Clin Exp Otorhinolaryngol.
2021 Nov;14(4):407-413. 10.21053/ceo.2020.00234.
Externally Monitored Versus Conventional Buried Flaps in Laryngopharyngeal Reconstruction
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Cheonan, Korea
- 2Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Korea
- 3Clinical Trial Center, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2522432
- DOI: http://doi.org/10.21053/ceo.2020.00234
Abstract
Objectives
. To compare the surgical outcomes of externally monitored and conventional buried flaps with the goal of determining the usefulness of external monitoring of buried flaps.
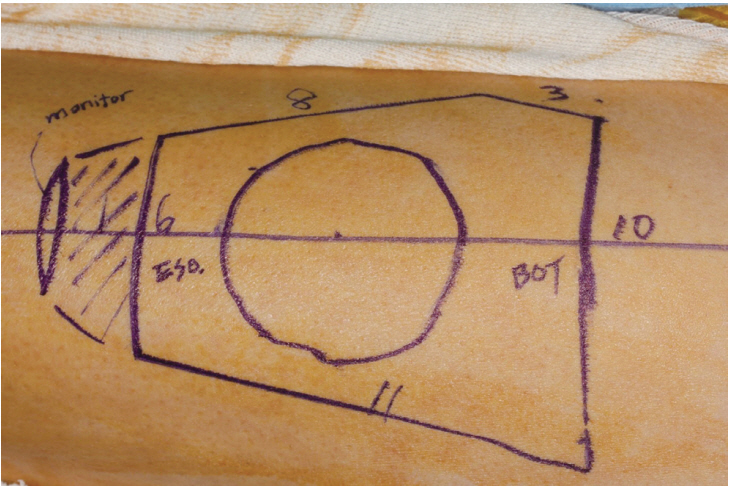
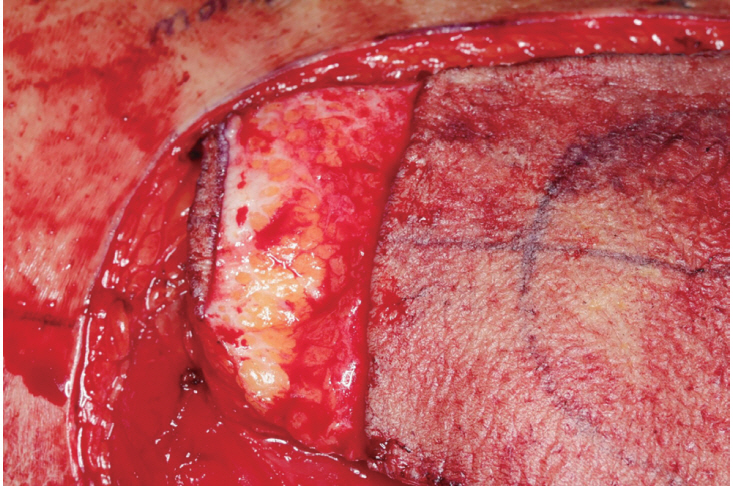
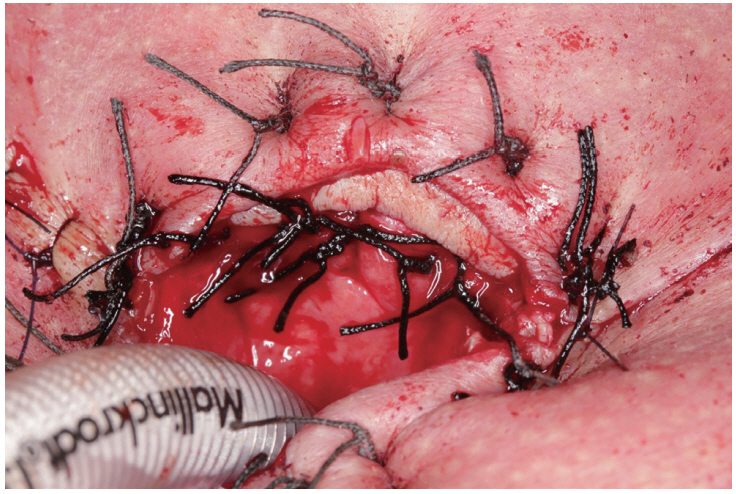
Methods
. In this case-control study with propensity score matching, 30 patients were evenly divided into externally monitored buried flap and conventional buried flap groups. The total operative time for free flap reconstruction, the flap survival rate, the length of hospital stay, the initial time of a reliable visual assessment, complications, the final diet achieved, and the duration until diet initiation were compared between the groups.
Results
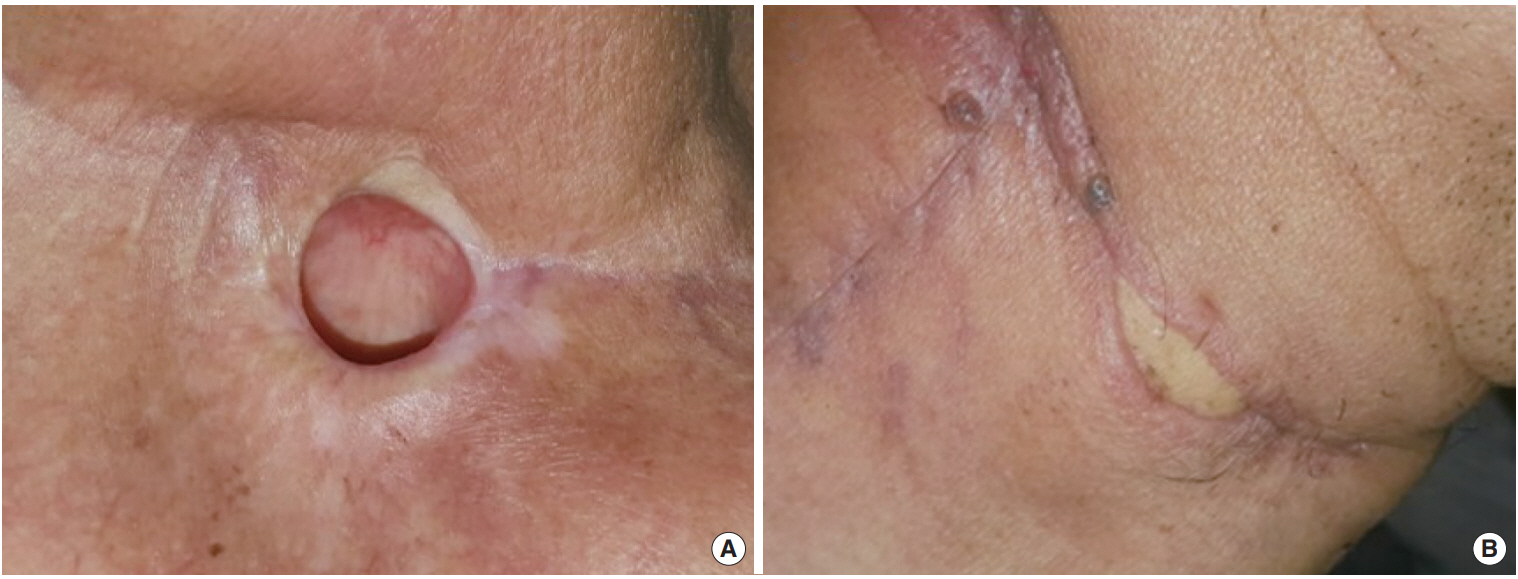
. The mean operative time for reconstruction was 115 minutes (interquartile range, 85–150 minutes) and 142 minutes (interquartile range, 95–180 minutes) in the externally monitored and conventional groups, respectively (P= 0.245). The median length of hospital stay was 24 days (interquartile range, 18–30 days) and 27 days (interquartile range, 20–41 days) in the externally monitored and conventional groups, respectively (P=0.298). The median duration until diet initiation was 15 days (interquartile range, 15–21 days) and 18 days (interquartile range, 15–34 days) in the externally monitored and conventional groups, respectively (P=0.466). The final diet, initial time of a reliable visual assessment, and complications were comparable between the groups, but the external skin paddle provided an excellent visual assessment immediately postoperatively in all cases.
Conclusion
. The outcomes were comparable between the groups, indicating that externalization of the cutaneous component of a buried flap may be a straightforward and useful technique for monitoring a buried anterolateral thigh free flap in laryngopharyngeal reconstructions. The salvage and false-positive rates of compromised flaps should be compared in large subject groups in future studies to prove that the use of an external skin paddle improves flap monitoring.
Keyword
Figure
Cited by 1 articles
-
Cumulative Sum Analysis of the Learning Curve of Free Flap Reconstruction in Head and Neck Cancer Patients
Seung Hoon Han, Young Chul Kim, Tack-Kyun Kwon, Doh Young Lee
Clin Exp Otorhinolaryngol. 2022;15(2):177-182. doi: 10.21053/ceo.2021.01053.
Reference
-
1. Chae MP, Rozen WM, Whitaker IS, Chubb D, Grinsell D, Ashton MW, et al. Current evidence for postoperative monitoring of microvascular free flaps: a systematic review. Ann Plast Surg. 2015; May. 74(5):621–32.2. Buncke HJ. Microsurgery: transplantation-replantation, an atlas text. Philadelphia (PA): Lea & Febiger;1991.3. Disa JJ, Cordeiro PG, Hidalgo DA. Efficacy of conventional monitoring techniques in free tissue transfer: an 11-year experience in 750 consecutive cases. Plast Reconstr Surg. 1999; Jul. 104(1):97–101.
Article4. Jones BM. Monitors for the cutaneous microcirculation. Plast Reconstr Surg. 1984; May. 73(5):843–50.
Article5. Pellini R, Pichi B, Marchesi P, Cristalli G, Deganello A, Spriano G. External monitor for buried free flaps in head and neck reconstructions. Acta Otorhinolaryngol Ital. 2006; Feb. 26(1):1–6.6. Ferguson RE Jr, Yu P. Techniques of monitoring buried fasciocutaneous free flaps. Plast Reconstr Surg. 2009; Feb. 123(2):525–32.
Article7. Yu P, Robb GL. Pharyngoesophageal reconstruction with the anterolateral thigh flap: a clinical and functional outcomes study. Plast Reconstr Surg. 2005; 116(7):1845–55.
Article8. Yu P, Hanasono MM, Skoracki RJ, Baumann DP, Lewin JS, Weber RS, et al. Pharyngoesophageal reconstruction with the anterolateral thigh flap after total laryngopharyngectomy. Cancer. 2010; Apr. 116(7):1718–24.
Article9. Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011; Mar-Apr. 10(2):150–61.
Article10. Lindau RH, Detwiller K, Wax MK. Buried free flaps in head and neck surgery: outcome analysis. Head Neck. 2013; Oct. 35(10):1468–70.
Article11. Kim SY, Kang CH, Park IK, Kim YT. Esophageal stent insertion for postesophagectomy anastomosis site leakage. Clin Exp Otorhinolaryngol. 2016; Dec. 9(4):382–4.
Article12. Haksever M, Akduman D, Aslan S, Solmaz F, Ozmen S. Modified continuous mucosal Connell suture for the pharyngeal closure after total laryngectomy: zipper suture. Clin Exp Otorhinolaryngol. 2015; Sep. 8(3):281–8.
Article13. Pirracchio R, Resche-Rigon M, Chevret S. Evaluation of the propensity score methods for estimating marginal odds ratios in case of small sample size. BMC Med Res Methodol. 2012; May. 12:70.
Article14. Chang EI, Zhang H, Liu J, Yu P, Skoracki RJ, Hanasono MM. Analysis of risk factors for flap loss and salvage in free flap head and neck reconstruction. Head Neck. 2016; Apr. 38 Suppl 1:E771–5.
Article15. Kim H, Jeong WJ, Ahn SH. Results of free flap reconstruction after ablative surgery in the head and neck. Clin Exp Otorhinolaryngol. 2015; Jun. 8(2):167–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contribution of Perforator Flaps in the Flap Selection for Head and Neck Reconstruction
- Perforator Flap versus Conventional Flap
- Pedicled sural flaps versus free anterolateral thigh flaps in reconstruction of dorsal foot and ankle defects in children: a systematic review
- Various Utility of Perforator Flaps in Head and Neck Reconstruction
- Perforator Flaps in Head and Neck Reconstruction