Neonatal Med.
2021 Aug;28(3):133-138. 10.5385/nm.2021.28.3.133.
Autosomal Recessive Malignant Infantile Osteopetrosis Associated with a TCIRG1 Mutation: A Case Report of a Neonate Presenting with Hypocalcemia in South Korea
- Affiliations
-
- 1Department of Pediatrics, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- 2Department of Pediatrics, Sungae Medical Foundation, Seoul, Korea
- 3Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2519776
- DOI: http://doi.org/10.5385/nm.2021.28.3.133
Abstract
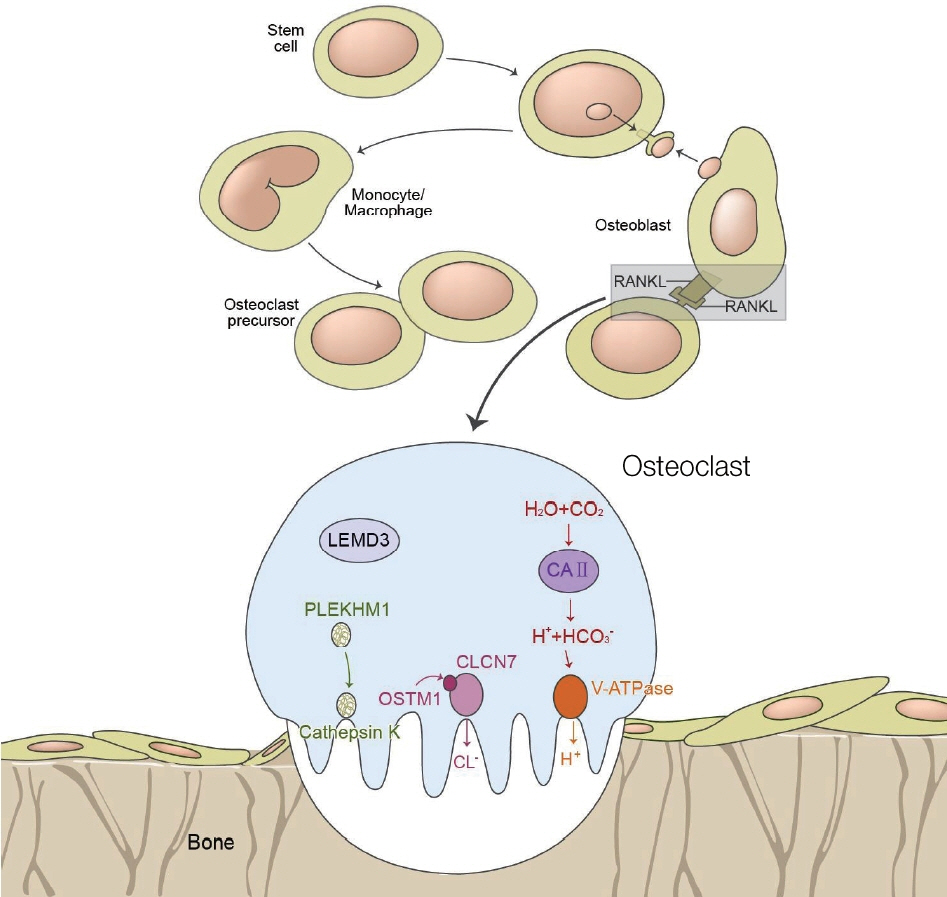
- Osteopetrosis refers to a group of genetic skeletal disorders characterized by osteosclerosis and fragile bones. Osteopetrosis can be classified into autosomal dominant, autosomal recessive, or X-linked forms, which might differ in clinical characteristics and disease severity. Autosomal recessive osteopetrosis, also known as malignant osteopetrosis, has an earlier onset, more serious clinical symptoms, and is usually fatal. We encountered a 1-day-old girl who was born full-term via vaginal delivery, which was complicated by meconium-stained amniotic fluid, cephalo-pelvic disproportion, and nuchal cord. Routine neonatal care was provided, in addition to blood tests and chest radiography to screen for sepsis, as well as skull radiography to rule out head injuries. Initial blood tests revealed hypocalcemia, which persisted on follow-up tests the next day. Radiographic examinations revealed diffusely increased bone density and a "space alien" appearance of the skull. Based on radiographic and laboratory findings, the infantile form of osteopetrosis was suspected and genetic testing for identification of the responsible gene. Eventually, a heterozygous mutation of the T cell immune regulator 1, ATPase H+ transporting V0 subunit a3 (TCIRG1) gene (c.292C>T) was identified, making this the first reported case of neonatal-onset malignant osteopetrosis with TCIRG1 mutation in South Korea. Early-onset hypocalcemia is common and usually results from prematurity, fetal growth restriction, maternal diabetes, perinatal asphyxia, and physiologic hypoparathyroidism. However, if hypocalcemia persists, we recommend considering 'infantile of osteopetrosis' as a rare cause of neonatal hypocalcemia and performing radiographic examinations to establish the diagnosis.
Keyword
Figure
Reference
-
1. Stark Z, Savarirayan R. Osteopetrosis. Orphanet J Rare Dis. 2009; 4:5.2. Aker M, Rouvinski A, Hashavia S, Ta-Shma A, Shaag A, Zenvirt S, et al. An SNX10 mutation causes malignant osteopetrosis of infancy. J Med Genet. 2012; 49:221–6.3. Palagano E, Blair HC, Pangrazio A, Tourkova I, Strina D, Angius A, et al. Buried in the middle but guilty: intronic mutations in the TCIRG1 gene cause human autosomal recessive osteopetrosis. J Bone Miner Res. 2015; 30:1814–21.4. Pangrazio A, Caldana ME, Lo Iacono N, Mantero S, Vezzoni P, Villa A, et al. Autosomal recessive osteopetrosis: report of 41 novel mutations in the TCIRG1 gene and diagnostic implications. Osteoporos Int. 2012; 23:2713–8.5. Sobacchi C, Pangrazio A, Lopez AG, Gomez DP, Caldana ME, Susani L, et al. As little as needed: the extraordinary case of a mild recessive osteopetrosis owing to a novel splicing hypomorphic mutation in the TCIRG1 gene. J Bone Miner Res. 2014; 29:1646–50.6. Kornak U, Kasper D, Bosl MR, Kaiser E, Schweizer M, Schulz A, et al. Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001; 104:205–15.7. Frattini A, Orchard PJ, Sobacchi C, Giliani S, Abinun M, Mattsson JP, et al. Defects in TCIRG1 subunit of the vacuolar proton pump are responsible for a subset of human autosomal recessive osteopetrosis. Nat Genet. 2000; 25:343–6.8. Kornak U, Schulz A, Friedrich W, Uhlhaas S, Kremens B, Voit T, et al. Mutations in the a3 subunit of the vacuolar H(+)-ATPase cause infantile malignant osteopetrosis. Hum Mol Genet. 2000; 9:2059–63.9. Li YP, Chen W, Liang Y, Li E, Stashenko P. Atp6i-deficient mice exhibit severe osteopetrosis due to loss of osteoclast-mediated extracellular acidification. Nat Genet. 1999; 23:447–51.10. Sobacchi C, Frattini A, Orchard P, Porras O, Tezcan I, Andolina M, et al. The mutational spectrum of human malignant autosomal recessive osteopetrosis. Hum Mol Genet. 2001; 10:1767–73.11. Steward CG. Neurological aspects of osteopetrosis. Neuropathol Appl Neurobiol. 2003; 29:87–97.12. Kasper D, Planells-Cases R, Fuhrmann JC, Scheel O, Zeitz O, Ruether K, et al. Loss of the chloride channel ClC-7 leads to lysosomal storage disease and neurodegeneration. EMBO J. 2005; 24:1079–91.13. Pangrazio A, Fasth A, Sbardellati A, Orchard PJ, Kasow KA, Raza J, et al. SNX10 mutations define a subgroup of human autosomal recessive osteopetrosis with variable clinical severity. J Bone Miner Res. 2013; 28:1041–9.14. Doffinger R, Smahi A, Bessia C, Geissmann F, Feinberg J, Durandy A, et al. X-linked anhidrotic ectodermal dysplasia with immunodeficiency is caused by impaired NF-kappaB signaling. Nat Genet. 2001; 27:277–85.15. Tolar J, Teitelbaum SL, Orchard PJ. Osteopetrosis. N Engl J Med. 2004; 351:2839–49.16. Del Fattore A, Cappariello A, Teti A. Genetics, pathogenesis and complications of osteopetrosis. Bone. 2008; 42:19–29.17. Kim JY, Lee HS, Kang IS. Preimplantation genetic diagnosis. J Korean Med Assoc. 2015; 58:979–88.18. Wu CC, Econs MJ, DiMeglio LA, Insogna KL, Levine MA, Orchard PJ, et al. Diagnosis and management of osteopetrosis: consensus guidelines from the Osteopetrosis Working Group. J Clin Endocrinol Metab. 2017; 102:3111–23.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cytomegalovirus Infection in a Neonate with Osteopetrosis
- Analysis of Inheritance in Infantile Nystagmus
- Newly Detected PKHD1 Gene Mutation in a Newborn with Fatal Autosomal Recessive Polycystic Kidney Disease
- De novo a novel variant of CaSR gene in a neonate with congenital hypoparathyroidism
- Autosomal Recessive Polycystic Kidney Disease Confirmed to PKHD1 Gene Mutation: A Case of PKHD1 Gene Mutation