J Korean Med Sci.
2015 May;30(5):514-522. 10.3346/jkms.2015.30.5.514.
Perforator Flap versus Conventional Flap
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, College of Medicine, Hanyang University, Seoul, Korea.
- 2Department of Plastic and Reconstructive Surgery, College of Medicine, Seoul National University, Seoul National University Hospital, Seoul, Korea. sw1215@snu.ac.kr
- KMID: 2155462
- DOI: http://doi.org/10.3346/jkms.2015.30.5.514
Abstract
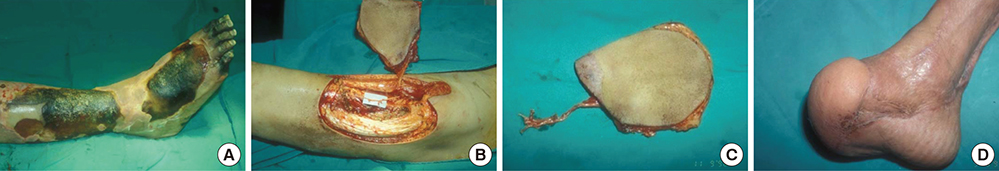
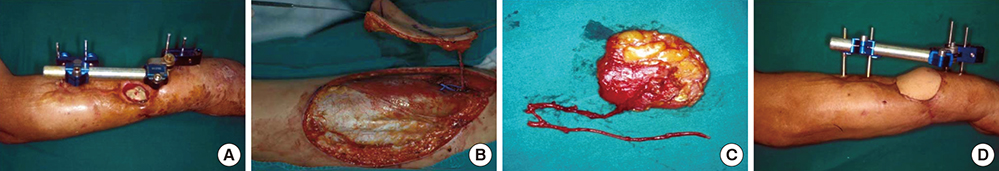
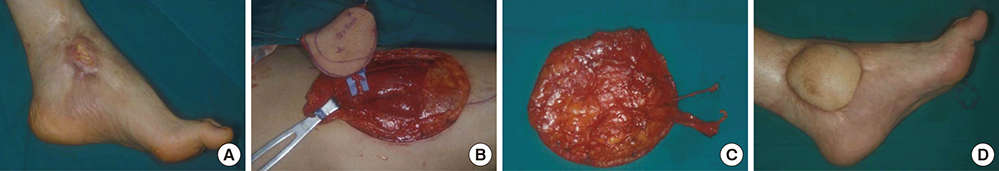
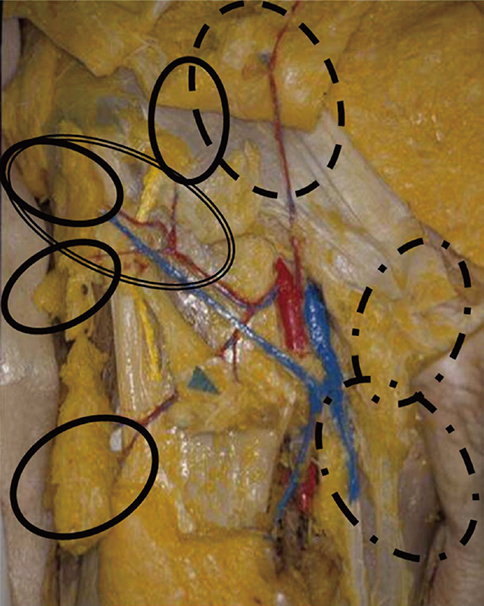
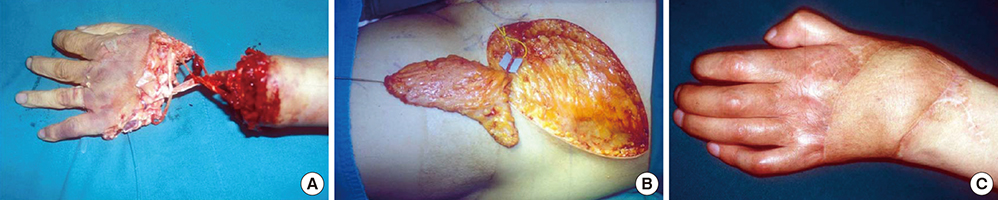
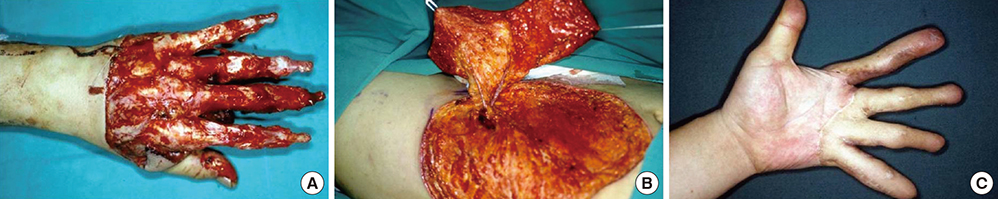
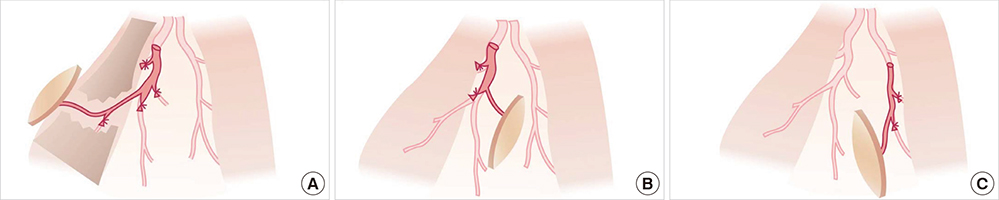
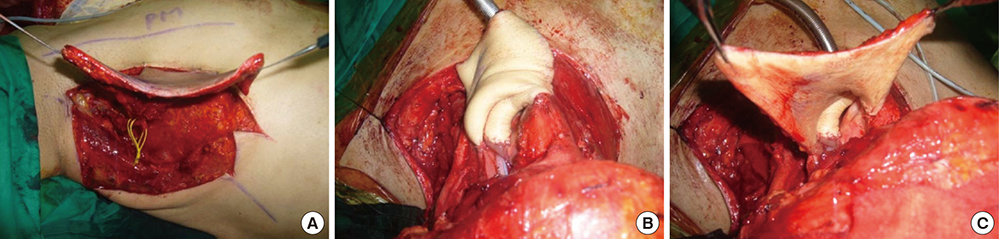
- The introduction of perforator flaps represented a significant advance in microsurgical reconstruction. However, confusion has developed due to the erroneous belief that perforator flaps are different from conventional flaps. The concept of the perforator is not new, but is an idea that evolved from the conventional flap. In fact, some of the flaps used by microsurgeons were perforator flaps. The only difference is the anatomical level of the blood vessels involved; the perforator concept is focused on the distal circulation, so-called 'perforator'. Therefore, thinner sections of tissue can be taken from the conventional donor sites of myocutaneous flaps. With the use of perforators, there are no longer "flap of choice" for specific reconstructions, because conventional donor sites have become universal donor sites, enabling the harvesting of a variety of flaps. Moreover, depending on the surgeon's ability, any flap can be utilized as a perforator-based island flap whose source vessel has been completely preserved. Therefore, tissues can be efficiently customized and tailored into any configuration required for reconstruction. The application of perforator flap technique enables more precise dissection, and allows more selective harvesting of thinner flaps, which will expand options in reconstructive surgery. No doubt the technique will continue to evolve.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Propeller Dorsal Intercostal Artery Perforator Flap for an Extensive Defect on the Back Following Malignant Peripheral Nerve Sheath Tumor Resection: A Case Report
Seung Han Song, Hyeokdong Kwon, Sunje Kim, Joo Hak Kim, Hyun Woo Kyung, Sang-Ha Oh, Ho Jik Yang, Yooseok Ha
Arch Hand Microsurg. 2021;26(1):63-67. doi: 10.12790/ahm.20.0068.
Reference
-
1. Geddes CR, Morris SF, Neligan PC. Perforator flaps: evolution, classification, and applications. Ann Plast Surg. 2003; 50:90–99.2. McGregor IA, Morgan G. Axial and random pattern flaps. Br J Plast Surg. 1973; 26:202–213.3. Sinna R, Boloorchi A, Mahajan AL, Qassemyar Q, Robbe M. What should define a "perforator flap"? Plast Reconstr Surg. 2010; 126:2258–2263.4. Blondeel PN, Morris SF, Hallock GG, Heligan PC. Perforator flaps: anatomy, technique and clinical application. St. Louis: Quality Medical;2006.5. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987; 40:113–141.6. Wei FC, Celik N. Perforator flap entity. Clin Plast Surg. 2003; 30:325–329.7. Wei FC, Mardini S. Free-style free flaps. Plast Reconstr Surg. 2004; 114:910–916.8. Grover R, Nelson JA, Fischer JP, Kovach SJ, Serletti JM, Wu LC. The impact of perforator number on deep inferior epigastric perforator flap breast reconstruction. Arch Plast Surg. 2014; 41:63–70.9. Saint-Cyr M, Schaverien MV, Rohrich RJ. Perforator flaps: history, controversies, physiology, anatomy, and use in reconstruction. Plast Reconstr Surg. 2009; 123:132e–145e.10. Kim JT. New nomenclature concept of perforator flap. Br J Plast Surg. 2005; 58:431–440.11. Wei FC, Jain V, Suominen S, Chen HC. Confusion among perforator flaps: what is a true perforator flap? Plast Reconstru Surg. 2001; 107:874–876.12. Kang MJ, Chung CH, Chang YJ, Kim KH. Reconstruction of the lower extremity using free flaps. Arch Plast Surg. 2013; 40:575–583.13. Agostini T, Russo GL, Zhang YX, Spinelli G, Lazzeri D. Adipofascial anterolateral thigh flap safety: applications and complications. Arch Plast Surg. 2013; 40:91–96.14. Lee MJ, Yun IS, Rah DK, Lee WJ. Lower extremity reconstruction using vastus lateralis myocutaneous flap versus anterolateral thigh fasciocutaneous flap. Arch Plast Surg. 2012; 39:367–375.15. Pribaz JJ, Chan RK. Where do perforator flaps fit in our armamentarium? Clin Plast Surg. 2010; 37:571–579.16. Kim JT. Latissimus dorsi perforator flap. Clin Plast Surg. 2003; 30:403–431.17. McGregor IA, Jackson IT. The groin flap. Br J Plast Surg. 1972; 25:3–16.18. Zayakova Y, Stanev A, Mihailov H, Pashaliev N. Application of local axial flaps to scalp reconstruction. Arch Plast Surg. 2013; 40:564–569.19. Yoo KW, Shin HW, Lee HK. A case of urethral reconstruction using a superficial circumflex iliac artery. Arch Plast Surg. 2012; 39:253–256.20. Han DH, Park MC, Park DH, Song H, Lee IJ. Role of muscle free flap in the salvage of complicated scalp wounds and infected prosthetic dura. Arch Plast Surg. 2013; 40:735–741.21. Yoon SK, Song SH, Kang N, Yoon YH, Koo BS, Oh SH. Reconstruction of the head and neck region using lower trapezius musculocutaneous flaps. Arch Plast Surg. 2012; 39:626–630.22. McCraw JB, Vasconez LO. Musculocutaneous flaps: principles. Clin Plast Surg. 1980; 7:9–13.23. Mathes SJ, Nahai F. Clinical atlas of muscle and musculocutaneous flaps. St. Louis: CV Mosby;1979.24. Yang J, Ko SH, Oh SJ, Jung SW. Reconstruction of a perineoscrotal defect using bilateral medial thigh fasciocutaneous flaps. Arch Plast Surg. 2013; 40:72–74.25. Shin IS, Lee DW, Rah DK, Lee WJ. Reconstruction of pretibial defect using pedicled perforator flaps. Arch Plast Surg. 2012; 39:360–366.26. Pontén B. The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg. 1981; 34:215–220.27. Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989; 42:645–648.28. Park JS, Roh SG, Lee NH, Yang KM. Versatility of the distally-based sural artery fasciocutaneous flap on the lower leg and foot in patients with chronic disease. Arch Plast Surg. 2013; 40:220–225.29. Tan S, Lim J, Yek J, Ong WC, Hing CH, Lim TC. The deep inferior epigastric perforator and pedicled transverse rectus abdominis myocutaneous flap in breast reconstruction: a comparative study. Arch Plast Surg. 2013; 40:187–191.30. Kimura N, Satoh K. Consideration of a thin flap as an entity and clinical applications of the thin anterolateral thigh flap. Plast Reconstr Surg. 1996; 97:985–992.31. Kim JT. Two options for perforator flaps in the flank donor site: latissimus dorsi and thoracodorsal perforator flaps. Plast Reconstr Surg. 2005; 115:755–763.32. Kim JT, Ng SW, Naidu S, Kim JD, Kim YH. Lateral thoracic perforator flap: additional perforator flap option from the lateral thoracic region. J Plast Reconstr Aesthet Surg. 2011; 64:1596–1602.33. Yang JD, Ryu DW, Lee JW, Choi KY, Chung HY, Cho BC, Park HY, Byun JS. Usefulness of a lateral thoracodorsal flap after breast conserving surgery in laterally located breast cancer. Arch Plast Surg. 2013; 40:367–373.34. Jeong JH, Hong JM, Imanishi N, Lee Y, Chang H. Face reconstruction using lateral intercostal artery perforator-based adipofascial free flap. Arch Plast Surg. 2014; 41:50–56.35. De la Parra M, Sanchez G, Lopez J, Perez A, Naal N. Total maxillary reconstruction using a double-barreled and double skin paddle fibular flap after total maxillectomy. Arch Plast Surg. 2013; 40:779–782.36. Yoon TH, Yun IS, Rha DK, Lee WJ. Reconstruction of various perinasal defects using facial artery perforator-based nasolabial island flaps. Arch Plast Surg. 2013; 40:754–760.37. Lazzeri D, Huemer GM, Nicoli F, Larcher L, Dashti T, Grassetti L, Li Q, Zhang Y, Spinelli G, Agostini T. Indications, outcomes, and complications of pedicled propeller perforator flaps for upper body defects: a systematic review. Arch Plast Surg. 2013; 40:44–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Flap thinning: Defatting after conventional elevation
- Contribution of Perforator Flaps in the Flap Selection for Head and Neck Reconstruction
- Reconstruction of the Soft Tissue Defect Using Thoracodorsal Artery Perforator Skin Flap
- Dual Perforator Flap for Reconstruction of Large Sacral Defects: Superior Gluteal Artery Perforator Super-Flap with Parasacral Perforator
- Perineal Reconstruction with the Perineal Perforator Based Island Flap