Endocrinol Metab.
2021 Aug;36(4):725-736. 10.3803/EnM.2021.1164.
The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
- Affiliations
-
- 1Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Biomedical Sciences, Seoul National University Graduate School, Seoul, Korea
- 3Cancer Research Institute, Seoul National University, Seoul, Korea
- 4Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 5Integrated Major in Innovative Medical Science, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2519660
- DOI: http://doi.org/10.3803/EnM.2021.1164
Abstract
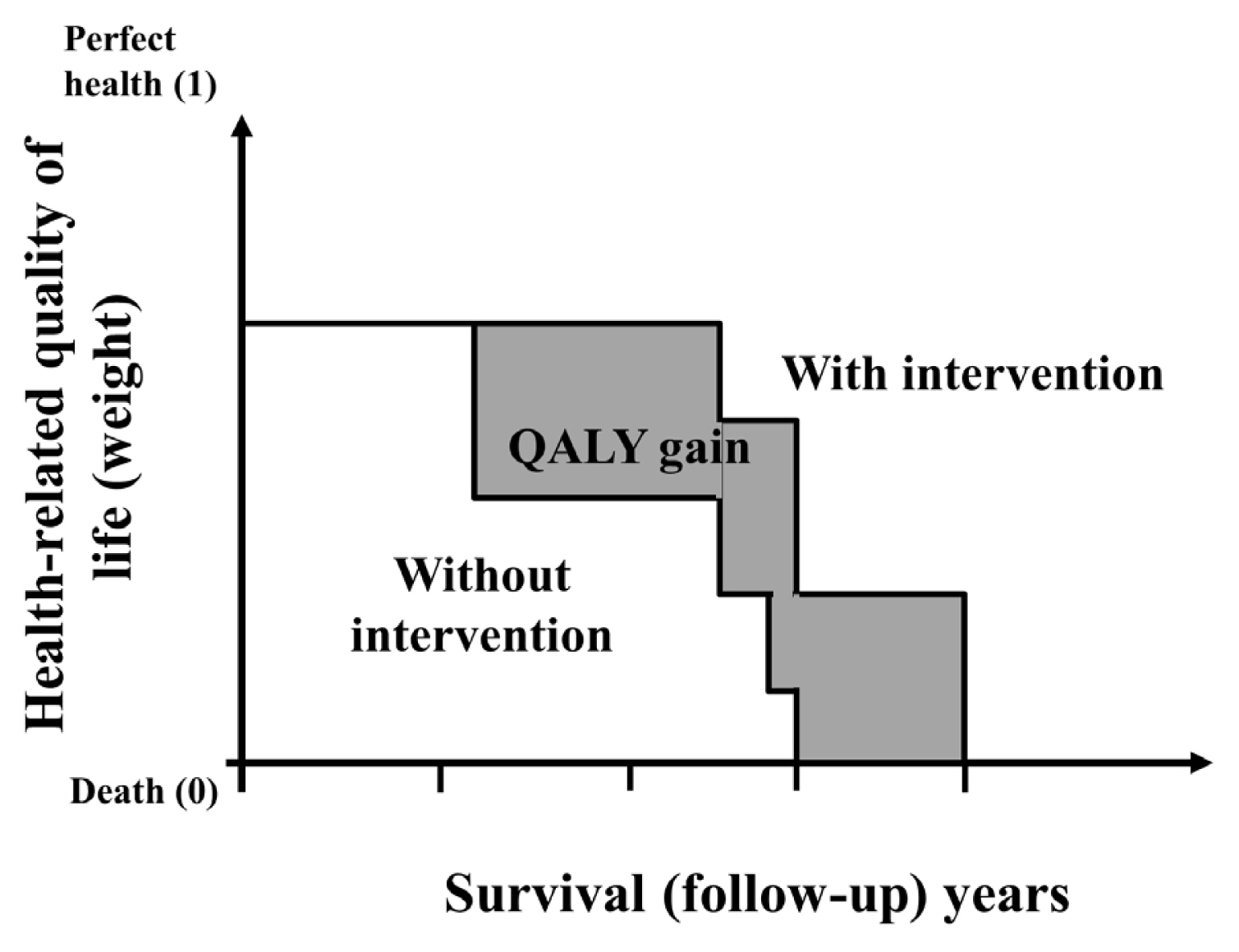
- Economic evaluation is a type of comparative analysis between interventions in terms of both their resource use and health outcomes. Due to the good prognosis of thyroid cancer (TC), the socioeconomic burden of TC patients post-diagnosis is increasing. Therefore, economic evaluation studies focusing on TC are recommended. This study aimed to describe the concept and methods of economic evaluation and reviewed previous TC studies. Several previous studies compared the costs of interventions or evaluated recurrence, complications, or quality of life as measures of their effectiveness. Regarding costs, most studies focused on direct costs and applied hypothetical models. Cost-minimization analysis should be distinguished from simple cost analysis. Furthermore, due to the universality of the term “cost-effectiveness analysis” (CEA), several studies have not distinguished CEA from cost-utility analysis; this point needs to be considered in future research. Cost-benefit analyses have not been conducted in previous TC research. Since TC has a high survival rate and good prognosis, the need for economic evaluations has recently been pointed out. Therefore, correct concepts and methods are needed to obtain clear economic evaluation results. On this basis, it will be possible to provide appropriate guidelines for TC treatment and management in the future.
Figure
Cited by 2 articles
-
A Systematic Review of Economic Evaluation of Thyroid Cancer
Mijin Kim, Woojin Lim, Kyungsik Kim, Ja Seong Bae, Byung Joo Lee, Bon Seok Koo, Eun Kyung Lee, Eu Jeong Ku, June Young Choi, Bo Hyun Kim, Sue K. Park
Int J Thyroidol. 2022;15(2):74-104. doi: 10.11106/ijt.2022.15.2.74.Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
Endocrinol Metab. 2024;39(2):310-323. doi: 10.3803/EnM.2023.1870.
Reference
-
1. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.
Article2. Korea Central Cancer Registry, National Cancer Center, Korea. Annual report of cancer statistics in Korea in 2018 [Internet]. Goyang: National Cancer Center;2021. [cited 2021 Aug 10]. Available from: https://ncc.re.kr/cancerStatsView.ncc?bbsnum=558&searchKey=total&searchValue=&pageNum=1 .3. International Agency for Research on Cancer. World Health Organization. Cancer today, Globocan 2020 [Internet]. Lyon: IARC;2020. [cited 2021 Aug 10]. Available from: https://gco.iarc.fr/today/home .4. Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”: screening and overdiagnosis. N Engl J Med. 2014; 371:1765–7.
Article5. Folland S, Goodman AC, Stano M. The economics of health and health care. New York: Macmillan Publishing Company;1993.6. Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009; 24:63–71.
Article7. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed. Oxford;Oxford University Press;2015.8. Haddix AC, Teutsch SM, Corso PS. Prevention effectiveness: a guide to decision analysis and economic evaluation. 2nd ed. New York: Oxford University Press;2003. Chapter 8:Cost-effectiveness analysis. p. 156–77.9. Brown J. Economic evaluation of cancer treatments: a review of the methods. Clin Oncol (R Coll Radiol). 1999; 11:78–83.
Article10. Neumann PJ. Costing and perspective in published cost-effectiveness analysis. Med Care. 2009; 47(7 Suppl 1):S28–32.
Article11. Ngorsuraches S. Defining types of economic evaluation. J Med Assoc Thai. 2008; 91(Suppl 2):S21–7.12. Vohora D, Singh G. Pharmaceutical medicine and translational clinical research. Boston: Academic Press;2018. Chapter 33:Pharmacoeconomics in healthcare. p. 465–72.13. Phillips C, Thompson G. What is cost-effectiveness? Kent: Hayward Medical Communication;2001.14. McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. Pharmacoeconomics. 2008; 26:733–44.15. Wang TS, Cheung K, Mehta P, Roman SA, Walker HD, Sosa JA. To stimulate or withdraw?: a cost-utility analysis of recombinant human thyrotropin versus thyroxine withdrawal for radioiodine ablation in patients with low-risk differentiated thyroid cancer in the United States. J Clin Endocrinol Metab. 2010; 95:1672–80.16. Donovan PJ, McLeod DS, Little R, Gordon L. Cost-utility analysis comparing radioactive iodine, anti-thyroid drugs and total thyroidectomy for primary treatment of Graves’ disease. Eur J Endocrinol. 2016; 175:595–603.
Article17. Al-Qurayshi Z, Farag M, Shama MA, Ibraheem K, Randolph GW, Kandil E. Total thyroidectomy versus lobectomy in small nodules suspicious for papillary thyroid cancer: cost-effectiveness analysis. Laryngoscope. 2020; 130:2922–6.
Article18. Bergmo TS. How to measure costs and benefits of ehealth interventions: an overview of methods and frameworks. J Med Internet Res. 2015; 17:e254.
Article19. Transportation Benefit-Cost Analysis. Benefit-cost ratio [Internet]. Transportation Benefit-Cost Analysis. 2021. [cited 2021 Aug 10]. Available from: http://bca.transportationeconomics.org/types-of-measures/benefit-cost-ratio .20. Sculpher MJ, Price M. Measuring costs and consequences in economic evaluation in asthma. Respir Med. 2003; 97:508–20.
Article21. Yousefi M, Assari Arani A, Sahabi B, Kazemnejad A, Fazaeli S. Household health costs: direct, indirect and intangible. Iran J Public Health. 2014; 43:202–9.22. Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014; 20:327–37.
Article23. Spinks J. Economic considerations of complementary and alternative medicine (CAM) use in Australia [dissertation]. Clayton: Monash University;2017. https://doi.org/10.4225/03/58b3a70ad11a7 .
Article24. National Library of Medicine. National Information Center on Health Services Research and Health Care Technology (NICHSR): Health Economics Information Resources: A Self-Study Course [Internet]. Bethesda: National Library of Medicine;2016. [cited 2021 Aug 10]. Available from: https://www.nlm.nih.gov/nichsr/edu/healthecon/04_he_07.html .25. Prieto L, Sacristan JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes. 2003; 1:80.26. Lang BH, Wong CK. A cost-minimization analysis comparing total thyroidectomy alone and total thyroidectomy with prophylactic central neck dissection in clinically nodal-negative papillary thyroid carcinoma. Ann Surg Oncol. 2014; 21:416–25.
Article27. Shrime MG, Goldstein DP, Seaberg RM, Sawka AM, Rotstein L, Freeman JL, et al. Cost-effective management of low-risk papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 2007; 133:1245–53.
Article28. Guo K, Zheng X, Li D, Wu Y, Ji Q, Wang Z. Cost-effectiveness analysis in papillary thyroid carcinoma patients with different neck dissection strategy: a retrospective cohort study. Int J Surg. 2018; 50:1–5.
Article29. Walgama E, Randolph GW, Lewis C, Tolley N, Sacks W, Chen Y, et al. Cost-effectiveness of fiberoptic laryngoscopy prior to total thyroidectomy for low-risk thyroid cancer patients. Head Neck. 2020; 42:2593–601.
Article30. Kuo EJ, Wu JX, Zanocco KA. Cost effectiveness of immediate biopsy versus surveillance of intermediate-suspicion thyroid nodules. Surgery. 2018; 164:1330–5.
Article31. Lang BH, Wong CK, Chan CT. Initial attributable cost and economic burden of clinically-relevant differentiated thyroid cancer: a health care service provider perspective. Eur J Surg Oncol. 2015; 41:758–65.
Article32. Kim SY, Kim SM, Chang H, Kim BW, Lee YS, Kwon SS, et al. Cost for treatment and follow-up of thyroid cancer increases according to the severity of disease. Head Neck. 2019; 41:2376–9.
Article33. Lin JF, Jonker PK, Cunich M, Sidhu SB, Delbridge LW, Glover AR, et al. Surgery alone for papillary thyroid microcarcinoma is less costly and more effective than long term active surveillance. Surgery. 2020; 167:110–6.
Article34. Oda H, Miyauchi A, Ito Y, Sasai H, Masuoka H, Yabuta T, et al. Comparison of the costs of active surveillance and immediate surgery in the management of low-risk papillary microcarcinoma of the thyroid. Endocr J. 2017; 64:59–64.
Article35. Boltz MM, Hollenbeak CS, Schaefer E, Goldenberg D, Saunders BD. Attributable costs of differentiated thyroid cancer in the elderly Medicare population. Surgery. 2013; 154:1363–70.
Article36. Lubitz CC, Kong CY, McMahon PM, Daniels GH, Chen Y, Economopoulos KP, et al. Annual financial impact of well-differentiated thyroid cancer care in the United States. Cancer. 2014; 120:1345–52.
Article37. Lang BH, Wong CK. A cost-effectiveness comparison between early surgery and non-surgical approach for incidental papillary thyroid microcarcinoma. Eur J Endocrinol. 2015; 173:367–75.
Article38. Lee L, How J, Tabah RJ, Mitmaker EJ. Cost-effectiveness of molecular testing for thyroid nodules with atypia of undetermined significance cytology. J Clin Endocrinol Metab. 2014; 99:2674–82.
Article39. Wilson L, Huang W, Chen L, Ting J, Cao V. Cost effectiveness of lenvatinib, sorafenib and placebo in treatment of radioiodine-refractory differentiated thyroid cancer. Thyroid. 2017; 27:1043–52.
Article40. Venkatesh S, Pasternak JD, Beninato T, Drake FT, Kluijfhout WP, Liu C, et al. Cost-effectiveness of active surveillance versus hemithyroidectomy for micropapillary thyroid cancer. Surgery. 2017; 161:116–26.
Article41. Zanocco K, Heller M, Elaraj D, Sturgeon C. Cost effectiveness of intraoperative pathology examination during diagnostic hemithyroidectomy for unilateral follicular thyroid neoplasms. J Am Coll Surg. 2013; 217:702–10.
Article42. Cleemput I, Neyt M, Thiry N, De Laet C, Leys M. Threshold values for cost-effectiveness in health care. Belgian Health Care Knowledge Centre. HTA reports. Brussels: KCE;2008. p. 88.43. Lohia S, Hanson M, Tuttle RM, Morris LG. Active surveillance for patients with very low-risk thyroid cancer. Laryngoscope Investig Otolaryngol. 2020; 5:175–82.
Article44. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.
Article45. Moon JH, Kim JH, Lee EK, Lee KE, Kong SH, Kim YK, et al. Study protocol of multicenter prospective cohort study of active surveillance on papillary thyroid microcarcinoma (MAeSTro). Endocrinol Metab (Seoul). 2018; 33:278–86.
Article46. Lee EK, Kang YE, Park YJ, Koo BS, Chung KW, Ku EJ, et al. A multicenter, randomized, controlled trial for assessing the usefulness of suppressing thyroid stimulating hormone target levels after thyroid lobectomy in low to intermediate risk thyroid cancer patients (MASTER): a study protocol. Endocrinol Metab (Seoul). 2021; 36:574–81.
Article