Ann Hepatobiliary Pancreat Surg.
2024 Aug;28(3):388-392. 10.14701/ahbps.24-005.
Left lobe living donor liver transplantation using the resection and partial liver segment 2–3 transplantation with delayed total hepatectomy (RAPID) procedure in cirrhotic patients: First case report in Korea
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2558650
- DOI: http://doi.org/10.14701/ahbps.24-005
Abstract
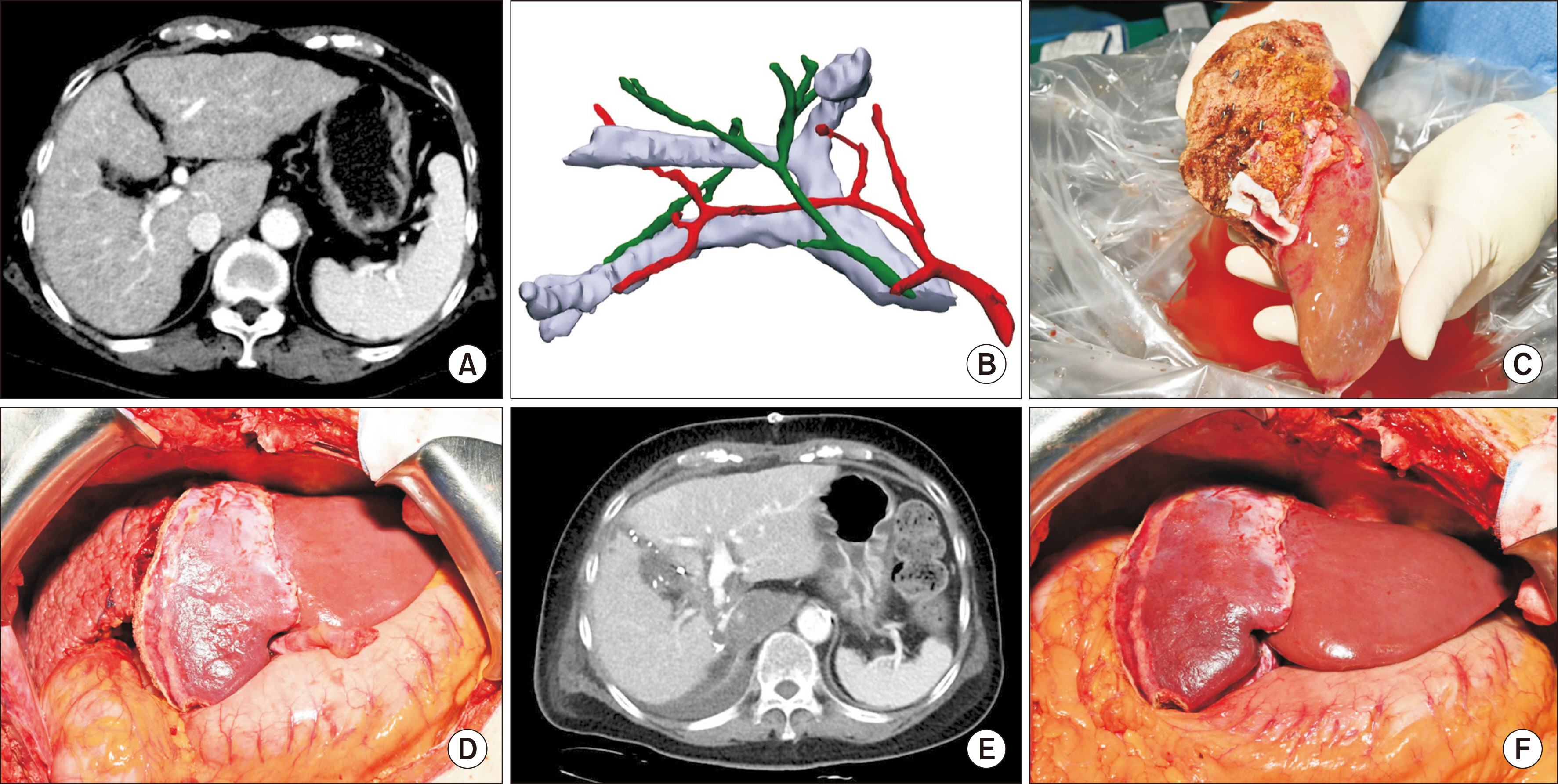
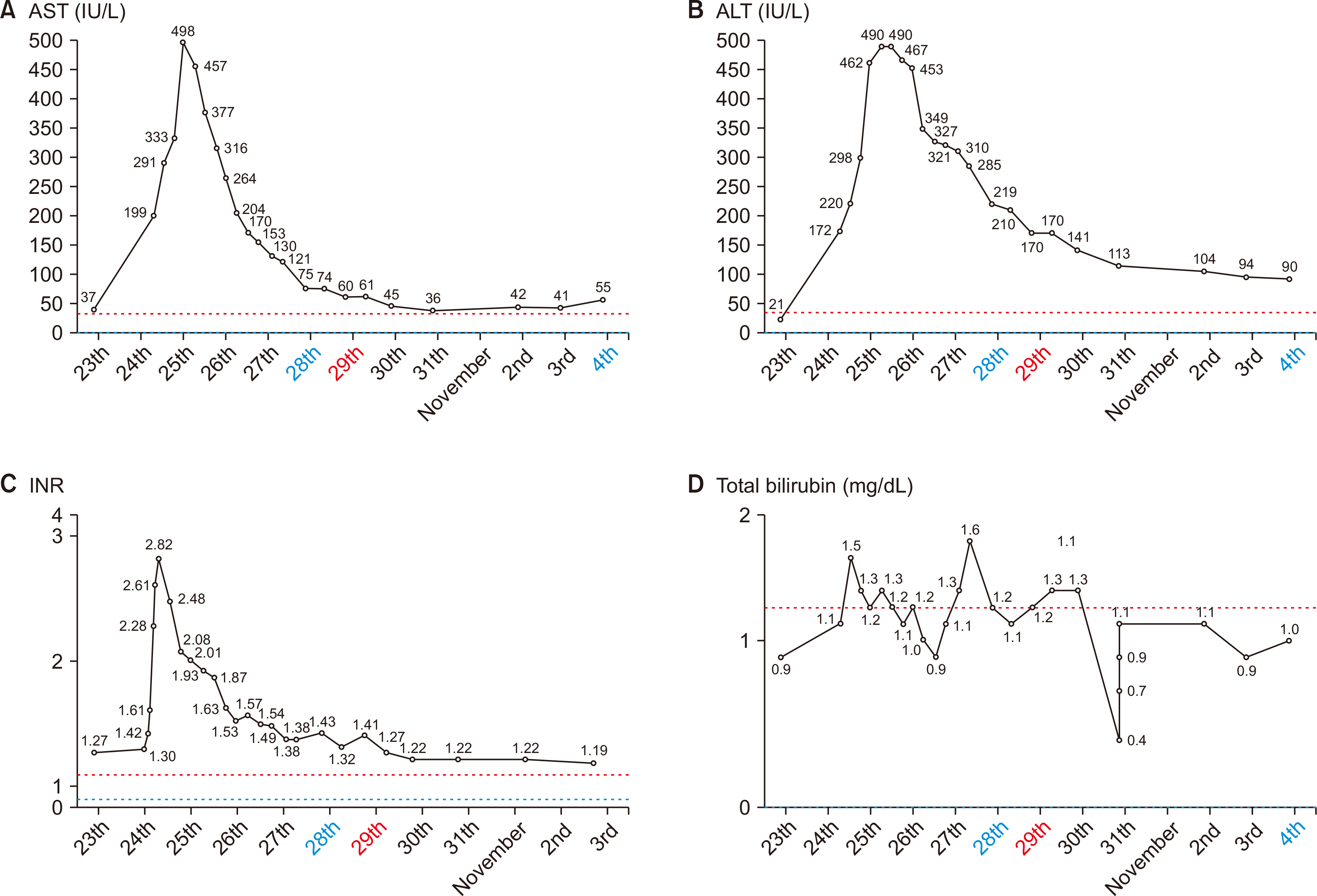
- In liver transplantation, the primary concern is to ensure an adequate future liver remnant (FLR) volume for the donor, while selecting a graft of sufficient size for the recipient. The living donor–resection and partial liver segment 2−3 transplantation with delayed total hepatectomy (LD−RAPID) procedure offers a potential solution to expand the donor pool for living donor liver transplantation (LDLT). We report the first case involving a cirrhotic patient with autoimmune hepatitis and hepatocellular carcinoma, who underwent left lobe LDLT using the LD−RAPID procedure. The living liver donor (LLD) underwent a laparoscopic left hepatectomy, including middle hepatic vein. The resection on the recipient side was an extended left hepatectomy, including the middle hepatic vein orifice and caudate lobe. At postoperative day 7, a computed tomography scan showed hypertrophy of the left graft from 320 g to 465 mL (i.e., a 45.3% increase in graft volume body weight ratio from 0.60% to 0.77%). After a 7-day interval, the diseased right lobe was removed in the second stage surgery. The LD−RAPID procedure using left lobe graft allows for the use of a small liver graft or small FLR volume in LLD in LDLT, which expands the donor pool to minimize the risk to LLD by enabling the donation of a smaller liver portion.
Figure
Reference
-
References
1. Choi JY, Kim JH, Kim JM, Kim HJ, Ahn HS, Joh JW. 2022; Outcomes of living liver donors are worse than those of matched healthy controls. J Hepatol. 76:628–638. DOI: 10.1016/j.jhep.2021.10.031. PMID: 34785324.2. Kow AWC, Liu J, Patel MS, De Martin E, Reddy MS, Soejima Y, et al. 2023; Post living donor liver transplantation small-for-size syndrome: definitions, timelines, biochemical, and clinical factors for diagnosis: guidelines from the ILTS-iLDLT-LTSI consensus conference. Transplantation. 107:2226–2237. DOI: 10.1097/TP.0000000000004770. PMID: 37749812.3. Kirchner VA, Shankar S, Victor DW 3rd, Tanaka T, Goldaracena N, Troisi RI, et al. 2023; Management of established small-for-size syndrome in post living donor liver transplantation: medical, radiological, and surgical interventions: guidelines from the ILTS-iLDLT-LTSI consensus conference. Transplantation. 107:2238–2246. DOI: 10.1097/TP.0000000000004771. PMID: 37749813.4. Balci D, Kirimker EO, Kologlu MB, Ustuner E, Erkoc SK, Cinar G, et al. 2022; Left lobe living donor liver transplantation using rapid procedure in a cirrhotic patient with portal vein thrombosis. Ann Surg. 275:e538–e539. DOI: 10.1097/SLA.0000000000005107. PMID: 34334650.5. Königsrainer A, Templin S, Capobianco I, Königsrainer I, Bitzer M, Zender L, et al. 2019; Paradigm shift in the management of irresectable colorectal liver metastases: living donor auxiliary partial orthotopic liver transplantation in combination with two-stage hepatectomy (LD-RAPID). Ann Surg. 270:327–332. DOI: 10.1097/SLA.0000000000002861. PMID: 29916882.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic living donor hepatectomy
- Postoperative Liver Regeneration and Complication In Live Liver Donor after Partial Hepatectomy for Living Donor Liver Transplantation
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Two-stage liver transplantation in a surgically complicated liver failure patient after hepatic tumor resection: A case report
- Resection or transplantation for perihilar cholangiocarcinoma