Neurointervention.
2021 Nov;16(3):240-251. 10.5469/neuroint.2021.00437.
Monitoring Radiation Doses during Diagnostic and Therapeutic Neurointerventional Procedures: Multicenter Study for Establishment of Reference Levels
- Affiliations
-
- 1Department of Radiology, St. Vincent’s Hospital, The Catholic University of Korea, Suwon, Korea
- 2Department of Radiology, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- 3Department of Radiology, Busan Paik Hospital, Inje University, Busan, Korea
- 4Department of Radiology, Gangnam Severance Hospital, Yonsei University, Seoul, Korea
- 5Department of Radiology, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- 6Department of Radiology, Hanyang University College of Medicine, Seoul, Korea
- 7Department of Radiology, Severance Hospital, Yonsei Unviersity College of Medicine, Seoul, Korea
- 8Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 9Department of Radiology, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- 10Department of Radiology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 11Department of Radiology, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea
- 12Department of Radiology, Wonkwang University Hospital, Iksan, Korea
- 13Department of Radiology, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 14Department of Radiology, Chung-Ang University Hospital, Seoul, Korea
- 15Department of Radiology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 16Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 17Department of Radiology, Ajou University Medical Center, Ajou University School of Medicine, Suwon, Korea
- 18Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 19Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea
- 20Department of Neurology, Konkuk University Medical Center, Seoul, Korea
- 21Department of Radiology, Ewha Womans University Seoul Hospital, Seoul, Korea
- 22Department of Neurosurgery, Ewha Womans University Seoul Hospital, Seoul, Korea
- 23Department of Radiology, Chonnam National University Hospital, Gwangju, Korea
- KMID: 2522038
- DOI: http://doi.org/10.5469/neuroint.2021.00437
Abstract
- Purpose
To assess patient radiation doses during diagnostic and therapeutic neurointerventional procedures from multiple centers and propose dose reference level (RL).
Materials and Methods
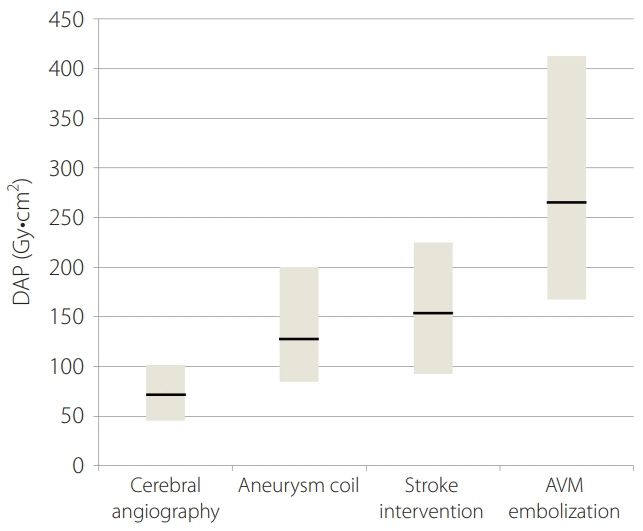
Consecutive neurointerventional procedures, performed in 22 hospitals from December 2020 to June 2021, were retrospectively studied. We collected data from a sample of 429 diagnostic and 731 therapeutic procedures. Parameters including dose-area product (DAP), cumulative air kerma (CAK), fluoroscopic time (FT), and total number of image frames (NI) were obtained. RL were calculated as the 3rd quartiles of the distribution.
Results
Analysis of 1160 procedures from 22 hospitals confirmed the large variability in patient dose for similar procedures. RLs in terms of DAP, CAK, FT, and NI were 101.6 Gy·cm2, 711.3 mGy, 13.3 minutes, and 637 frames for cerebral angiography, 199.9 Gy·cm2, 3,458.7 mGy, 57.3 minutes, and 1,000 frames for aneurysm coiling, 225.1 Gy·cm2, 1,590 mGy, 44.7 minutes, and 800 frames for stroke thrombolysis, 412.3 Gy·cm2, 4,447.8 mGy, 99.3 minutes, and 1,621.3 frames for arteriovenous malformation (AVM) embolization, respectively. For all procedures, the results were comparable to most of those already published. Statistical analysis showed male and presence of procedural complications were significant factors in aneurysmal coiling. Male, number of passages, and procedural combined technique were significant factors in stroke thrombolysis. In AVM embolization, a significantly higher radiation dose was found in the definitive endovascular cure group.
Conclusion
Various RLs introduced in this study promote the optimization of patient doses in diagnostic and therapeutic interventional neuroradiology procedures. Proposed 3rd quartile DAP (Gy·cm2) values were 101.6 for diagnostic cerebral angiography, 199.9 for aneurysm coiling, 225.1 for stroke thrombolysis, and 412.3 for AVM embolization. Continual evolution of practices and technologies requires regular updates of RLs.
Keyword
Figure
Reference
-
1. Alexander MD, Oliff MC, Olorunsola OG, Brus-Ramer M, Nickoloff EL, Meyers PM. Patient radiation exposure during diagnostic and therapeutic interventional neuroradiology procedures. J Neurointerv Surg. 2010; 2:6–10.
Article2. Valentin J. Avoidance of radiation injuries from medical interventional procedures. Ann ICRP. 2000; 30:7–67.3. The 2007 recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37:1–332.4. Vañó E, Miller DL, Martin CJ, Rehani MM, Kang K, Rosenstein M, Authors on behalf of ICRP, et al. ICRP publication 135: diagnostic reference levels in medical imaging. Ann ICRP. 2017; 46:1–144.
Article5. Aroua A, Rickli H, Stauffer JC, Schnyder P, Trueb PR, Valley JF, et al. How to set up and apply reference levels in fluoroscopy at a national level. Eur Radiol. 2007; 17:1621–1633.
Article6. Chung JW. Evaluation of patient dose in interventional radiology. Seoul: Korea Food & Drug Administration;2007.7. Chun CW, Kim BS, Lee CH, Ihn YK, Shin YS. Patient radiation dose in diagnostic and interventional procedures for intracranial aneurysms: experience at a single center. Korean J Radiol. 2014; 15:844–849.
Article8. Ihn YK, Kim BS, Byun JS, Suh SH, Won YD, Lee DH, et al. Patient radiation exposure during diagnostic and therapeutic procedures for intracranial aneurysms: a multicenter study. Neurointervention. 2016; 11:78–85.
Article9. Vano E, Järvinen H, Kosunen A, Bly R, Malone J, Dowling A, et al. Patient dose in interventional radiology: a European survey. Radiat Prot Dosimetry. 2008; 129:39–45.
Article10. Etard C, Bigand E, Salvat C, Vidal V, Beregi JP, Hornbeck A, et al. Patient dose in interventional radiology: a multicentre study of the most frequent procedures in France. Eur Radiol. 2017; 27:4281–4290.
Article11. Kien N, Rehel JL, Etard C, Aubert B. [Patient dose during interventional neuroradiology procedures: results from a multi-center study]. J Radiol. 2011; 92:1101–1112. French.12. Miller DL, Kwon D, Bonavia GH. Reference levels for patient radiation doses in interventional radiology: proposed initial values for U.S. practice. Radiology. 2009; 253:753–764.
Article13. Guenego A, Mosimann PJ, Pereira VM, Nicholson P, Zuber K, Lotterie JA, RADON Investigators, et al. Proposed achievable levels of dose and impact of dose-reduction systems for thrombectomy in acute ischemic stroke: an international, multicentric, retrospective study in 1096 patients. Eur Radiol. 2019; 29:3506–3515.
Article14. Farah J, Rouchaud A, Henry T, Regen C, Mihalea C, Moret J, et al. Dose reference levels and clinical determinants in stroke neuroradiology interventions. Eur Radiol. 2019; 29:645–653.
Article15. Acton H, James K, Kavanagh RG, O’Tuathaigh C, Moloney D, Wyse G, et al. Monitoring neurointerventional radiation doses using dose-tracking software: implications for the establishment of local diagnostic reference levels. Eur Radiol. 2018; 28:3669–3675.
Article16. Weyland CS, Hemmerich F, Möhlenbruch MA, Bendszus M, Pfaff JAR. Radiation exposure and fluoroscopy time in mechanical thrombectomy of anterior circulation ischemic stroke depending on the interventionalist’s experience-a retrospective single center experience. Eur Radiol. 2020; 30:1564–1570.
Article17. Forbrig R, Ozpeynirci Y, Grasser M, Dorn F, Liebig T, Trumm CG. Radiation dose and fluoroscopy time of modern endovascular treatment techniques in patients with saccular unruptured intracranial aneurysms. Eur Radiol. 2020; 30:4504–4513.
Article18. Peter Y, Speelman A, Daries V. Measurement of the average radiation dose to the local skin and thyroid gland during intracranial aneurysm coil embolization. Radiography (Lond). 2021; 27:255–259.
Article19. Kahn EN, Gemmete JJ, Chaudhary N, Thompson BG, Chen K, Christodoulou EG, et al. Radiation dose reduction during neurointerventional procedures by modification of default settings on biplane angiography equipment. J Neurointerv Surg. 2016; 8:819–823.
Article20. Morris PP, Geer CP, Singh J, Brinjikji W, Carter RE. Radiation dose reduction during neuroendovascular procedures. J Neurointerv Surg. 2018; 10:481–486.
Article21. Kawauchi S, Chida K, Moritake T, Hamada Y, Matsumaru Y, Tsuruta W, et al. Treatment of internal carotid aneurysms using pipeline embolization devices: measuring the radiation dose of the patient and determining the factors affecting it. Radiat Prot Dosimetry. 2020; 188:389–396.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient Radiation Dose in Neurointerventional Radiologic Procedure: A Tertiary Care Experience
- Review of National Diagnostic Reference Levels for Interventional Procedures
- Patient Radiation Dose in Diagnostic and Interventional Procedures for Intracranial Aneurysms: Experience at a Single Center
- Radiation Safety in Nuclear Medicine Procedures
- General Principles of Radiation Protection in Fields of Diagnostic Medical Exposure