Korean J Transplant.
2021 Jun;35(2):130-136. 10.4285/kjt.20.0056.
Recipient hepatectomy under total hepatic vascular exclusion to prevent hepatocellular carcinoma spread in living donor liver transplantation
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2517297
- DOI: http://doi.org/10.4285/kjt.20.0056
Abstract
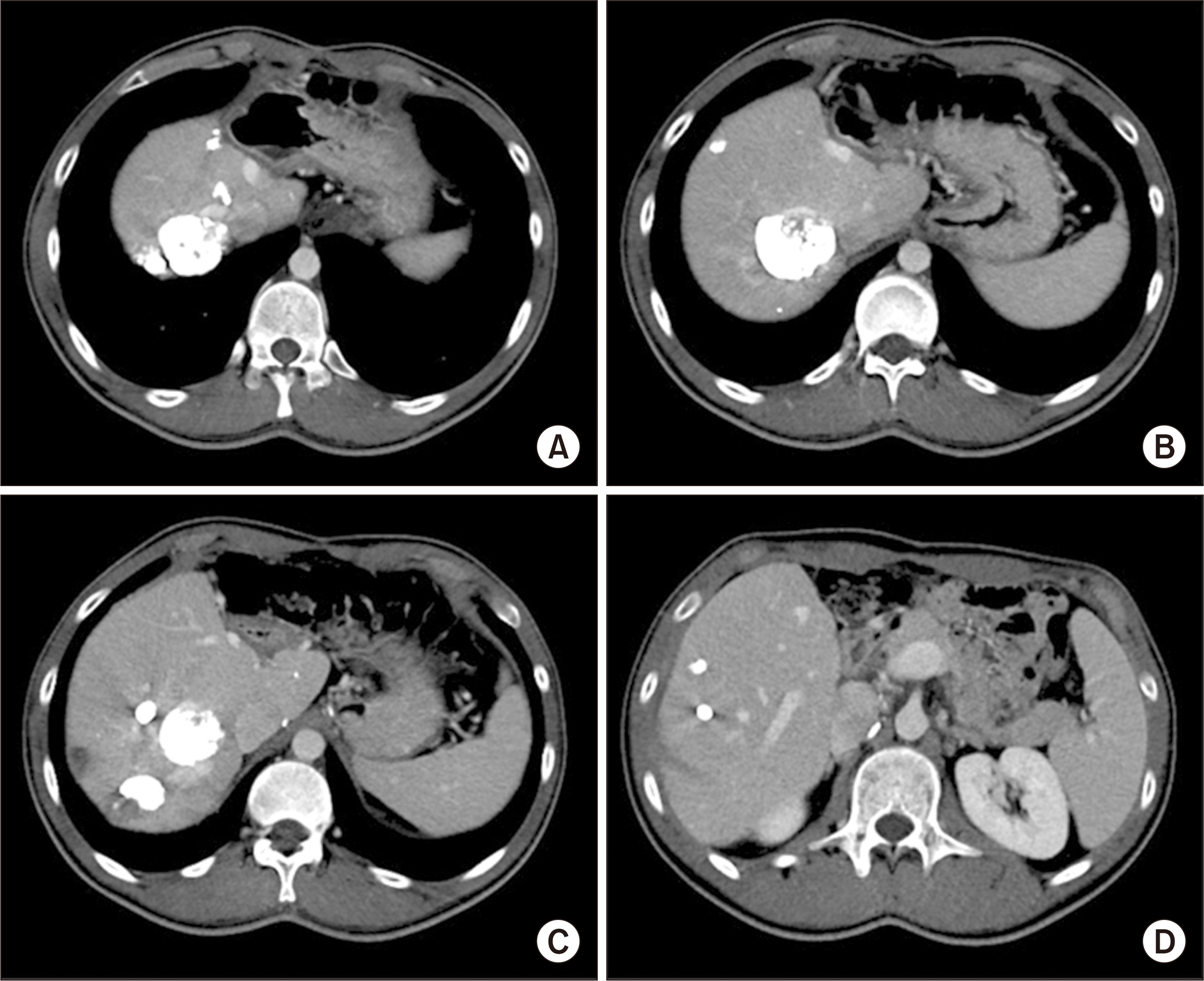
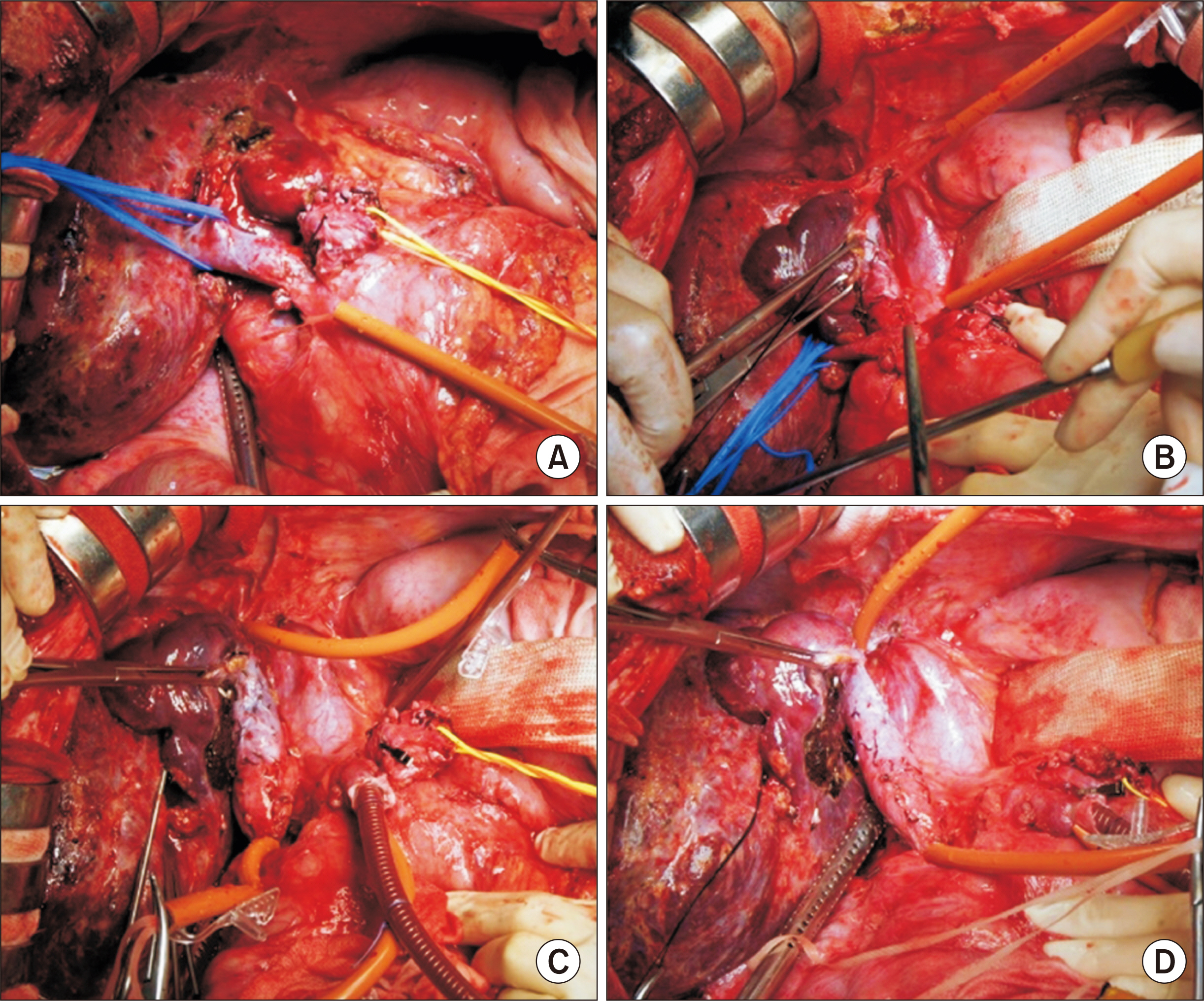
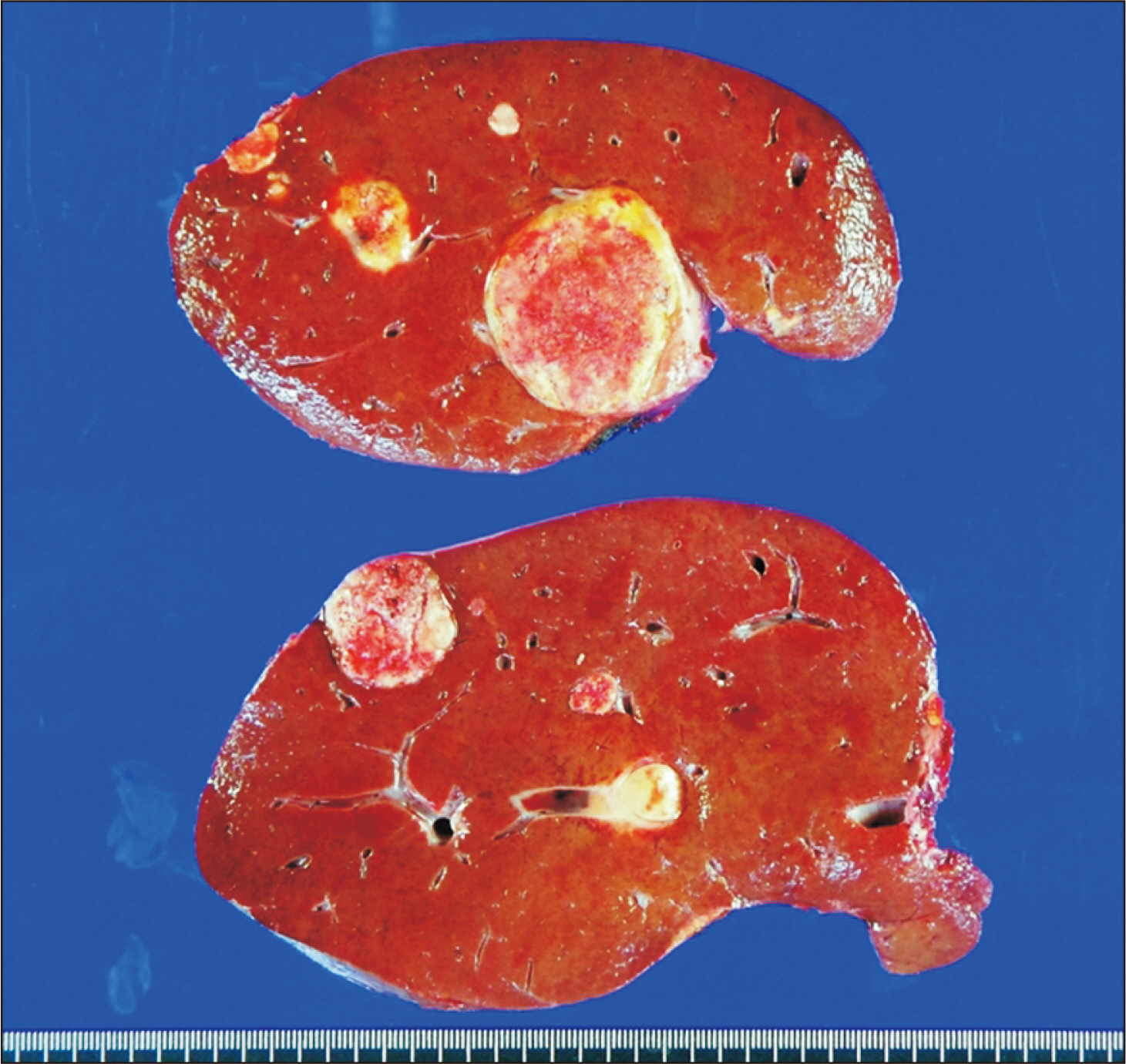
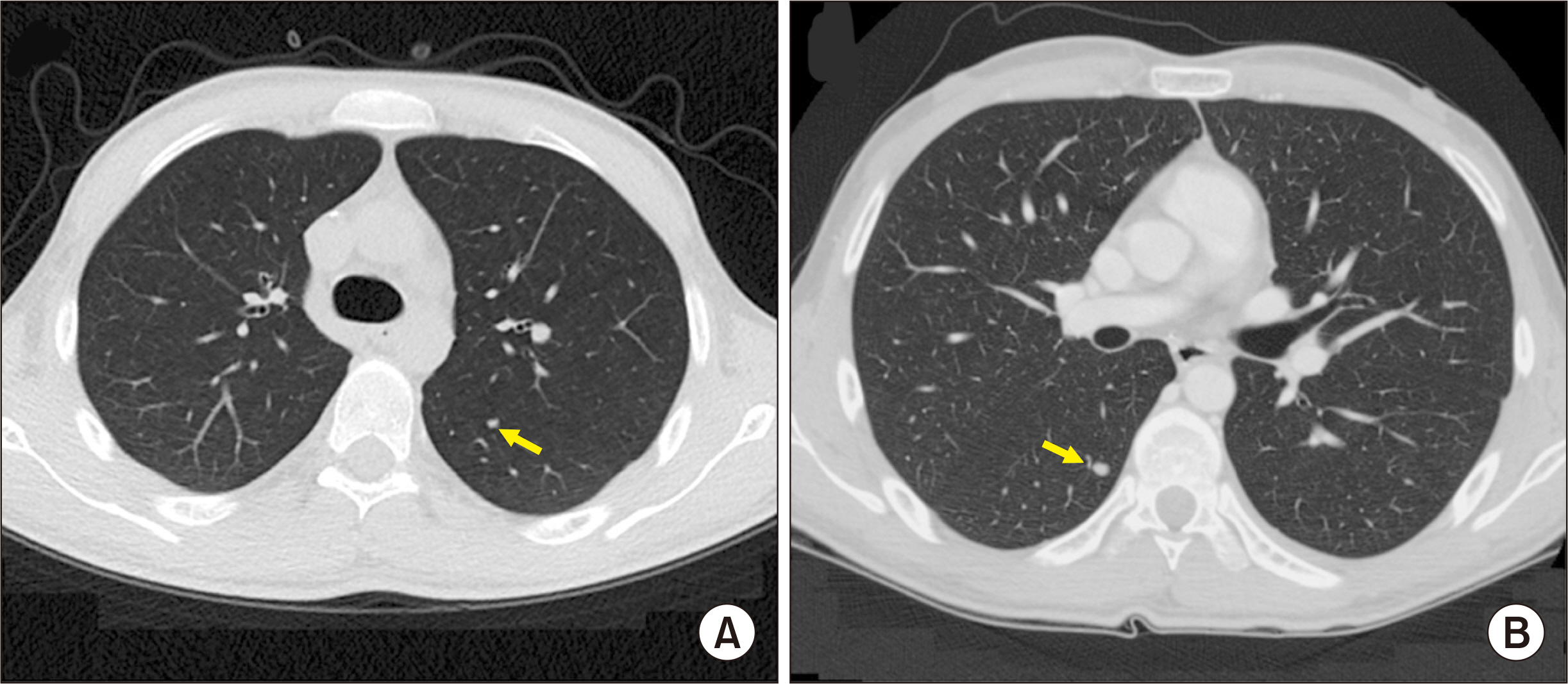
- We present a case of recipient hepatectomy under total hepatic vascular exclusion (THVE) and venovenous bypass for living donor liver transplantation (LDLT) in a patient with multiple hepatocellular carcinomas (HCCs) closely located to the retrohepatic inferior vena cava (IVC). A 19-year-old male patient diagnosed with multiple HCCs underwent left lateral sectionectomy 14 months before and received four sessions of transarterial chemoembolization due to post-hepatectomy tumor recurrence. These pretransplant sequences implicated high risk of posttransplant HCC recurrence. However, LDLT was performed with expectation of prolonged survival. During recipient operation, the portal vein was transected and active venovenous bypass was performed. Supra- and infra-hepatic portions of the retrohepatic IVC were then clamped. Under THVE and portal vein bypass, recipient hepatectomy was meticulously performed. A modified right liver graft recovered from his brother was implanted according to standard procedures of LDLT. The patient recovered uneventfully from LDLT operation. However, multiple pulmonary metastasis occurred. The patient has been doing well for 12 months after LDLT, with administration of chemotherapeutic agents. Although early pulmonary metastasis occurred in this patient, we suggest that recipient hepatectomy under THVE and venovenous bypass can be a feasible technical option to cope with risk of iatrogenic tumor cell spread during LDLT operation.
Figure
Reference
-
1. Mangus RS, Fridell JA, Vianna RM, Cooper AB, Jones DT, Tector AJ. 2008; Use of the piggyback hepatectomy technique in liver transplant recipients with hepatocellular carcinoma. Transplantation. 85:1496–9. DOI: 10.1097/TP.0b013e31816feec0. PMID: 18497692.
Article2. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. 2013; No-touch en bloc right lobe living-donor liver transplantation with inferior vena cava replacement for hepatocellular carcinoma close to retrohepatic inferior vena cava: case report. Transplant Proc. 45:3135–9. DOI: 10.1016/j.transproceed.2013.08.052. PMID: 24157050.
Article3. Matsuda H, Sadamori H, Shinoura S, Umeda Y, Yoshida R, Satoh D, et al. 2010; Aggressive combined resection of hepatic inferior vena cava, with replacement by a ringed expanded polytetrafluoroethylene graft, in living-donor liver transplantation for hepatocellular carcinoma beyond the Milan criteria. J Hepatobiliary Pancreat Sci. 17:719–24. DOI: 10.1007/s00534-010-0287-z. PMID: 20425126.
Article4. Smyrniotis VE, Kostopanagiotou GG, Gamaletsos EL, Vassiliou JG, Voros DC, Fotopoulos AC, et al. 2002; Total versus selective hepatic vascular exclusion in major liver resections. Am J Surg. 183:173–8. DOI: 10.1016/S0002-9610(01)00864-9.
Article5. Azoulay D, Lim C, Salloum C, Andreani P, Maggi U, Bartelmaos T, et al. 2015; Complex liver resection using standard total vascular exclusion, venovenous bypass, and in situ hypothermic portal perfusion: an audit of 77 consecutive cases. Ann Surg. 262:93–104. DOI: 10.1097/SLA.0000000000000787. PMID: 24950284.6. Choi JU, Hwang S, Chung IJ, Kang SH, Ahn CS, Moon DB, et al. 2020; Prolonged hepatic inflow occlusion to reduce bleeding during recipient hepatectomy in living donor liver transplantation. Korean J Transplant. 34:55–61.7. Choi JU, Hwang S, Ahn CS, Moon DB, Ha TY, Kim KH, et al. 2019; Prolonged occlusion of the hepatoduodenal ligament to reduce risk of bleeding and tumor spread during recipient hepatectomy for living donor liver transplantation. Ann Hepatobiliary Pancreat Surg. 23:61–4. DOI: 10.14701/ahbps.2019.23.1.61. PMID: 30863809. PMCID: PMC6405371.
Article8. Hwang S, Song GW, Ahn CS, Kim KH, Moon DB, Ha TY, et al. 2020; Nov. 11. Salvage living donor liver transplantation for hepatocellular carcinoma recurrence after hepatectomy: quantitative prediction using ADV score. J Hepatobiliary Pancreat Sci. [Epub]. https://doi.org/ 10.1002/jhbp.863. DOI: 10.1002/jhbp.863. PMID: 33175453.
Article9. Jabir MA, Hamza HM, Fakhry H, Amira G, Hatano E, Uemoto S. 2017; Anterior versus conventional approach for resection of large right lobe hepatocellular carcinoma. J Gastrointest Cancer. 48:25–30. DOI: 10.1007/s12029-016-9865-x. PMID: 27506210.
Article10. Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. 2007; Small-sized liver graft does not increase the risk of hepatocellular carcinoma recurrence after living donor liver transplantation. Transplant Proc. 39:1526–9. DOI: 10.1016/j.transproceed.2007.03.066. PMID: 17580180.
Article11. Liang W, Wu L, Ling X, Schroder PM, Ju W, Wang D, et al. 2012; Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: a meta-analysis. Liver Transpl. 18:1226–36. DOI: 10.1002/lt.23490. PMID: 22685095.
Article12. Yoon YI, Lee SG, Moon DB, Ahn CS, Hwang S, Kim KH, et al. 2019; Surgical techniques and long-term outcomes of living-donor liver transplantation with inferior vena cava replacement using atriocaval synthetic interposition graft for Budd-Chiari syndrome. Ann Surg. 269:e43–5. DOI: 10.1097/SLA.0000000000002847. PMID: 30080720.
Article13. Yoon YI, Lee SG. 2019; Living donor liver transplantation for hepatocellular carcinoma: an Asian perspective. Dig Dis Sci. 64:993–1000. DOI: 10.1007/s10620-019-05551-4. PMID: 30895483.
Article14. Li H, Yang Z, Tian F. 2019; Clinical characteristics and risk factors for sinistral portal hypertension associated with moderate and severe acute pancreatitis: a seven-year single-center retrospective study. Med Sci Monit. 25:5969–76. DOI: 10.12659/MSM.916192. PMID: 31400275. PMCID: PMC6699198.
Article15. Reddy K, Mallett S, Peachey T. 2005; Venovenous bypass in orthotopic liver transplantation: time for a rethink? Liver Transpl. 11:741–9. DOI: 10.1002/lt.20482. PMID: 15973707.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Technical Feasibility of Living Donor Liver Transplantation after Prior Major Liver Resection for Hepatocellular Carcinoma
- Minimal-incision donor right hepatectomy for living donor liver transplantation
- Left lobe living donor liver transplantation using the resection and partial liver segment 2–3 transplantation with delayed total hepatectomy (RAPID) procedure in cirrhotic patients: First case report in Korea
- Recipient liver splitting to facilitate piggyback hepatectomy in adult living donor liver transplantation
- Technical refinement of inferior vena cava replacement using a synthetic vascular graft in living donor liver transplantation