Korean J Transplant.
2021 Jun;35(2):124-129. 10.4285/kjt.20.0055.
Recipient liver splitting to facilitate piggyback hepatectomy in adult living donor liver transplantation
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2517296
- DOI: http://doi.org/10.4285/kjt.20.0055
Abstract
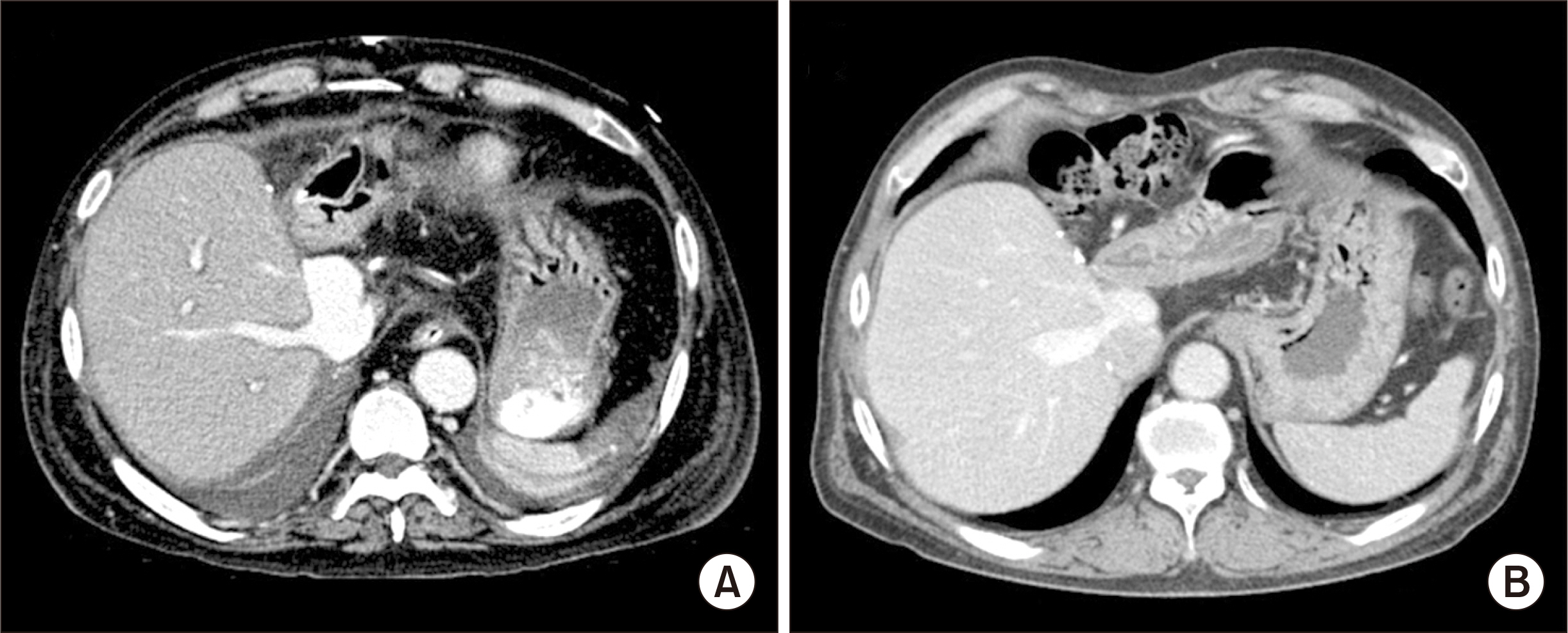
- Recipient hepatectomy for an enlarged stony-hard liver is a demanding procedure, thus it is often accompanied by massive blood loss. Recipient liver splitting under prolonged hepatic inflow occlusion would facilitate the piggyback recipient hepatectomy. We herein present a case of recipient liver splitting, which was used for living donor liver transplantation (LDLT). A 48-year-old male patient diagnosed with acute-on-chronic liver failure underwent LDLT. During the recipient operation, the native liver was stony-hard and heavily adherent to the retrohepatic inferior vena cava (IVC). During liver mobilization, diffuse oozing occurred due to disseminated intravascular coagulation. As a change in the concept, we decided to perform in situ liver splitting of the recipient liver to facilitate dissection of the retrohepatic IVC. Under hepatic inflow occlusion, right-left liver splitting was performed along the usual plane of extended left hepatectomy. The procedures time for recipient liver splitting and removal was 60 minutes. A modified right liver graft recovered from his daughter was implanted according to the standard procedures of LDLT. We think that recipient liver splitting is a feasible technical option for coping with difficult recipient hepatectomy, especially in patients with an enlarged stony-hard liver and heavy adhesion around the IVC.
Figure
Reference
-
1. Hwang S, Moon DB, Lee SG. 2010; Liver transplantation and conventional surgery for advanced hepatocellular carcinoma. Transpl Int. 23:723–7. DOI: 10.1111/j.1432-2277.2010.01103.x. PMID: 20477996.
Article2. Jabir MA, Hamza HM, Fakhry H, Amira G, Hatano E, Uemoto S. 2017; Anterior versus conventional approach for resection of large right lobe hepatocellular carcinoma. J Gastrointest Cancer. 48:25–30. DOI: 10.1007/s12029-016-9865-x. PMID: 27506210.
Article3. Choi JU, Hwang S, Chung IJ, Kang SH, Ahn CS, Moon DB, et al. 2020; Prolonged hepatic inflow occlusion to reduce bleeding during recipient hepatectomy in living donor liver transplantation. Korean J Transplant. 34:55–61.4. Choi JU, Hwang S, Ahn CS, Moon DB, Ha TY, Kim KH, et al. 2019; Prolonged occlusion of the hepatoduodenal ligament to reduce risk of bleeding and tumor spread during recipient hepatectomy for living donor liver transplantation. Ann Hepatobiliary Pancreat Surg. 23:61–4. DOI: 10.14701/ahbps.2019.23.1.61. PMID: 30863809. PMCID: PMC6405371.
Article5. Lee SG, Song GW, Yoon YI. 2019; An exceptional series: 5000 living donor liver transplantations at Asan Medical Center, Seoul, Korea. Transplantation. 103:1739–41. DOI: 10.1097/TP.0000000000002708. PMID: 31461082.
Article6. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. 2006; Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 12:920–7. DOI: 10.1002/lt.20734. PMID: 16721780.
Article7. Pustavoitau A, Lesley M, Ariyo P, Latif A, Villamayor AJ, Frank SM, et al. 2017; Predictive modeling of massive transfusion requirements during liver transplantation and its potential to reduce utilization of blood bank resources. Anesth Analg. 124:1644–52. DOI: 10.1213/ANE.0000000000001994. PMID: 28426586.
Article8. Donohue CI, Mallett SV. 2015; Reducing transfusion requirements in liver transplantation. World J Transplant. 5:165–82. DOI: 10.5500/wjt.v5.i4.165. PMID: 26722645. PMCID: PMC4689928.
Article9. Steib A, Freys G, Lehmann C, Meyer C, Mahoudeau G. 2001; Intraoperative blood losses and transfusion requirements during adult liver transplantation remain difficult to predict. Can J Anaesth. 48:1075–9. DOI: 10.1007/BF03020372. PMID: 11744582.
Article10. Massicotte L, Beaulieu D, Roy JD, Marleau D, Vandenbroucke F, Dagenais M, et al. 2009; MELD score and blood product requirements during liver transplantation: no link. Transplantation. 87:1689–94. DOI: 10.1097/TP.0b013e3181a5e5f1. PMID: 19502961.
Article11. Pinto MA, Chedid MF, Sekine L, Schmidt AP, Capra RP, Prediger C, et al. 2019; Intraoperative cell salvage with autologous transfusion in liver transplantation. World J Gastrointest Surg. 11:11–8. DOI: 10.4240/wjgs.v11.i1.11. PMID: 30705735. PMCID: PMC6354069.
Article12. Park YK, Kim BW, Wang HJ, Xu W. 2012; Usefulness of the Pinch-Burn-Cut (PBC) technique for recipient hepatectomy in liver transplantation. Korean J Hepatobiliary Pancreat Surg. 16:13–6. DOI: 10.14701/kjhbps.2012.16.1.13. PMID: 26388900. PMCID: PMC4575015.
Article13. Lee KW, Joh JW, Kim SJ, Choi SH, Heo JS, Lee HH, et al. 2004; High hilar dissection: new technique to reduce biliary complication in living donor liver transplantation. Liver Transpl. 10:1158–62. DOI: 10.1002/lt.20230. PMID: 15350008.
Article14. Verran DJ, Gurkan A, Chui AK, Dilworth P, Koorey D, McCaughan G, et al. 2000; Pancreatitis in adult orthotopic liver allograft recipients: risk factors and outcome. Liver Transpl. 6:362–6. DOI: 10.1053/lv.2000.5203. PMID: 10827240.
Article15. Smyrniotis VE, Kostopanagiotou GG, Gamaletsos EL, Vassiliou JG, Voros DC, Fotopoulos AC, et al. 2002; Total versus selective hepatic vascular exclusion in major liver resections. Am J Surg. 183:173–8. DOI: 10.1016/S0002-9610(01)00864-9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimal-incision donor right hepatectomy for living donor liver transplantation
- Diaphragmatic herniation following donor hepatectomy for living donor liver transplantation: a serious complication not given due recognition
- Split liver transplantation for two adult recipients: A collective review of Korean experience
- Technical refinement of the anterior sectional drainage in right liver transplantation: a single center experience
- Decreasing the operation time of living donor liver transplantation in the era of laparoscopic living donor hepatectomy