Int J Thyroidol.
2022 Nov;15(2):74-104. 10.11106/ijt.2022.15.2.74.
A Systematic Review of Economic Evaluation of Thyroid Cancer
- Affiliations
-
- 1Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan,
- 2Department of Preventive Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Biomedical Sciences, Seoul National University Graduate School, Seoul, Korea
- 4Cancer Research Institute, Seoul National University, Seoul, Korea
- 5Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 6Department of Otorhinolaryngology-Head and Neck Surgery, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 7Department of Otorhinolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- 8Center for Thyroid Cancer, National Cancer Center, Goyang, Korea
- 9Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea
- 10Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 11Integrated Major in Innovative Medical Science, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2536494
- DOI: http://doi.org/10.11106/ijt.2022.15.2.74
Abstract
- Background
This systematic review was conducted to identify and summarize key factors, including economic methods, topics, results, and indicators, within relevant economic evaluation research on thyroid cancer.
Materials and Methods
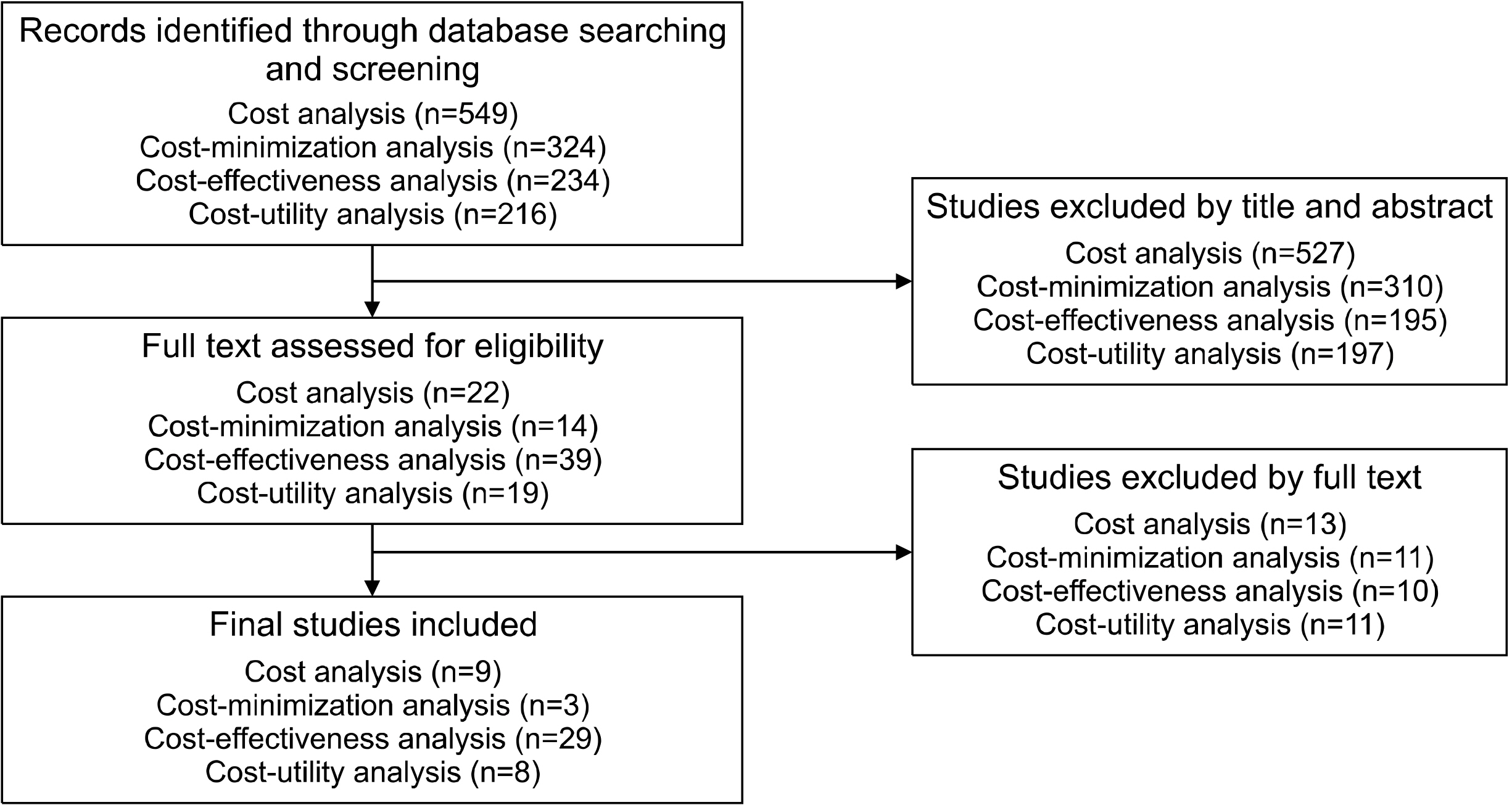
A literature search on the economic evaluation of thyroid cancer treatment was conducted using the MEDLINE database up to May 2021. Data on population, intervention, comparison, outcome, time, setting, and study design were extracted from each study. The economic evaluation method in each study was re-classified according to the theoretical criteria defined by the international economic evaluation guidelines.
Results
A total of 49 studies were included, involving cost analysis (CA, n=9), cost-minimization analysis (CMA, n=3), cost-effectiveness analysis (CEA, n=29), and cost-utility analysis (CUA, n=8). When CEA and CUA were classified as one method, the consistency between the methods of the reviewers based on the theoretical criteria and those from the original studies was 77% (95% confidence interval, 0.63-0.92). Most studies dealt with specific period-related controversial issues including comparison between treatment strategies, and cost-effectiveness of the prophylactic central neck dissection, molecular testing, and rhTSH. Contrasting results have been obtained when different economic evaluation methods were applied for the same topic (e.g., total thyroidectomy [TT] was more dominant than hemithyroidectomy [HT] in CEA, but HT was more dominant than TT in CUA), and different clinical and economic inputs were applied. All studies included direct medical costs, which were mostly derived from Medicare and input probabilities in each economic model, and utility scores for outcomes were mostly based on literature reviews. Few studies included non-medical direct costs and indirect costs.
Conclusion
Our systematic review provides information on how to design and proceed to overcome the limitations of existing studies and ensure validity.
Keyword
Figure
Reference
-
References
1. Siegel RL, Miller KD, Jemal A. 2018; Cancer statistics, 2018. CA Cancer J Clin. 68(1):7–30. DOI: 10.3322/caac.21442. PMID: 29313949.
Article2. Kitahara CM, Sosa JA. 2016; The changing incidence of thyroid cancer. Nat Rev Endocrinol. 12(11):646–53. DOI: 10.1038/nrendo.2016.110. PMID: 27418023.
Article3. Choi YM, Kim WG, Kwon H, Jeon MJ, Han M, Kim TY, et al. Changes in standardized mortality rates from thyroid cancer in Korea between 1985 and 2015: analysis of Korean national data. Cancer. 2017; 123(24):4808–14. DOI: 10.1002/cncr.30943. PMID: 28817188.
Article4. Yoon J, Park B. 2020; Factors associated with health behaviors in thyroid cancer survivors. J Cancer Prev. 25(3):173–80. DOI: 10.15430/JCP.2020.25.3.173. PMID: 33033711. PMCID: PMC7523035.
Article5. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. 2020; Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 52(2):335–50. DOI: 10.4143/crt.2020.206. PMID: 32178489. PMCID: PMC7176962.
Article6. Krajewska J, Kukulska A, Oczko-Wojciechowska M, Kotecka-Blicharz A, Drosik-Rutowicz K, Haras-Gil M, et al. 2020; Early diagnosis of low-risk papillary thyroid cancer results rather in overtreatment than a better survival. Front Endocrinol (Lausanne). 11:571421. DOI: 10.3389/fendo.2020.571421. PMID: 33123090. PMCID: PMC7573306.
Article7. Kim K, Kim M, Lim W, Kim BH, Park SK. 2021; The concept of economic evaluation and its application in thyroid cancer research. Endocrinol Metab (Seoul). 36(4):725–36. DOI: 10.3803/EnM.2021.1164. PMID: 34474512. PMCID: PMC8419602.
Article8. Bae JM. 2017; Strategies for appropriate patient-centered care to decrease the nationwide cost of cancers in Korea. J Prev Med Public Health. 50(4):217–27. DOI: 10.3961/jpmph.17.069. PMID: 28768400. PMCID: PMC5541273.
Article9. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2016; 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 26(1):1–133. DOI: 10.1089/thy.2015.0020. PMID: 26462967. PMCID: PMC4739132.
Article10. Tuttle RM. 2018; Controversial issues in thyroid cancer management. J Nucl Med. 59(8):1187–94. DOI: 10.2967/jnumed.117.192559. PMID: 29653980. PMCID: PMC6071505.
Article11. Lubitz CC, Kong CY, McMahon PM, Daniels GH, Chen Y, Economopoulos KP, et al. 2014; Annual financial impact of well-differentiated thyroid cancer care in the United States. Cancer. 120(9):1345–52. DOI: 10.1002/cncr.28562. PMID: 24481684. PMCID: PMC3999178.
Article12. Ngorsuraches S. 2008; Defining types of economic evaluation. J Med Assoc Thai. 91 Suppl 2:S21–7.13. Shrime MG, Goldstein DP, Seaberg RM, Sawka AM, Rotstein L, Freeman JL, et al. 2007; Cost-effective management of low-risk papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 133(12):1245–53. DOI: 10.1001/archotol.133.12.1245. PMID: 18086967.
Article14. Lang BH, Wong CKH. 2016; Lobectomy is a more cost-effective option than total thyroidectomy for 1 to 4 cm papillary thyroid carcinoma that do not possess clinically recognizable high-risk features. Ann Surg Oncol. 23(11):3641–52. DOI: 10.1245/s10434-016-5280-6. PMID: 27221359.
Article15. Al-Qurayshi Z, Farag M, Shama MA, Ibraheem K, Randolph GW, Kandil E. 2020; Total thyroidectomy versus lobectomy in small nodules suspicious for papillary thyroid cancer: cost-effectiveness analysis. Laryngoscope. 130(12):2922–6. DOI: 10.1002/lary.28634. PMID: 32239764.
Article16. Oda H, Miyauchi A, Ito Y, Sasai H, Masuoka H, Yabuta T, et al. 2017; Comparison of the costs of active surveillance and immediate surgery in the management of low-risk papillary microcarcinoma of the thyroid. Endocr J. 64(1):59–64. DOI: 10.1507/endocrj.EJ16-0381. PMID: 27667647.
Article17. Lin JF, Jonker PKC, Cunich M, Sidhu SB, Delbridge LW, Glover AR, et al. 2020; Surgery alone for papillary thyroid microcarcinoma is less costly and more effective than long term active surveillance. Surgery. 167(1):110–6. DOI: 10.1016/j.surg.2019.05.078. PMID: 31543327.
Article18. Lang BH, Wong CK. 2015; A cost-effectiveness comparison between early surgery and non-surgical approach for incidental papillary thyroid microcarcinoma. Eur J Endocrinol. 173(3):367–75. DOI: 10.1530/EJE-15-0454. PMID: 26104754.
Article19. Venkatesh S, Pasternak JD, Beninato T, Drake FT, Kluijfhout WP, Liu C, et al. 2017; Cost-effectiveness of active surveillance versus hemithyroidectomy for micropapillary thyroid cancer. Surgery. 161(1):116–26. DOI: 10.1016/j.surg.2016.06.076.
Article20. Lang BH, Wong CK. 2014; A cost-minimization analysis comparing total thyroidectomy alone and total thyroidectomy with prophylactic central neck dissection in clinically nodal-negative papillary thyroid carcinoma. Ann Surg Oncol. 21(2):416–25. DOI: 10.1245/s10434-013-3234-9.
Article21. Zanocco K, Elaraj D, Sturgeon C. 2013; Routine prophylactic central neck dissection for low-risk papillary thyroid cancer: a cost-effectiveness analysis. Surgery. 154(6):1148–55. discussion 54–5. DOI: 10.1016/j.surg.2013.06.016. PMID: 24383082.
Article22. Garcia A, Palmer BJ, Parks NA, Liu TH. 2014; Routine prophylactic central neck dissection for low-risk papillary thyroid cancer is not cost-effective. Clin Endocrinol (Oxf). 81(5):754–61. DOI: 10.1111/cen.12506. PMID: 24862564.
Article23. Wong CK, Lang BH. 2014; A cost-utility analysis for prophylactic central neck dissection in clinically nodal-negative papillary thyroid carcinoma. Ann Surg Oncol. 21(3):767–77. DOI: 10.1245/s10434-013-3398-3. PMID: 24276639.
Article24. Najafzadeh M, Marra CA, Lynd LD, Wiseman SM. 2012; Cost-effectiveness of using a molecular diagnostic test to improve preoperative diagnosis of thyroid cancer. Value Health. 15(8):1005–13. DOI: 10.1016/j.jval.2012.06.017. PMID: 23244801.
Article25. Lee L, How J, Tabah RJ, Mitmaker EJ. 2014; Cost-effectiveness of molecular testing for thyroid nodules with atypia of undetermined significance cytology. J Clin Endocrinol Metab. 99(8):2674–82. DOI: 10.1210/jc.2014-1219. PMID: 24684467.
Article26. Nicholson KJ, Roberts MS, McCoy KL, Carty SE, Yip L. 2019; Molecular testing versus diagnostic lobectomy in Bethesda III/IV thyroid nodules: a cost-effectiveness analysis. Thyroid. 29(9):1237–43. DOI: 10.1089/thy.2018.0779. PMID: 31407625. PMCID: PMC7366255.
Article27. Balentine CJ, Vanness DJ, Schneider DF. 2018; Cost-effectiveness of lobectomy versus genetic testing (Afirma(R)) for indeterminate thyroid nodules: considering the costs of surveillance. Surgery. 163(1):88–96. DOI: 10.1016/j.surg.2017.10.004. PMID: 29128178. PMCID: PMC5736452.
Article28. Borget I, Bonastre J, Catargi B, Deandreis D, Zerdoud S, Rusu D, et al. 2015; Quality of life and cost-effectiveness assessment of radioiodine ablation strategies in patients with thyroid cancer: results from the randomized phase III ESTIMABL trial. J Clin Oncol. 33(26):2885–92. DOI: 10.1200/JCO.2015.61.6722. PMID: 26240230.
Article29. Mernagh P, Suebwongpat A, Silverberg J, Weston A. 2010; Cost-effectiveness of using recombinant human thyroid-stimulating hormone before radioiodine ablation for thyroid cancer: the Canadian perspective. Value Health. 13(2):180–7. DOI: 10.1111/j.1524-4733.2009.00650.x. PMID: 19818064.
Article30. Mernagh P, Campbell S, Dietlein M, Luster M, Mazzaferri E, Weston AR. 2006; Cost-effectiveness of using recombinant human TSH prior to radioiodine ablation for thyroid cancer, compared with treating patients in a hypothyroid state: the German perspective. Eur J Endocrinol. 155(3):405–14. DOI: 10.1530/eje.1.02223. PMID: 16914594.
Article31. Vallejo JA, Muros MA. 2017; Cost-effectiveness of using recombinant human thyroid-stimulating hormone before radioiodine ablation for thyroid cancer treatment in Spanish hospitals. Rev Esp Med Nucl Imagen Mol. 36(6):362–70. DOI: 10.1016/j.remnie.2017.09.001.
Article32. Wang TS, Cheung K, Mehta P, Roman SA, Walker HD, Sosa JA. 2010; To stimulate or withdraw? A cost-utility analysis of recombinant human thyrotropin versus thyroxine withdrawal for radioiodine ablation in patients with low-risk differentiated thyroid cancer in the United States. J Clin Endocrinol Metab. 95(4):1672–80. DOI: 10.1210/jc.2009-1803. PMID: 20139234.33. Goldsmith LJ, Hutchison B, Hurley FJ. 2004. Economic evaluation across the four faces of prevention. Centre for Health Economics and Policy Analysis, McMaster University;Hamilton, Ontario:34. Sculpher MJ, Price M. 2003; Measuring costs and consequences in economic evaluation in asthma. Respir Med. 97(5):508–20. DOI: 10.1053/rmed.2002.1474. PMID: 12735668.
Article35. Wilson L, Huang W, Chen L, Ting J, Cao V. 2017; Cost effectiveness of lenvatinib, sorafenib and placebo in treatment of radioiodine-refractory differentiated thyroid cancer. Thyroid. 27(8):1043–52. DOI: 10.1089/thy.2016.0572. PMID: 28486081.
Article36. Zanocco K, Heller M, Elaraj D, Sturgeon C. 2013; Cost effectiveness of intraoperative pathology examination during diagnostic hemithyroidectomy for unilateral follicular thyroid neoplasms. J Am Coll Surg. 217(4):702–10. DOI: 10.1016/j.jamcollsurg.2013.05.008. PMID: 23810576.
Article37. Rocke DJ, Goldstein DP, de Almeida JR. 2016; A cost-utility analysis of recurrent laryngeal nerve monitoring in the setting of total thyroidectomy. JAMA Otolaryngol Head Neck Surg. 142(12):1199–205. DOI: 10.1001/jamaoto.2016.2860. PMID: 27737451.
Article38. Lee WS, Palmer BJ, Garcia A, Chong VE, Liu TH. 2014; BRAF mutation in papillary thyroid cancer: a cost-utility analysis of preoperative testing. Surgery. 156(6):1569–77. discussion 77–8. DOI: 10.1016/j.surg.2014.08.051. PMID: 25444226.
Article39. Leiker AJ, Yen TW, Cheung K, Evans DB, Wang TS. 2013; Cost analysis of thyroid lobectomy and intraoperative frozen section versus total thyroidectomy in patients with a cytologic diagnosis of "suspicious for papillary thyroid cancer". Surgery. 154(6):1307–13. discussion 13–4. DOI: 10.1016/j.surg.2013.06.031. PMID: 24238049.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Lymphovascular Invasion as a Prognostic Factor in Patients with Papillary Thyroid Cancer: a Systematic Review and Meta-Analysis
- Preoperative Staging of Well Differentiated Thyroid Cancer: US Is Enough?
- The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
- Clinical Factors Associated with Quality of Life in Patients with Thyroid Cancer
- Postoperative Surveillance of Thyroid Cancer: in View of US