Neurointervention.
2021 Jul;16(2):91-110. 10.5469/neuroint.2020.00339.
Factors Contributing to an Efficacious Endovascular Treatment for Acute Ischemic Stroke in Asian Population
- Affiliations
-
- 1Department of Neurology, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- 2Department of Neurology, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Department of Neurology, Keimyung University Dongsan Hospital, Kyemyung University School of Medicine, Daegu, Korea
- KMID: 2517734
- DOI: http://doi.org/10.5469/neuroint.2020.00339
Abstract
- Although randomized control trials about endovascular treatment (EVT) of emergent large vessel occlusion (LVO) have demonstrated the success of mechanical thrombectomy as the choice of treatment, a wide range of caveats remain unaddressed. Asian patients were rarely included in the trials, thereby raising the question of whether the treatment could be generalized. In addition, there remains a concern on the feasibility of the method with respect to its application against intracranial atherosclerosis (ICAS)-related LVO, frequently observed in the Asian population. It is important to include evidence on ICAS LVO from Asian countries in the future for a comprehensive understanding of LVO etiology. Besides the issues with EVT, prognostic concerns in diabetes patients, acute kidney injury following EVT, neuroprotective management against reperfusion injury, and other peri-EVT issues should be considered in clinical practice. In the current article, we present an in-depth review of the literature that revises information pertaining to such concerns.
Keyword
Figure
Cited by 1 articles
-
Clinical Manifestation and Radiologic Patterns of Spontaneous Cervicocephalic Dissection According to the Anatomic Location: A Single-Center Analysis in Korean Patients
Yunsun Song, Sang Ik Park, Pepi Budianto, Boseong Kwon, Dae Chul Suh
Neurointervention. 2022;17(2):78-86. doi: 10.5469/neuroint.2022.00143.
Reference
-
1. Lee JS, Lee SJ, Hong JM, Choi JW, Hong JH, Chang HW, et al. Temporal changes in care processes and outcomes for endovascular treatment of acute ischemic stroke: retrospective registry data from three Korean centers. Neurointervention. 2018; 13:2–12.
Article2. Lee SJ, Hong JM, Choi JW, Park JH, Park B, Kang DH, et al. Predicting endovascular treatment outcomes in acute vertebrobasilar artery occlusion: a model to aid patient selection from the Asian KR registry. Radiology. 2020; 294:628–637.3. Lee SJ, Hong JM, Choi JW, Kang DH, Kim YW, Kim YS, et al. CTA-based truncal-type occlusion is best matched with postprocedural fixed focal stenosis in vertebrobasilar occlusions. Front Neurol. 2019; 9:1195.
Article4. Lee JS, Lee SJ, Yoo JS, Hong JH, Kim CH, Kim YW, et al. Prognosis of acute intracranial atherosclerosis-related occlusion after endovascular treatment. J Stroke. 2018; 20:394–403.
Article5. Lee SJ, Hwang YH, Hong JM, Choi JW, Kang DH, Kim YW, et al. Predictors and prognoses of Willisian collateral failure during mechanical thrombectomy. Sci Rep. 2020; 10:20874.
Article6. Lee JS, Lee SJ, Hong JM, Choi JW, Yoo J, Hong JH, et al. Solitaire thrombectomy for acute stroke due to intracranial atherosclerosis-related occlusion: ROSE ASSIST study. Front Neurol. 2018; 9:1064.
Article7. Yoo J, Lee SJ, Hong JH, Kim YW, Hong JM, Kim CH, et al. Immediate effects of first-line thrombectomy devices for intracranial atherosclerosis-related occlusion: stent retriever versus contact aspiration. BMC Neurol. 2020; 20:283.
Article8. Kim YW, Sohn SI, Yoo J, Hong JH, Kim CH, Kang DH, et al. Local tirofiban infusion for remnant stenosis in large vessel occlusion: tirofiban ASSIST study. BMC Neurol. 2020; 20:284.
Article9. Lee SJ, Park SY, Hong JM, Choi JW, Kang DH, Kim YW, et al. Etiological approach to understanding recanalization failure in intracranial large vessel occlusion and thrombectomy: close to embolism but distant from atherosclerosis. Front Neurol. 2021; 11:598216.
Article10. Min JH, Lee SJ, Hong JM, Choi JW, Kang DH, Kim YW, et al. Clinical impact of intracerebral hemorrhage after hyperacute extracranial stenting in patients with ischemic stroke. Neurointervention. 2019; 14:107–115.
Article11. Yoo J, Choi JW, Lee SJ, Hong JM, Hong JH, Kim CH, et al. Ischemic diffusion lesion reversal after endovascular treatment. Stroke. 2019; 50:1504–1509.
Article12. Lee SJ, Hwang YH, Hong JM, Choi JW, Yoon BS, Kang DH, et al. Impact of varying levels of hyperglycemia on clinicoradiographic outcomes after endovascular reperfusion treatment. Sci Rep. 2018; 8:9832.
Article13. Yoo J, Hong JH, Lee SJ, Kim YW, Hong JM, Kim CH, et al. Acute kidney injury after endovascular treatment in patients with acute ischemic stroke. J Clin Med. 2020; 9:1471.
Article14. Choi MH, Gil YE, Lee SJ, Lee JS, Hong JH, Sohn SI, et al. The clinical usefulness of targeted temperature management in acute ischemic stroke with malignant trait after endovascular thrombectomy. [published online ahead of print Aug 18, 2020]. Neurocrit Care. 2020.
Article15. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, Interventional Management of Stroke (IMS) III Investigators, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 368:893–903.
Article16. Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, MR RESCUE Investigators, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013; 368:914–923.
Article17. Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, SYNTHESIS Expansion Investigators, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013; 368:904–913.
Article18. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, MR CLEAN Investigators, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.19. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, ESCAPE Trial Investigators, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.20. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, SWIFT PRIME Investigators, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.
Article21. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, EXTEND-IA Investigators, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.
Article22. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, REVASCAT Trial Investigators, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article23. Goyal M, Yu AY, Menon BK, Dippel DW, Hacke W, Davis SM, et al. Endovascular therapy in acute ischemic stroke: challenges and transition from trials to bedside. Stroke. 2016; 47:548–553.24. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, American Heart Association Stroke Council, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035.
Article25. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the Korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2016; 18:102–113.
Article26. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, RE-LY Steering Committee and Investigators, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Article27. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, ROCKET AF Investigators, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Article28. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, ARISTOTLE Committees and Investigators, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.29. Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, ENGAGE AF-TIMI 48 Investigators, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104.
Article30. Park SJ, Shim WH, Ho DS, Raizner AE, Park SW, Hong MK, et al. A paclitaxel-eluting stent for the prevention of coronary restenosis. N Engl J Med. 2003; 348:1537–1545.
Article31. Seung KB, Park DW, Kim YH, Lee SW, Lee CW, Hong MK, et al. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N Engl J Med. 2008; 358:1781–1792.
Article32. Park SJ, Kim YH, Park DW, Yun SC, Ahn JM, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011; 364:1718–1727.
Article33. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, DAWN Trial Investigators, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.34. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, DEFUSE 3 Investigators, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.
Article35. Liu X, Dai Q, Ye R, Zi W, Liu Y, Wang H, BEST Trial Investigators, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. 2020; 19:115–122.36. Schonewille W; BASICS study group. The Basilar Artery International Collaboration Study (BASICS): a randomized controlled trial of endovascular therapy in basilar artery occlusion. Paper presented at: the Joint European Stroke Organisation and World Stroke Organization Conference (ESO-WSO 2020). 2020 Nov 7-9; Vienna, Austria. Geneva: World Stroke Organization;2020. p. 5.37. Kim BM, Baek JH, Heo JH, Nam HS, Kim YD, Yoo J, et al. Collateral status affects the onset-to-reperfusion time window for good outcome. J Neurol Neurosurg Psychiatry. 2018; 89:903–909.
Article38. Kim YD, Heo JH, Yoo J, Park H, Kim BM, Bang OY, et al. Improving the clinical outcome in stroke patients receiving thrombolytic or endovascular treatment in Korea: from the SECRET study. J Clin Med. 2020; 9:717.
Article39. Kang DH, Jung C, Yoon W, Kim SK, Baek BH, Kim JT, et al. Endovascular thrombectomy for acute basilar artery occlusion: a multicenter retrospective observational study. J Am Heart Assoc. 2018; 7:e009419.
Article40. Lee JS, Hong JM, Kim JS. Diagnostic and Therapeutic Strategies for Acute Intracranial Atherosclerosis-related Occlusions. J Stroke. 2017; 19:143–151.
Article41. Koh S, Park JH, Park B, Choi MH, Lee SE, Lee JS, et al. Prediction of infarct growth and neurological deterioration in patients with vertebrobasilar artery occlusions. J Clin Med. 2020; 9:3759.
Article42. Kim YW, Hong JM, Park DG, Choi JW, Kang DH, Kim YS, et al. Effect of intracranial atherosclerotic disease on endovascular treatment for patients with acute vertebrobasilar occlusion. AJNR Am J Neuroradiol. 2016; 37:2072–2078.
Article43. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article44. Ko SB, Park HK, Kim BM, Heo JH, Rha JH, Kwon SU, et al. 2019 Update of the Korean clinical practice guidelines of stroke for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2019; 21:231–240.
Article45. Kim BJ, Kim JS. Ischemic stroke subtype classification: an Asian viewpoint. J Stroke. 2014; 16:8–17.
Article46. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan stroke study. Stroke. 1995; 26:14–20.47. Ratanakorn D, Keandoungchun J, Tegeler CH. Coexistent extra- and intracranial stenosis, cervical atherosclerosis, and abnormal ankle brachial index in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2012; 21:782–789.
Article48. Kim JS, Kim YJ, Ahn SH, Kim BJ. Location of cerebral atherosclerosis: why is there a difference between East and West? Int J Stroke. 2018; 13:35–46.
Article49. Baek JH, Kim BM, Heo JH, Kim DJ, Nam HS, Kim YD. Outcomes of endovascular treatment for acute intracranial atherosclerosis-related large vessel occlusion. Stroke. 2018; 49:2699–2705.
Article50. Suh HI, Hong JM, Lee KS, Han M, Choi JW, Kim JS, et al. Imaging predictors for atherosclerosis-related intracranial large artery occlusions in acute anterior circulation stroke. J Stroke. 2016; 18:352–354.
Article51. Lee YY, Yoon W, Kim SK, Baek BH, Kim GS, Kim JT, et al. Acute basilar artery occlusion: differences in characteristics and outcomes after endovascular therapy between patients with and without underlying severe atherosclerotic stenosis. AJNR Am J Neuroradiol. 2017; 38:1600–1604.
Article52. Baek JH, Kim BM, Heo JH, Kim DJ, Nam HS, Kim YD. Endovascular and clinical outcomes of vertebrobasilar intracranial atherosclerosis-related large vessel occlusion. Front Neurol. 2019; 10:215.
Article53. Li H, Zhang Y, Zhang L, Li Z, Xing P, Zhang Y, et al. Endovascular treatment of acute ischemic stroke due to intracranial atherosclerotic large vessel occlusion : a systematic review. Clin Neuroradiol. 2020; 30:777–787.54. Tsang ACO, Orru E, Klostranec JM, Yang IH, Lau KK, Tsang FCP, et al. Thrombectomy outcomes of intracranial atherosclerosis-related occlusions. Stroke. 2019; 50:1460–1466.
Article55. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, SWIFT Trialists, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249.
Article56. Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, TREVO 2 Trialists, et al. Trevo versus Merci Retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012; 380:1231–1240.
Article57. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system: forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287.
Article58. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014; 6:260–264.
Article59. Nguyen TN, Malisch T, Castonguay AC, Gupta R, Sun CH, Martin CO, et al. Balloon guide catheter improves revascularization and clinical outcomes with the Solitaire device: analysis of the North American Solitaire Acute Stroke registry. Stroke. 2014; 45:141–145.
Article60. Kang DH, Kim BM, Heo JH, Nam HS, Kim YD, Hwang YH, et al. Effect of balloon guide catheter utilization on contact aspiration thrombectomy. [published online ahead of print Nov 1, 2018]. J Neurosurg. 2018.
Article61. Kim YW, Kang DH, Hwang YH, Park J, Kim YS. Efficacy of proximal aspiration thrombectomy for using balloon-tipped guide catheter in acute intracranial internal carotid artery occlusion. J Korean Neurosurg Soc. 2016; 59:379–384.
Article62. Baek JH, Kim BM, Kang DH, Heo JH, Nam HS, Kim YD, et al. Balloon guide catheter is beneficial in endovascular treatment regardless of mechanical recanalization modality. Stroke. 2019; 50:1490–1496.
Article63. Klinger-Gratz PP, Schroth G, Gralla J, Jung S, Weisstanner C, Verma RK, et al. Protected stent retriever thrombectomy prevents iatrogenic emboli in new vascular territories. Neuroradiology. 2015; 57:1045–1054.
Article64. Alverne FJAM, Lima FO, Rocha FA, Bandeira DA, Lucena AF, Silva HC, et al. Unfavorable vascular anatomy during endovascular treatment of stroke: challenges and bailout strategies. J Stroke. 2020; 22:185–202.
Article65. Yoo AJ, Andersson T. Thrombectomy in acute ischemic stroke: challenges to procedural success. J Stroke. 2017; 19:121–130.
Article66. Klisch J, Sychra V, Strasilla C, Taschner CA, Reinhard M, Urbach H, et al. Double solitaire mechanical thrombectomy in acute stroke: effective rescue strategy for refractory artery occlusions? AJNR Am J Neuroradiol. 2015; 36:552–556.
Article67. Aydin K, Barburoglu M, Oztop Cakmak O, Yesilot N, Vanli ENY, Akpek S. Crossing Y-Solitaire thrombectomy as a rescue treatment for refractory acute occlusions of the middle cerebral artery. J Neurointerv Surg. 2019; 11:246–250.
Article68. Lee JS, Hong JM, Lee KS, Suh HI, Choi JW, Kim SY. Primary stent retrieval for acute intracranial large artery occlusion due to atherosclerotic disease. J Stroke. 2016; 18:96–101.
Article69. Kang DH, Yoon W, Baek BH, Kim SK, Lee YY, Kim JT, et al. Front-line thrombectomy for acute large-vessel occlusion with underlying severe intracranial stenosis: stent retriever versus contact aspiration. J Neurosurg. 2019; 132:1202–1208.
Article70. Kang DH, Hwang YH. Frontline contact aspiration treatment for emergent large vessel occlusion: a review focused on practical techniques. J Stroke. 2019; 21:10–22.
Article71. Heo JH, Lee KY, Kim SH, Kim DI. Immediate reocclusion following a successful thrombolysis in acute stroke: a pilot study. Neurology. 2003; 60:1684–1687.
Article72. Kwon OK, Lee KJ, Han MH, Oh CW, Han DH, Koh YC. Intraarterially administered abciximab as an adjuvant thrombolytic therapy: report of three cases. AJNR Am J Neuroradiol. 2002; 23:447–451.73. Baik SK, Oh SJ, Park KP, Lee JH. Intra-arterial tirofiban infusion for partial recanalization with stagnant flow in hyperacute cerebral ischemic stroke. Interv Neuroradiol. 2011; 17:442–451.
Article74. Kang DH, Kim YW, Hwang YH, Park SP, Kim YS, Baik SK. Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis. 2014; 37:350–355.
Article75. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015; 76:680–686.
Article76. Kim JG, Suh DC, Song Y, Choi JC, Lee DH. Direct stenting of intracranial atherosclerosis-related acute large vessel occlusion. [published online ahead of print Jul 30, 2020]. Clin Neuroradiol. 2020.
Article77. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 2016; 47:2360–2363.
Article78. Chang Y, Kim BM, Bang OY, Baek JH, Heo JH, Nam HS, et al. Rescue stenting for failed mechanical thrombectomy in acute ischemic stroke: a multicenter experience. Stroke. 2018; 49:958–964.79. Maingard J, Phan K, Lamanna A, Kok HK, Barras CD, Russell J, et al. Rescue intracranial stenting after failed mechanical thrombectomy for acute ischemic stroke: a systematic review and meta-analysis. World Neurosurg. 2019; 132:e235–e245.
Article80. Papanagiotou P, Roth C, Walter S, Behnke S, Grunwald IQ, Viera J, et al. Carotid artery stenting in acute stroke. J Am Coll Cardiol. 2011; 58:2363–2369.
Article81. Anadani M, Spiotta AM, Alawieh A, Turjman F, Piotin M, Haussen DC, TITAN (Thrombectomy In TANdem Lesions) Investigators, et al. Emergent carotid stenting plus thrombectomy after thrombolysis in tandem strokes: analysis of the TITAN registry. Stroke. 2019; 50:2250–2252.
Article82. Rodrigues M, Cunha A, Figueiredo S, Carvalho A, Veloso M, Barros P, et al. Emergent carotid artery stenting in atherosclerotic disease of the internal carotid artery with tandem intracranial occlusion. J Neurol Sci. 2018; 387:196–198.
Article83. Saver JL. Time is brain--quantified. Stroke. 2006; 37:263–266.
Article84. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, HERMES Collaborators, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316:1279–1288.
Article85. Bang OY, Saver JL, Buck BH, Alger JR, Starkman S, Ovbiagele B, UCLA Collateral Investigators, et al. Impact of collateral flow on tissue fate in acute ischaemic stroke. J Neurol Neurosurg Psychiatry. 2008; 79:625–629.
Article86. Liebeskind DS. Collateral lessons from recent acute ischemic stroke trials. Neurol Res. 2014; 36:397–402.
Article87. Hwang YH, Kang DH, Kim YW, Kim YS, Park SP, Liebeskind DS. Impact of time-to-reperfusion on outcome in patients with poor collaterals. AJNR Am J Neuroradiol. 2015; 36:495–500.
Article88. Lee SU, Hong JM, Kim SY, Bang OY, Demchuk AM, Lee JS. Differentiating carotid terminus occlusions into two distinct populations based on willisian collateral status. J Stroke. 2016; 18:179–186.
Article89. Kim DH, Kim B, Jung C, Nam HS, Lee JS, Kim JW, et al. Consensus statements by Korean Society of Interventional Neuroradiology and Korean Stroke Society: hyperacute endovascular treatment workflow to reduce door-to-reperfusion time. Korean J Radiol. 2018; 19:838–848.
Article90. Lee D, Lee DH, Suh DC, Kim BJ, Kwon SU, Kwon HS, et al. Endovascular treatment in patients with cerebral artery occlusion of three different etiologies. J Stroke. 2020; 22:234–244.
Article91. Demchuk AM, Goyal M, Menon BK, Eesa M, Ryckborst KJ, Kamal N, ESCAPE Trial Investigators, et al. Endovascular treatment for Small Core and Anterior circulation Proximal occlusion with Emphasis on minimizing CT to recanalization times (ESCAPE) trial: methodology. Int J Stroke. 2015; 10:429–438.
Article92. Choi MH, Lim TS, Yoon BS, Son KS, Hong JM, Lee JS. Low testosterone level as a predictor of poststroke emotional disturbances: anger proneness and emotional incontinence. J Stroke Cerebrovasc Dis. 2018; 27:3549–3554.
Article93. Ribo M, Molina CA, Cobo E, Cerdà N, Tomasello A, Quesada H, REVASCAT Trial Investigators, et al. Association between time to reperfusion and outcome is primarily driven by the time from imaging to reperfusion. Stroke. 2016; 47:999–1004.
Article94. Tsai JP, Mlynash M, Christensen S, Kemp S, Kim S, Mishra NK, CRISP Investigators, et al. Time from imaging to endovascular reperfusion predicts outcome in acute stroke. Stroke. 2018; 49:952–957.
Article95. Loubinoux I, Volk A, Borredon J, Guirimand S, Tiffon B, Seylaz J, et al. Spreading of vasogenic edema and cytotoxic edema assessed by quantitative diffusion and T2 magnetic resonance imaging. Stroke. 1997; 28:419–426. discussion 426-427.
Article96. Hossmann KA, Fischer M, Bockhorst K, Hoehn-Berlage M. NMR imaging of the apparent diffusion coefficient (ADC) for the evaluation of metabolic suppression and recovery after prolonged cerebral ischemia. J Cereb Blood Flow Metab. 1994; 14:723–731.
Article97. Han M, Choi JW, Rim NJ, Kim SY, Suh HI, Lee KS, et al. Cerebral infarct volume measurements to improve patient selection for endovascular treatment. Medicine (Baltimore). 2016; 95:e4702.
Article98. Sakamoto Y, Kimura K, Shibazaki K, Inoue T, Uemura J, Aoki J, et al. Early ischaemic diffusion lesion reduction in patients treated with intravenous tissue plasminogen activator: infrequent, but significantly associated with recanalization. Int J Stroke. 2013; 8:321–326.
Article99. Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke. 2018; 49:660–666.100. Chamorro Á, Blasco J, López A, Amaro S, Román LS, Llull L, et al. Complete reperfusion is required for maximal benefits of mechanical thrombectomy in stroke patients. Sci Rep. 2017; 7:11636.
Article101. Kleine JF, Wunderlich S, Zimmer C, Kaesmacher J. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J Neurointerv Surg. 2017; 9:117–121.
Article102. Tung EL, McTaggart RA, Baird GL, Yaghi S, Hemendinger M, Dibiasio EL, et al. Rethinking thrombolysis in cerebral infarction 2b: which thrombolysis in cerebral infarction scales best define near complete recanalization in the modern thrombectomy era? Stroke. 2017; 48:2488–2493.
Article103. Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, ASTER Trial Investigators, et al. Modified Thrombolysis in Cerebral Infarction 2C/Thrombolysis in Cerebral Infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights from the ASTER trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization). Stroke. 2018; 49:1189–1196.104. Kaesmacher J, Dobrocky T, Heldner MR, Bellwald S, Mosimann PJ, Mordasini P, et al. Systematic review and meta-analysis on outcome differences among patients with TICI2b versus TICI3 reperfusions: success revisited. J Neurol Neurosurg Psychiatry. 2018; 89:910–917.
Article105. Parsons MW, Barber PA, Desmond PM, Baird TA, Darby DG, Byrnes G, et al. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002; 52:20–28.
Article106. Dávalos A, Toni D, Iweins F, Lesaffre E, Bastianello S, Castillo J. Neurological deterioration in acute ischemic stroke: potential predictors and associated factors in the European cooperative acute stroke study (ECASS) I. Stroke. 1999; 30:2631–2636.107. Lansberg MG, Albers GW, Wijman CA. Symptomatic intracerebral hemorrhage following thrombolytic therapy for acute ischemic stroke: a review of the risk factors. Cerebrovasc Dis. 2007; 24:1–10.
Article108. Lee SJ, Hong JM, Lee SE, Kang DR, Ovbiagele B, Demchuk AM, et al. Association of fibrinogen level with early neurological deterioration among acute ischemic stroke patients with diabetes. BMC Neurol. 2017; 17:101.
Article109. Summary information on a referral opinion following an arbitration pursuant to Article 29 of Directive 2001/83/ec, for Actilyse [Internet]. London: European Medicines Agency;2002. Nov. 21. [cited 2020 Sep 7]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Actilyse_29/WC500010327.pdf.110. Hacke W, Albers G, Al-Rawi Y, Bogousslavsky J, Davalos A, Eliasziw M, DIAS Study Group, et al. The Desmoteplase in Acute Ischemic Stroke Trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke. 2005; 36:66–73.111. Ehrlich ME, Liang L, Xu H, Kosinski AS, Hernandez AF, Schwamm LH, et al. Intravenous tissue-type plasminogen activator in acute ischemic stroke patients with history of stroke plus diabetes mellitus. Stroke. 2019; 50:1497–1503.
Article112. Demchuk AM, Morgenstern LB, Krieger DW, Linda Chi T, Hu W, Wein TH, et al. Serum glucose level and diabetes predict tissue plasminogen activator-related intracerebral hemorrhage in acute ischemic stroke. Stroke. 1999; 30:34–39.
Article113. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999; 282:2003–2011.114. Kase CS, Furlan AJ, Wechsler LR, Higashida RT, Rowley HA, Hart RG, et al. Cerebral hemorrhage after intra-arterial thrombolysis for ischemic stroke: the PROACT II trial. Neurology. 2001; 57:1603–1610.
Article115. Wei J, Huang NC, Quast MJ. Hydroxyl radical formation in hyperglycemic rats during middle cerebral artery occlusion/reperfusion. Free Radic Biol Med. 1997; 23:986–995.
Article116. Quast MJ, Wei J, Huang NC, Brunder DG, Sell SL, Gonzalez JM, et al. Perfusion deficit parallels exacerbation of cerebral ischemia/reperfusion injury in hyperglycemic rats. J Cereb Blood Flow Metab. 1997; 17:553–559.
Article117. Osei E, den Hertog HM, Berkhemer OA, Fransen PS, Roos YB, Beumer D, MR CLEAN pretrial investigators, et al. Increased admission and fasting glucose are associated with unfavorable short-term outcome after intra-arterial treatment of ischemic stroke in the MR CLEAN pretrial cohort. J Neurol Sci. 2016; 371:1–5.
Article118. Kruyt ND, Biessels GJ, Devries JH, Roos YB. Hyperglycemia in acute ischemic stroke: pathophysiology and clinical management. Nat Rev Neurol. 2010; 6:145–155.
Article119. Johnston KC, Bruno A, Pauls Q, Hall CE, Barrett KM, Barsan W, Neurological Emergencies Treatment Trials Network and the SHINE Trial Investigators, et al. Intensive vs standard treatment of hyperglycemia and functional outcome in patients with acute ischemic stroke: the SHINE randomized clinical trial. JAMA. 2019; 322:326–335.120. Josephson SA, Dillon WP, Smith WS. Incidence of contrast nephropathy from cerebral CT angiography and CT perfusion imaging. Neurology. 2005; 64:1805–1806.
Article121. Krol AL, Dzialowski I, Roy J, Puetz V, Subramaniam S, Coutts SB, et al. Incidence of radiocontrast nephropathy in patients undergoing acute stroke computed tomography angiography. Stroke. 2007; 38:2364–2366.
Article122. Hopyan JJ, Gladstone DJ, Mallia G, Schiff J, Fox AJ, Symons SP, et al. Renal safety of CT angiography and perfusion imaging in the emergency evaluation of acute stroke. AJNR Am J Neuroradiol. 2008; 29:1826–1830.
Article123. Prasad V, Gandhi D, Stokum C, Miller T, Jindal G. Incidence of contrast material-induced nephropathy after neuroendovascular procedures. Radiology. 2014; 273:853–858.
Article124. Covic A, Schiller A, Mardare NG, Petrica L, Petrica M, Mihaescu A, et al. The impact of acute kidney injury on short-term survival in an Eastern European population with stroke. Nephrol Dial Transplant. 2008; 23:2228–2234.
Article125. Tsagalis G, Akrivos T, Alevizaki M, Manios E, Theodorakis M, Laggouranis A, et al. Long-term prognosis of acute kidney injury after first acute stroke. Clin J Am Soc Nephrol. 2009; 4:616–622.
Article126. Tsagalis G, Akrivos T, Alevizaki M, Manios E, Stamatellopoulos K, Laggouranis A, et al. Renal dysfunction in acute stroke: an independent predictor of long-term all combined vascular events and overall mortality. Nephrol Dial Transplant. 2009; 24:194–200.
Article127. Rowe AS, Hawkins B, Hamilton LA, Ferrell A, Henry J, Wiseman BF, et al. Contrast-induced nephropathy in ischemic stroke patients undergoing computed tomography angiography: CINISter study. J Stroke Cerebrovasc Dis. 2019; 28:649–654.
Article128. McCullough PA, Wolyn R, Rocher LL, Levin RN, O’Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997; 103:368–375.129. Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002; 105:2259–2264.
Article130. Gruberg L, Mintz GS, Mehran R, Gangas G, Lansky AJ, Kent KM, et al. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol. 2000; 36:1542–1548.
Article131. Marenzi G, Assanelli E, Campodonico J, Lauri G, Marana I, De Metrio M, et al. Contrast volume during primary percutaneous coronary intervention and subsequent contrast-induced nephropathy and mortality. Ann Intern Med. 2009; 150:170–177.
Article132. Loh Y, McArthur DL, Vespa P, Shi ZS, Liebeskind DS, Jahan R, et al. The risk of acute radiocontrast-mediated kidney injury following endovascular therapy for acute ischemic stroke is low. AJNR Am J Neuroradiol. 2010; 31:1584–1587.
Article133. Sharma J, Nanda A, Jung RS, Mehta S, Pooria J, Hsu DP. Risk of contrast-induced nephropathy in patients undergoing endovascular treatment of acute ischemic stroke. J Neurointerv Surg. 2013; 5:543–545.
Article134. Diprose WK, Sutherland LJ, Wang MTM, Barber PA. Contrast-associated acute kidney injury in endovascular thrombectomy patients with and without baseline renal impairment. Stroke. 2019; 50:3527–3531.
Article135. Jia ZY, Wang SX, Zhao LB, Cao YZ, Shi HB, Liu S. Risk of acute kidney injury with consecutive, multidose use of iodinated contrast in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 2019; 40:652–654.
Article136. Chen YL, Fu NK, Xu J, Yang SC, Li S, Liu YY. A simple preprocedural score for risk of contrast-induced acute kidney injury after percutaneous coronary intervention. Catheter Cardiovasc Interv. 2014; 83:E8–E16.
Article137. Parfrey P. The clinical epidemiology of contrast-induced nephropathy. Cardiovasc Intervent Radiol. 2005; 28 Suppl 2:S3–S11.
Article138. Stacul F. Reducing the risks for contrast-induced nephropathy. Cardiovasc Intervent Radiol. 2005; 28 Suppl 2:S12–S18.
Article139. Solomon R, Dumouchel W. Contrast media and nephropathy: findings from systematic analysis and Food and Drug Administration reports of adverse effects. Invest Radiol. 2006; 41:651–660.140. Dong M, Jiao Z, Liu T, Guo F, Li G. Effect of administration route on the renal safety of contrast agents: a meta-analysis of randomized controlled trials. J Nephrol. 2012; 25:290–301.
Article141. Han XF, Zhang XX, Liu KM, Tan H, Zhang Q. Contrast-induced nephropathy in patients with diabetes mellitus between iso- and low-osmolar contrast media: a meta-analysis of fulltext prospective, randomized controlled trials. PLoS One. 2018; 13:e0194330.
Article142. Toprak O. Risk markers for contrast-induced nephropathy. Am J Med Sci. 2007; 334:283–290.
Article143. Calvin AD, Misra S, Pflueger A. Contrast-induced acute kidney injury and diabetic nephropathy. Nat Rev Nephrol. 2010; 6:679–688.
Article144. Heyman SN, Rosenberger C, Rosen S, Khamaisi M. Why is diabetes mellitus a risk factor for contrast-induced nephropathy? Biomed Res Int. 2013; 2013:123589.
Article145. Wichmann JL, Katzberg RW, Litwin SE, Zwerner PL, De Cecco CN, Vogl TJ, et al. Contrast-induced nephropathy. Circulation. 2015; 132:1931–1936.
Article146. Liu LY, Liu Y, Wu MY, Sun YY, Ma FZ. Efficacy of atorvastatin on the prevention of contrast-induced acute kidney injury: a meta-analysis. Drug Des Devel Ther. 2018; 12:437–444.
Article147. Dirnagl U, Iadecola C, Moskowitz MA. Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci. 1999; 22:391–397.
Article148. Shuaib A, Lees KR, Lyden P, Grotta J, Davalos A, Davis SM, SAINT II Trial Investigators, et al. NXY-059 for the treatment of acute ischemic stroke. N Engl J Med. 2007; 357:562–571.
Article149. Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, ESCAPE-NA1 Investigators, et al. Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet. 2020; 395:878–887.150. Hong JM, Choi MH, Sohn SI, Hwang YH, Ahn SH, Lee YB, on the behalf of the SONIC investigators, et al. Safety and Optimal Neuroprotection of Neu2000 in acute Ischemic stroke with reCanalization: study protocol for a randomized, double-blinded, placebo-controlled, phase-II trial. Trials. 2018; 19:375.
Article151. Lyden P, Hemmen T, Grotta J, Rapp K, Ernstrom K, Rzesiewicz T, Collaborators, et al. Results of the ICTuS 2 trial (intravascular cooling in the treatment of stroke 2). Stroke. 2016; 47:2888–2895.152. Neugebauer H, Schneider H, Bösel J, Hobohm C, Poli S, Kollmar R, et al. Outcomes of hypothermia in addition to decompressive hemicraniectomy in treatment of malignant middle cerebral artery stroke: a randomized clinical trial. JAMA Neurol. 2019; 76:571–579.153. Hong JM, Lee JS, Song HJ, Jeong HS, Choi HA, Lee K. Therapeutic hypothermia after recanalization in patients with acute ischemic stroke. Stroke. 2014; 45:134–140.
Article154. Marshall JW, Duffin KJ, Green AR, Ridley RM. NXY-059, a free radical--trapping agent, substantially lessens the functional disability resulting from cerebral ischemia in a primate species. Stroke. 2001; 32:190–198.
Article155. Lees KR, Zivin JA, Ashwood T, Davalos A, Davis SM, Diener HC, Stroke-Acute Ischemic NXY Treatment (SAINT I) Trial Investigators, et al. NXY-059 for acute ischemic stroke. N Engl J Med. 2006; 354:588–600.
Article156. Stroke Therapy Academic Industry Roundtable (STAIR). Recommendations for standards regarding preclinical neuroprotective and restorative drug development. Stroke. 1999; 30:2752–2758.157. Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, STAIR Group, et al. Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke. 2009; 40:2244–2250.
Article158. Lee JS, Hong JM, Kim EJ, Shin DH, Joo IS, Lim YC, et al. Comparison of the incidence of parenchymal hematoma and poor outcome in patients with carotid terminus occlusion treated with intra-arterial urokinase alone or with combined IV rtPA and intra-arterial urokinase. AJNR Am J Neuroradiol. 2012; 33:175–179.
Article159. Lee JS, Hong JM, Lee SJ, Joo IS, Lim YC, Kim SY. The combined use of mechanical thrombectomy devices is feasible for treating acute carotid terminus occlusion. Acta Neurochir (Wien). 2013; 155:635–641.
Article160. Eom YI, Hwang YH, Hong JM, Choi JW, Lim YC, Kang DH, et al. Forced arterial suction thrombectomy with the penumbra reperfusion catheter in acute basilar artery occlusion: a retrospective comparison study in 2 Korean university hospitals. AJNR Am J Neuroradiol. 2014; 35:2354–2359.
Article161. Aarts M, Liu Y, Liu L, Besshoh S, Arundine M, Gurd JW, et al. Treatment of ischemic brain damage by perturbing NMDA receptor- PSD-95 protein interactions. Science. 2002; 298:846–850.
Article162. Sun HS, Doucette TA, Liu Y, Fang Y, Teves L, Aarts M, et al. Effectiveness of PSD95 inhibitors in permanent and transient focal ischemia in the rat. Stroke. 2008; 39:2544–2553.
Article163. Hill MD, Martin RH, Mikulis D, Wong JH, Silver FL, Terbrugge KG, ENACT trial investigators, et al. Safety and efficacy of NA-1 in patients with iatrogenic stroke after endovascular aneurysm repair (ENACT): a phase 2, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2012; 11:942–950.164. Slomski A. Alteplase inhibits nerinetide, a novel stroke drug. JAMA. 2020; 323:1543.
Article165. Baron JC. Nerinetide: a potential neuroprotectant as adjunct to thrombectomy for acute stroke. Can J Neurol Sci. 2021; 48:138.
Article166. Gwag BJ, Lee YA, Ko SY, Lee MJ, Im DS, Yun BS, et al. Marked prevention of ischemic brain injury by Neu2000, an NMDA antagonist and antioxidant derived from aspirin and sulfasalazine. J Cereb Blood Flow Metab. 2007; 27:1142–1151.
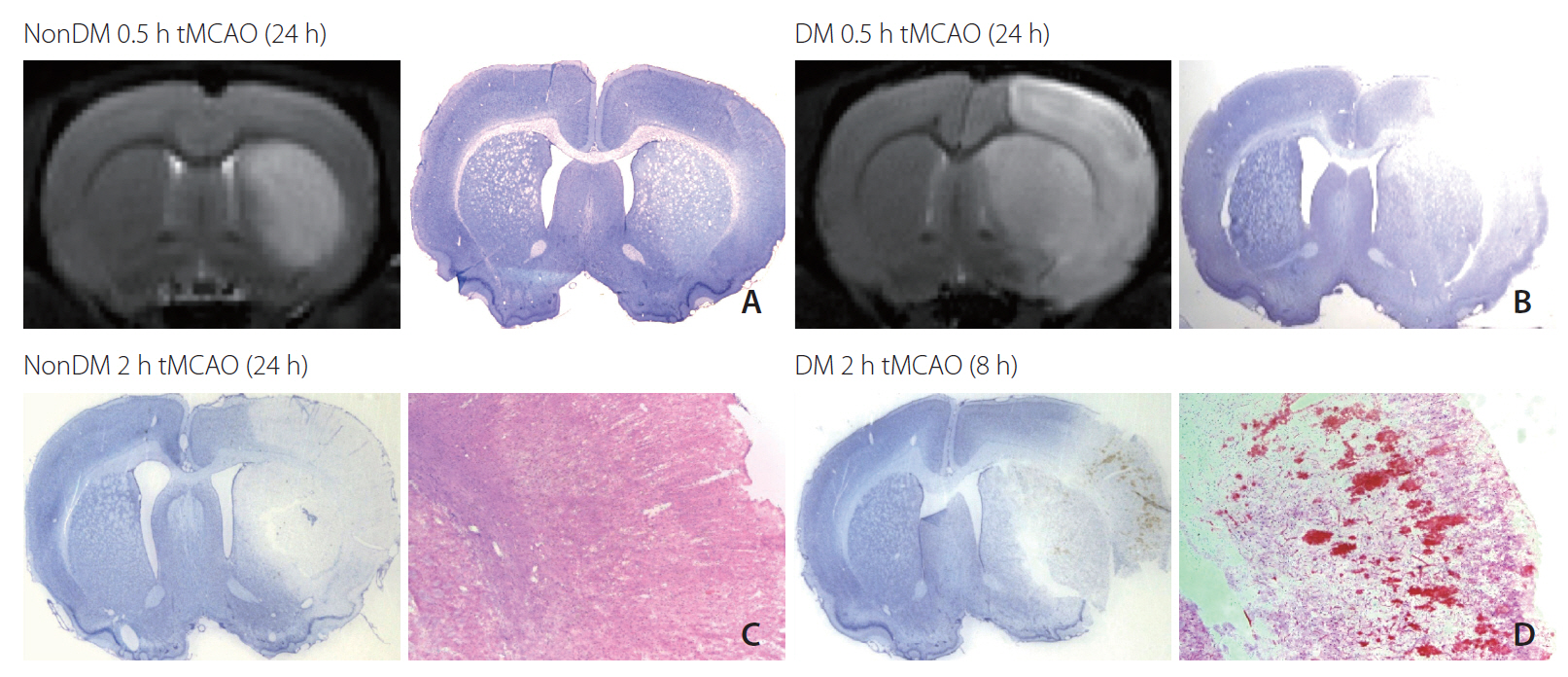
Article167. Im DS, Jeon JW, Lee JS, Won SJ, Cho SI, Lee YB, et al. Role of the NMDA receptor and iron on free radical production and brain damage following transient middle cerebral artery occlusion. Brain Res. 2012; 1455:114–123.
Article168. Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009; 37(7 Suppl):S186–S202.
Article169. Erecinska M, Thoresen M, Silver IA. Effects of hypothermia on energy metabolism in Mammalian central nervous system. J Cereb Blood Flow Metab. 2003; 23:513–530.
Article170. Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346:557–563.
Article171. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346:549–556.172. Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015; 132(18 Suppl 2):S465–S482.173. Kuczynski AM, Demchuk AM, Almekhlafi MA. Therapeutic hypothermia: applications in adults with acute ischemic stroke. Brain Circ. 2019; 5:43–54.
Article174. Piironen K, Tiainen M, Mustanoja S, Kaukonen KM, Meretoja A, Tatlisumak T, et al. Mild hypothermia after intravenous thrombolysis in patients with acute stroke: a randomized controlled trial. Stroke. 2014; 45:486–491.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Considerations When Subtyping Ischemic Stroke in Asian Patients
- Endovascular Thrombectomy for Acute Ischemic Stroke : Current Concept in Management
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke