.
Article31. Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003; 111:1805–1812. PMID: 12813013.
Article32. Bray C, Bell LN, Liang H, Haykal R, Kaiksow F, Mazza JJ, et al. Erythrocyte sedimentation rate and c-reactive protein measurements and their relevance in clinical medicine. WMJ. 2016; 115:317–321. PMID: 29094869.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical validation of implementing Enhanced Recovery After Surgery protocol in elderly colorectal cancer patients
- Influence of the Enhanced Recovery After Surgery Protocol on Postoperative Inflammation and Short-term Postoperative Surgical Outcomes After Colorectal Cancer Surgery
- Fast-Track Colorectal Surgery
- Implementation and improvement of Enhanced Recovery After Surgery protocols for colorectal cancer surgery
- Which patients with gastric cancer should be candidates for Enhanced Recovery After Surgery protocols?