Endocrinol Metab.
2021 Oct;36(5):938-951. 10.3803/EnM.2021.501.
T4+T3 Combination Therapy: An Unsolved Problem of Increasing Magnitude and Complexity
- Affiliations
-
- 1Department of Endocrinology, Amsterdam University Medical Center, Academic Medical Center, Amsterdam, the Netherlands
- KMID: 2521942
- DOI: http://doi.org/10.3803/EnM.2021.501
Abstract
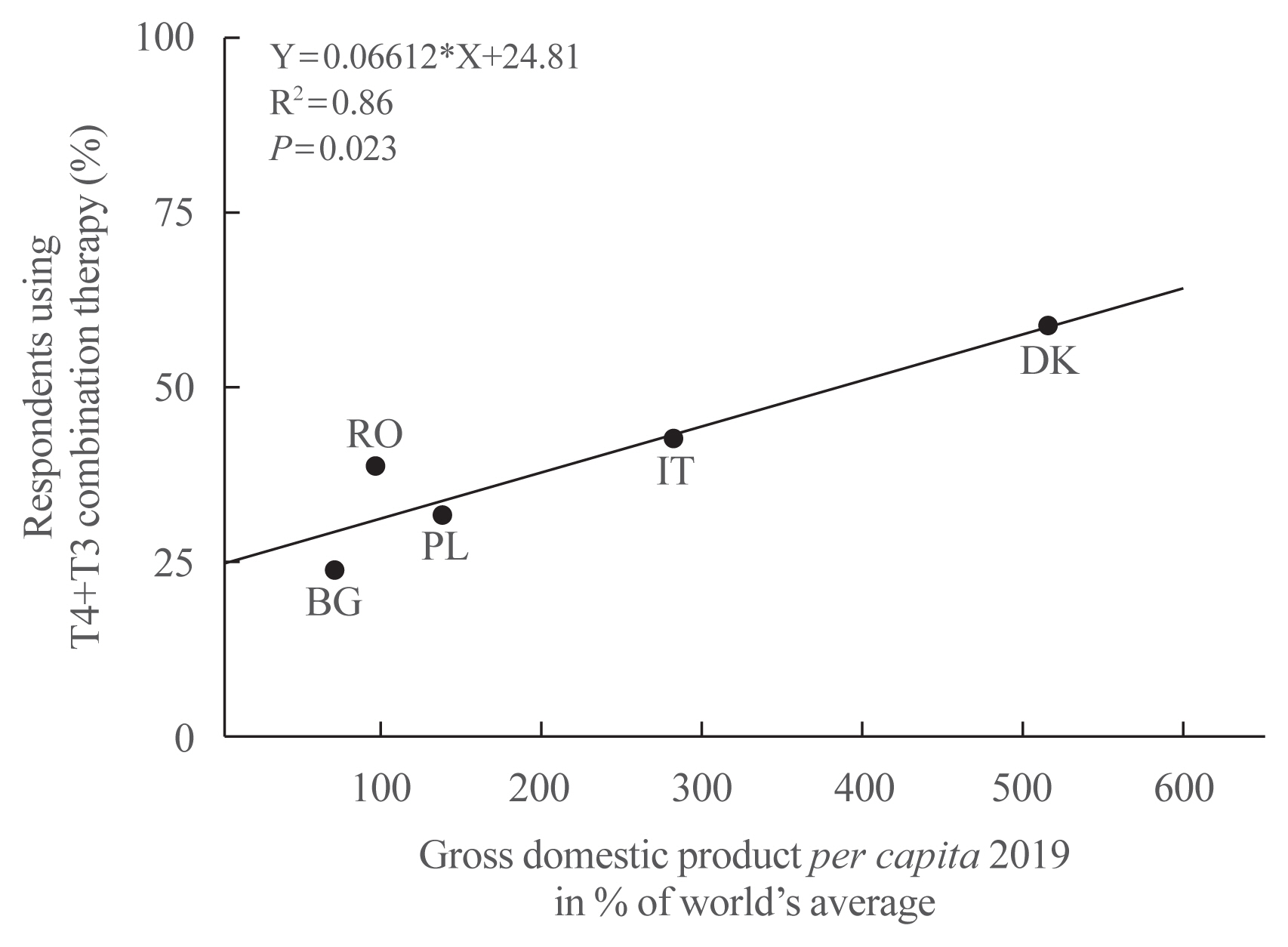
- Thyroxine (T4)+triiodothyronine (T3) combination therapy can be considered in case of persistent symptoms despite normal serum thyroid stimulating hormone in levothyroxine (LT4)-treated hypothyroid patients. Combination therapy has gained popularity in the last two decades, especially in countries with a relatively high gross domestic product. The prevalence of persistent symptoms has also increased; most frequent are complaints about energy levels and fatigue (80% to 90%), weight management (70% to 75%), memory (60% to 80%), and mood (40% to 50%). Pathophysiological explanations for persistent problems are unrealistic patient expectations, comorbidities, somatic symptoms, related disorders (Diagnostic and Statistical Manual of Mental Disorders [DSM-5]), autoimmune neuroinflammation, and low tissue T3. There is fair circumstantial evidence for the latter cause (tissue and specifically brain T3 content is normalized by T4+T3, not by T4 alone), but the other causes are viewed as more relevant in current practice. This might be related to the ‘hype’ that has emerged surrounding T4+T3 therapy. Although more and better-designed trials are needed to validate the efficacy of T4+T3 combination, the management of persistent symptoms should also be directed towards alternative causes. Improving the doctor-patient relationship and including more and better information is crucial. For example, dissatisfaction with the outcomes of T4 treatment for subclinical hypothyroidism can be anticipated as recent trials have demonstrated that LT4 is hardly effective in improving symptoms associated with subclinical hypothyroidism.
Keyword
Figure
Reference
-
1. Escobar-Morreale HF, Obregon MJ, Escobar del Rey F, Morreale de Escobar G. Replacement therapy for hypothyroidism with thyroxine alone does not ensure euthyroidism in all tissues, as studied in thyroidectomized rats. J Clin Invest. 1995; 96:2828–38.
Article2. Escobar-Morreale HF, del Rey FE, Obregon MJ, de Escobar GM. Only the combined treatment with thyroxine and triiodothyronine ensures euthyroidism in all tissues of the thyroidectomized rat. Endocrinology. 1996; 137:2490–502.
Article3. Grozinsky-Glasberg S, Fraser A, Nahshoni E, Weizman A, Leibovici L. Thyroxine-triiodothyronine combination therapy versus thyroxine monotherapy for clinical hypothyroidism: meta-analysis of randomized controlled trials. J Clin Endocrinol Metab. 2006; 91:2592–9.4. Wiersinga WM, Duntas L, Fadeyev V, Nygaard B, Vanderpump MP. 2012 ETA guidelines: the use of L-T4 + L-T3 in the treatment of hypothyroidism. Eur Thyroid J. 2012; 1:55–71.
Article5. Saravanan P, Chau WF, Roberts N, Vedhara K, Greenwood R, Dayan CM. Psychological well-being in patients on ‘adequate’ doses of l-thyroxine: results of a large, controlled community-based questionnaire study. Clin Endocrinol (Oxf). 2002; 57:577–85.6. Wekking EM, Appelhof BC, Fliers E, Schene AH, Huyser J, Tijssen JG, et al. Cognitive functioning and well-being in euthyroid patients on thyroxine replacement therapy for primary hypothyroidism. Eur J Endocrinol. 2005; 153:747–53.
Article7. Ettleson MD, Bianco AC. Individualized therapy for hypothyroidism: is T4 enough for everyone? J Clin Endocrinol Metab. 2020; 105:e3090–104.
Article8. Wiersinga WM. Paradigm shifts in thyroid hormone replacement therapies for hypothyroidism. Nat Rev Endocrinol. 2014; 10:164–74.
Article9. Wiersinga WM. Therapy of endocrine disease: T4 + T3 combination therapy: is there a true effect? Eur J Endocrinol. 2017; 177:R287–96.10. Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018; 14:301–16.
Article11. Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002; 87:489–99.12. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000; 160:526–34.
Article13. Garmendia Madariaga A, Santos Palacios S, Guillen-Grima F, Galofre JC. The incidence and prevalence of thyroid dysfunction in Europe: a meta-analysis. J Clin Endocrinol Metab. 2014; 99:923–31.
Article14. Mendes D, Alves C, Silverio N, Batel Marques F. Prevalence of undiagnosed hypothyroidism in Europe: a systematic review and meta-analysis. Eur Thyroid J. 2019; 8:130–43.
Article15. Valdes S, Maldonado-Araque C, Lago-Sampedro A, Lillo JA, Garcia-Fuentes E, Perez-Valero V, et al. Population-based national prevalence of thyroid dysfunction in Spain and associated factors: Di@bet.es Study. Thyroid. 2017; 27:156–66.
Article16. Kasagi K, Takahashi N, Inoue G, Honda T, Kawachi Y, Izumi Y. Thyroid function in Japanese adults as assessed by a general health checkup system in relation with thyroid-related antibodies and other clinical parameters. Thyroid. 2009; 19:937–44.
Article17. Chung JH. Evaluation of thyroid hormone levels and urinary iodine concentrations in Koreans based on the data from Korea National Health and Nutrition Examination Survey VI (2013 to 2015). Endocrinol Metab (Seoul). 2018; 33:160–3.
Article18. Kim WG, Kim WB, Woo G, Kim H, Cho Y, Kim TY, et al. Thyroid stimulating hormone reference range and prevalence of thyroid dysfunction in the Korean population: Korea National Health and Nutrition Examination Survey 2013 to 2015. Endocrinol Metab (Seoul). 2017; 32:106–14.
Article19. Leese GP, Flynn RV, Jung RT, Macdonald TM, Murphy MJ, Morris AD. Increasing prevalence and incidence of thyroid disease in Tayside, Scotland: the Thyroid Epidemiology Audit and Research Study (TEARS). Clin Endocrinol (Oxf). 2008; 68:311–6.
Article20. Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015; 314:1818–31.
Article21. Giorda CB, Carna P, Romeo F, Costa G, Tartaglino B, Gnavi R. Prevalence, incidence and associated comorbidities of treated hypothyroidism: an update from a European population. Eur J Endocrinol. 2017; 176:533–42.
Article22. Razvi S, Korevaar TIM, Taylor P. Trends, determinants, and associations of treated hypothyroidism in the United Kingdom, 2005–2014. Thyroid. 2019; 29:174–82.
Article23. Ingoe L, Phipps N, Armstrong G, Rajagopal A, Kamali F, Razvi S. Prevalence of treated hypothyroidism in the community: analysis from general practices in North-East England with implications for the United Kingdom. Clin Endocrinol (Oxf). 2017; 87:860–4.
Article24. Johansen ME, Marcinek JP, Doo Young Yun J. Thyroid hormone use in the United States, 1997–2016. J Am Board Fam Med. 2020; 33:284–8.
Article25. Rodriguez-Gutierrez R, Maraka S, Ospina NS, Montori VM, Brito JP. Levothyroxine overuse: time for an about face? Lancet Diabetes Endocrinol. 2017; 5:246–8.
Article26. Statista. Leading chemical drugs dispenses in England 2019 [Internet]. New York: Statista Inc.;2021. [cited 2021 Aug 27]. Available from: https://www.statista.com .27. Taylor PN, Iqbal A, Minassian C, Sayers A, Draman MS, Greenwood R, et al. Falling threshold for treatment of borderline elevated thyrotropin levels-balancing benefits and risks: evidence from a large community-based study. JAMA Intern Med. 2014; 174:32–9.
Article28. Medici BB, Nygaard B, la Cour JL, Grand MK, Siersma V, Nicolaisdottir DR, et al. Changes in prescription routines for treating hypothyroidism between 2001 and 2015: an observational study of 929,684 primary care patients in Copenhagen. Thyroid. 2019; 29:910–9.
Article29. de Jong NW, Baljet GM. Use of T4, T4 + T3, and T3 in the Dutch population in the period 2005–2011. Eur Thyroid J. 2012; 1:135–6.
Article30. Michaelsson LF, Medici BB, la Cour JL, Selmer C, Roder M, Perrild H, et al. Treating hypothyroidism with thyroxine/triiodothyronine combination therapy in Denmark: following guidelines or following trends? Eur Thyroid J. 2015; 4:174–80.
Article31. Burch HB, Burman KD, Cooper DS, Hennessey JV. A 2013 survey of clinical practice patterns in the management of primary hypothyroidism. J Clin Endocrinol Metab. 2014; 99:2077–85.
Article32. Jonklaas J, Tefera E, Shara N. Prescribing therapy for hypothyroidism: influence of physician characteristics. Thyroid. 2019; 29:44–52.
Article33. Negro R, Attanasio R, Nagy EV, Papini E, Perros P, Hegedus L. Use of thyroid hormones in hypothyroid and euthyroid patients: the 2019 Italian survey. Eur Thyroid J. 2020; 9:25–31.
Article34. Riis KR, Frolich JS, Hegedus L, Negro R, Attanasio R, Nagy EV, et al. Use of thyroid hormones in hypothyroid and euthyroid patients: a 2020 THESIS questionnaire survey of members of the Danish Endocrine Society. J Endocrinol Invest. 2021; 44:2435–44.
Article35. Niculescu DA, Attanasio R, Hegedus L, Nagy EV, Negro R, Papini E, et al. Use of thyroid hormones in hypothyroid and euthyroid patients: a Thesis* questionnaire survey of Romanian physicians *Thesis: treatment of hypothyroidism in Europe by specialists: an international survey. Acta Endocrinol (Buchar). 2020; 16:462–9.
Article36. Bednarczuk T, Attanasio R, Hegedus L, Nagy EV, Negro R, Papini E, et al. Use of thyroid hormones in hypothyroid and euthyroid patients: a Thesis* questionnaire survey of Polish physicians. *Thesis: treatment of hypothyroidism in Europe by specialists. An international survey. Endokrynol Pol. 2021; 72:357–65.
Article37. Borissova AMI, Boyanov MA, Attanasio R, Hegedus L, Nagy E, Negro R, et al. Use of thyroid hormones in hypothyroid and euthyroid patients: a THESIS* questionnaire survey of Bulgarian physicians. Endocrinologia. 2020; 25:299–309.38. Razvi S, Mrabeti S, Luster M. Managing symptoms in hypothyroid patients on adequate levothyroxine: a narrative review. Endocr Connect. 2020; 9:R241–50.
Article39. Carle A, Pedersen IB, Knudsen N, Perrild H, Ovesen L, Laurberg P. Hypothyroid symptoms and the likelihood of overt thyroid failure: a population-based case-control study. Eur J Endocrinol. 2014; 171:593–602.
Article40. Peterson SJ, Cappola AR, Castro MR, Dayan CM, Farwell AP, Hennessey JV, et al. An online survey of hypothyroid patients demonstrates prominent dissatisfaction. Thyroid. 2018; 28:707–21.
Article41. Michaelsson LF, la Cour JL, Medici BB, Watt T, Faber J, Nygaard B. Levothyroxine/liothyronine combination therapy and quality of life: is it all about weight loss? Eur Thyroid J. 2018; 7:243–50.
Article42. Akirov A, Fazelzad R, Ezzat S, Thabane L, Sawka AM. A systematic review and meta-analysis of patient preferences for combination thyroid hormone treatment for hypothyroidism. Front Endocrinol (Lausanne). 2019; 10:477.
Article43. Mitchell AL, Hegedus L, Zarkovic M, Hickey JL, Perros P. Patient satisfaction and quality of life in hypothyroidism: an online survey by the British thyroid foundation. Clin Endocrinol (Oxf). 2021; 94:513–20.
Article44. Perros P, Van Der Feltz-Cornelis C, Papini E, Nagy EV, Weetman AP, Hegedus L. The enigma of persistent symptoms in hypothyroid patients treated with levothyroxine: a narrative review. Clin Endocrinol (Oxf). 2021. Mar. 30. [Epub]. https://doi.org/10.1111/cen.14473 .
Article45. Gullo D, Latina A, Frasca F, Le Moli R, Pellegriti G, Vigneri R. Levothyroxine monotherapy cannot guarantee euthyroidism in all athyreotic patients. PLoS One. 2011; 6:e22552.
Article46. Jo S, Fonseca TL, Bocco BMLC, Fernandes GW, McAninch EA, Bolin AP, et al. Type 2 deiodinase polymorphism causes ER stress and hypothyroidism in the brain. J Clin Invest. 2019; 129:230–45.
Article47. Carle A, Faber J, Steffensen R, Laurberg P, Nygaard B. Hypothyroid patients encoding combined MCT10 and DIO2 gene polymorphisms may prefer L-T3 + L-T4 combination treatment: data using a blind, randomized, clinical study. Eur Thyroid J. 2017; 6:143–51.48. Ito M, Miyauchi A, Hisakado M, Yoshioka W, Ide A, Kudo T, et al. Biochemical markers reflecting thyroid function in athyreotic patients on levothyroxine monotherapy. Thyroid. 2017; 27:484–90.
Article49. Peterson SJ, McAninch EA, Bianco AC. Is a normal TSH synonymous with “euthyroidism” in levothyroxine monotherapy? J Clin Endocrinol Metab. 2016; 101:4964–73.
Article50. Fitzgerald SP, Bean NG, Falhammar H, Tuke J. Clinical parameters are more likely to be associated with thyroid hormone levels than with thyrotropin levels: a systematic review and meta-analysis. Thyroid. 2020; 30:1695–709.
Article51. Stott DJ, Rodondi N, Kearney PM, Ford I, Westendorp RGJ, Mooijaart SP, et al. Thyroid hormone therapy for older adults with subclinical hypothyroidism. N Engl J Med. 2017; 376:2534–44.52. Feller M, Snel M, Moutzouri E, Bauer DC, de Montmollin M, Aujesky D, et al. Association of thyroid hormone therapy with quality of life and thyroid-related symptoms in patients with subclinical hypothyroidism: a systematic review and meta-analysis. JAMA. 2018; 320:1349–59.
Article53. Mooijaart SP, Du Puy RS, Stott DJ, Kearney PM, Rodondi N, Westendorp RGJ, et al. Association between levothyroxine treatment and thyroid-related symptoms among adults aged 80 years and older with subclinical hypothyroidism. JAMA. 2019; 322:1977–86.
Article54. Wildisen L, Feller M, Del Giovane C, Moutzouri E, Du Puy RS, Mooijaart SP, et al. Effect of levothyroxine therapy on the development of depressive symptoms in older adults with subclinical hypothyroidism: an ancillary study of a randomized clinical trial. JAMA Netw Open. 2021; 4:e2036645.55. Bekkering GE, Agoritsas T, Lytvyn L, Heen AF, Feller M, Moutzouri E, et al. Thyroid hormones treatment for subclinical hypothyroidism: a clinical practice guideline. BMJ. 2019; 365:l2006.
Article56. Burgos N, Toloza FJK, Singh Ospina NM, Brito JP, Salloum RG, Hassett LC, et al. Clinical outcomes after discontinuation of thyroid hormone replacement: a systematic review and meta-analysis. Thyroid. 2021; 31:740–51.
Article57. Boelaert K, Newby PR, Simmonds MJ, Holder RL, Carr-Smith JD, Heward JM, et al. Prevalence and relative risk of other autoimmune diseases in subjects with autoimmune thyroid disease. Am J Med. 2010; 123:183.
Article58. Rotondi M, Leporati P, La Manna A, Pirali B, Mondello T, Fonte R, et al. Raised serum TSH levels in patients with morbid obesity: is it enough to diagnose subclinical hypothyroidism? Eur J Endocrinol. 2009; 160:403–8.
Article59. Valdes S, Maldonado-Araque C, Lago-Sampedro A, Lillo-Munoz JA, Garcia-Fuentes E, Perez-Valero V, et al. Reference values for TSH may be inadequate to define hypothyroidism in persons with morbid obesity: Di@bet.es study. Obesity (Silver Spring). 2017; 25:788–93.
Article60. van Hulsteijn LT, Pasquali R, Casanueva F, Haluzik M, Ledoux S, Monteiro MP, et al. Prevalence of endocrine disorders in obese patients: systematic review and meta-analysis. Eur J Endocrinol. 2020; 182:11–21.
Article61. Kok P, Roelfsema F, Langendonk JG, Frolich M, Burggraaf J, Meinders AE, et al. High circulating thyrotropin levels in obese women are reduced after body weight loss induced by caloric restriction. J Clin Endocrinol Metab. 2005; 90:4659–63.
Article62. Pasquali R, Casanueva F, Haluzik M, van Hulsteijn L, Ledoux S, Monteiro MP, et al. European Society of Endocrinology clinical practice guideline: endocrine work-up in obesity. Eur J Endocrinol. 2020; 182:G1–32.
Article63. Dew R, King K, Okosieme OE, Pearce SH, Donovan G, Taylor PN, et al. Attitudes and perceptions of health professionals towards management of hypothyroidism in general practice: a qualitative interview study. BMJ Open. 2018; 8:e019970.
Article64. American Psychiatric Association, Division of Research. Highlights of changes from DSM-IV to DSM-5: somatic symptom and related disorders. Focus. 2013; 11:525–7.65. Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: classification and criteria changes. World Psychiatry. 2013; 12:92–8.
Article66. van der Feltz-Cornelis CM, van Houdenhove B. DSM-5: from ‘somatoform disorders’ to ‘somatic symptom and related disorders’. Tijdschr Psychiatr. 2014; 56:182–6.67. Watt T, Hegedus L, Bjorner JB, Groenvold M, Bonnema SJ, Rasmussen AK, et al. Is thyroid autoimmunity per se a determinant of quality of life in patients with autoimmune hypothyroidism? Eur Thyroid J. 2012; 1:186–92.
Article68. Siegmann EM, Muller HHO, Luecke C, Philipsen A, Kornhuber J, Gromer TW. Association of depression and anxiety disorders with autoimmune thyroiditis: a systematic review and meta-analysis. JAMA Psychiatry. 2018; 75:577–84.
Article69. Guldvog I, Reitsma LC, Johnsen L, Lauzike A, Gibbs C, Carlsen E, et al. Thyroidectomy versus medical management for euthyroid patients with Hashimoto disease and persisting symptoms: a randomized trial. Ann Intern Med. 2019; 170:453–64.
Article70. Groenewegen KL, Mooij CF, van Trotsenburg ASP. Persisting symptoms in patients with Hashimoto’s disease despite normal thyroid hormone levels: does thyroid autoimmunity play a role? A systematic review. J Transl Autoimmun. 2021; 4:100101.
Article71. Rezaei S, Abedi P, Maraghi E, Hamid N, Rashidi H. The effectiveness of cognitive-behavioral therapy on quality of life in women with hypothyroidism in the reproductive age: a randomized controlled trial. Thyroid Res. 2020; 13:6.72. Verdurmen MJ, Videler AC, Kamperman AM, Khasho D, van der Feltz-Cornelis CM. Cognitive behavioral therapy for somatic symptom disorders in later life: a prospective comparative explorative pilot study in two clinical populations. Neuropsychiatr Dis Treat. 2017; 13:2331–9.
Article73. Rief W, Burton C, Frostholm L, Henningsen P, Kleinstauber M, Kop WJ, et al. Core outcome domains for clinical trials on somatic symptom disorder, bodily distress disorder, and functional somatic syndromes: European network on somatic symptom disorders recommendations. Psychosom Med. 2017; 79:1008–15.
Article74. van der Feltz-Cornelis CM, van Oppen P, Ader HJ, van Dyck R. Randomised controlled trial of a collaborative care model with psychiatric consultation for persistent medically unexplained symptoms in general practice. Psychother Psychosom. 2006; 75:282–9.
Article75. Jonklaas J, Bianco AC, Cappola AR, Celi FS, Fliers E, Heuer H, et al. Evidence-based use of levothyroxine/liothyronine combinations in treating hypothyroidism: a consensus document. Eur Thyroid J. 2021; 10:10–38.
Article76. McAninch EA, Jo S, Preite NZ, Farkas E, Mohacsik P, Fekete C, et al. Prevalent polymorphism in thyroid hormone-activating enzyme leaves a genetic fingerprint that underlies associated clinical syndromes. J Clin Endocrinol Metab. 2015; 100:920–33.
Article77. Porcelli T, Salvatore D. Targeting the right population for T3 + T4 combined therapy: where are we now and where to next? Endocrine. 2020; 69:244–8.
Article78. Wouters HJ, van Loon HC, van der Klauw MM, Elderson MF, Slagter SN, Kobold AM, et al. No effect of the Thr92Ala polymorphism of deiodinase-2 on thyroid hormone parameters, health-related quality of life, and cognitive functioning in a large population-based cohort study. Thyroid. 2017; 27:147–55.
Article79. Asvold BO, Vatten LJ, Bjoro T. Changes in the prevalence of hypothyroidism: the HUNT Study in Norway. Eur J Endocrinol. 2013; 169:613–20.
Article80. Celi FS, Zemskova M, Linderman JD, Babar NI, Skarulis MC, Csako G, et al. The pharmacodynamic equivalence of levothyroxine and liothyronine: a randomized, double blind, cross-over study in thyroidectomized patients. Clin Endocrinol (Oxf). 2010; 72:709–15.
Article81. Pilo A, Iervasi G, Vitek F, Ferdeghini M, Cazzuola F, Bianchi R. Thyroidal and peripheral production of 3,5,3’-triiodothyronine in humans by multicompartmental analysis. Am J Physiol. 1990; 258(4 Pt 1):E715–26.
Article82. Perros P, Nirantharakumar K, Hegedus L. Recent evidence sets therapeutic targets for levothyroxine-treated patients with primary hypothyroidism based on risk of death. Eur J Endocrinol. 2021; 184:C1–3.
Article83. DiStefano J 3rd, Jonklaas J. Predicting optimal combination LT4 + LT3 therapy for hypothyroidism based on residual thyroid function. Front Endocrinol (Lausanne). 2019; 10:746.
Article84. Winther KH, Cramon P, Watt T, Bjorner JB, Ekholm O, Feldt-Rasmussen U, et al. Disease-specific as well as generic quality of life is widely impacted in autoimmune hypothyroidism and improves during the first six months of levothyroxine therapy. PLoS One. 2016; 11:e0156925.
Article85. Watt T, Barbesino G, Bjorner JB, Bonnema SJ, Bukvic B, Drummond R, et al. Cross-cultural validity of the thyroid-specific quality-of-life patient-reported outcome measure, ThyPRO. Qual Life Res. 2015; 24:769–80.
Article86. Tariq A, Wert Y, Cheriyath P, Joshi R. Effects of long-term combination LT4 and LT3 therapy for improving hypothyroidism and overall quality of life. South Med J. 2018; 111:363–9.
Article87. Leese GP, Soto-Pedre E, Donnelly LA. Liothyronine use in a 17 year observational population-based study: the tears study. Clin Endocrinol (Oxf). 2016; 85:918–25.88. Idrees T, Palmer S, Maciel RMB, Bianco AC. Liothyronine and desiccated thyroid extract in the treatment of hypothyroidism. Thyroid. 2020; 30:1399–413.
Article89. Planck T, Hedberg F, Calissendorff J, Nilsson A. Liothyronine use in hypothyroidism and its effects on cancer and mortality. Thyroid. 2021; 31:732–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- T3 and T4 Responses to the Amygdaloid Electrical Stimulation and Coagulation
- The effect of the combination therapy with antithyroid drug and thyroxine in Graves' disease
- Factors Influencing Peripheral Conversion of Thyroxine to Tri-Iodothyronine in Athyreotic Individuals during Levothyroxine Replacement
- Anesthetic experience in a clinically euthyroid patient with hyperthyroxinemia and suspected impairment of T4 to T3 conversion: a case report
- Differential Diagnostic Value of Total T3/Free T4 Ratio in Graves' Disease and Painless Thyroiditis Presenting Thyrotoxicosis