Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004–2018
- Affiliations
-
- 1National Cancer Control Institute, National Cancer Center, Goyang, Korea
- KMID: 2514916
- DOI: http://doi.org/10.4143/crt.2020.263
Abstract
- Purpose
The Korean National Cancer Screening Survey (KNCSS) is a nationwide annual cross-sectional survey conducted for the past 15 years. This study aimed to report trends in the overall screening rates of both organized and opportunistic cancer screening programs from 2004–2018.
Materials and Methods
KNCSS data were collected using a structured questionnaire. For five major cancers (i.e., stomach, liver, colorectal, breast, and cervical cancer), we evaluated both the lifetime screening rate and the screening rate with recommendations. The study population included men aged 40–74 years and women aged 20–74 years with no cancer histories.
Results
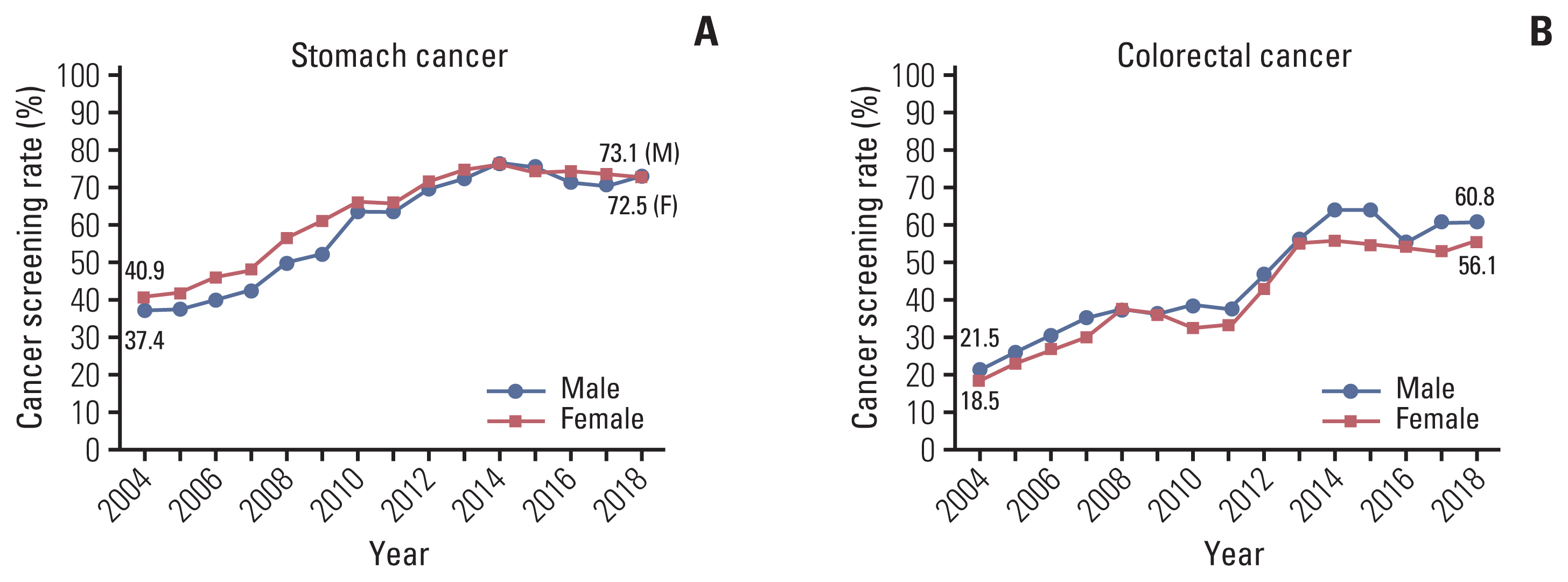
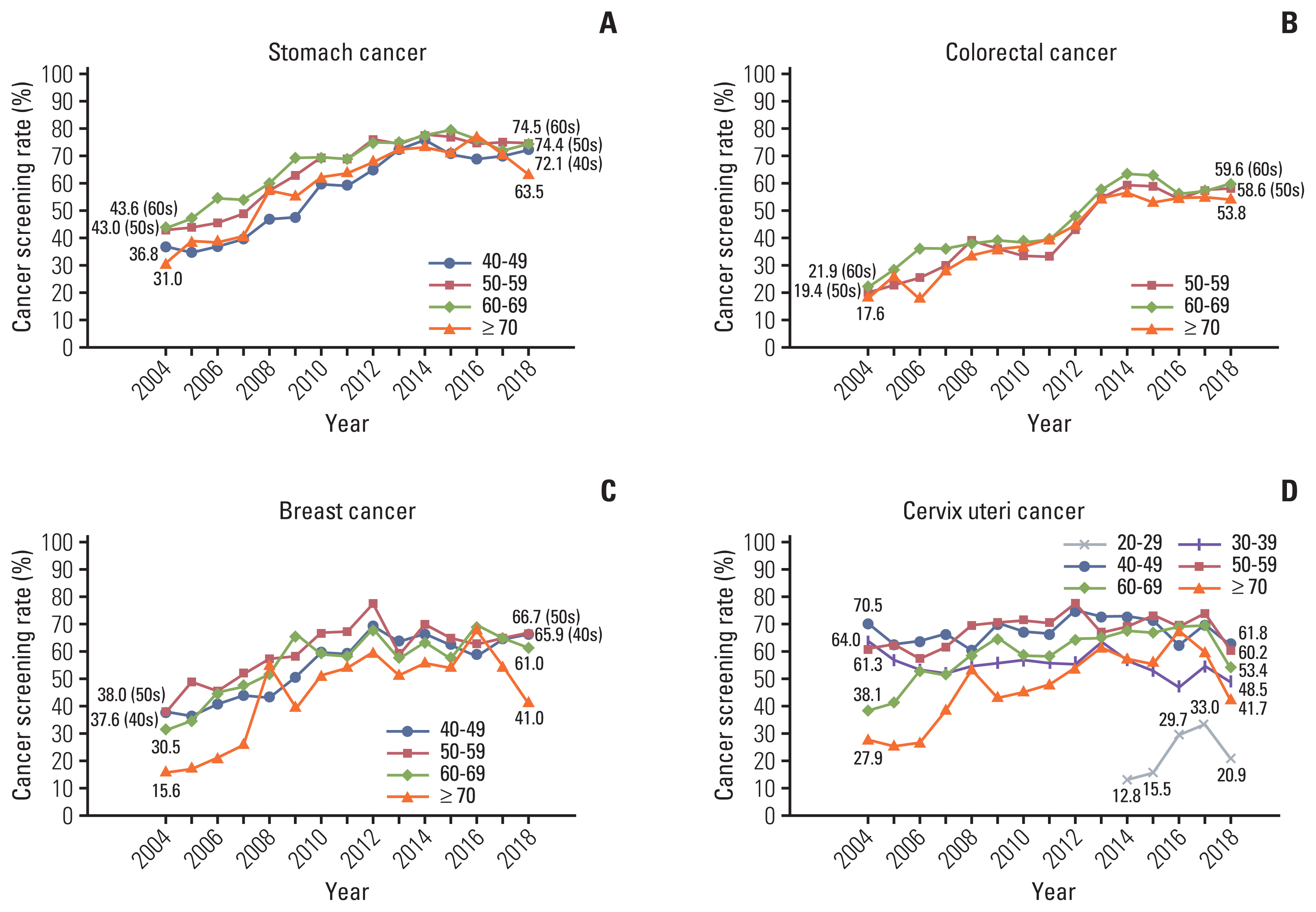
Screening rate with recommendations increased from 2004 annually by 4.4% and 1.5% until 2013 for stomach and liver cancers, respectively, by 4.0% until 2012 for breast cancer, and by 3.6% and 1.2% until 2014 for colorectal and cervical cancers, respectively, followed by nonsignificant trends thereafter. In 2018, screening rates with recommendations for these cancers were 72.8%, 26.2%, 63.1%, 58.4%, and 55.6%, respectively.
Conclusion
Screening rates for the five types of cancer demonstrated a marked increase between 2004 and 2018. However, many recent screening rates have been flattened with nonsignificant trends, and there are lower rates for cervical cancer screening among young age groups. Steady efforts are needed to achieve higher screening participation rates overall, especially for the cervical cancer screening of young women in their 20s.
Keyword
Figure
Cited by 3 articles
-
Overview of the National Cancer Screening Program for Colorectal Cancer in Korea over 14 Years (2004–2017)
Bomi Park, Eun Young Her, Kyeongmin Lee, Fatima Nari, Jae Kwan Jun, Kui Son Choi, Mina Suh
Cancer Res Treat. 2023;55(3):910-917. doi: 10.4143/crt.2022.1432.Temporal Trend in Uptake of the National General Health Checkups and Cancer Screening Program among Korean Women with Breast Cancer
Thi Xuan Mai Tran, Soyeoun Kim, Chihwan Cha, Boyoung Park
Cancer Res Treat. 2024;56(2):522-530. doi: 10.4143/crt.2023.729.Determinants of Prostate Cancer Screening in Korean Men: A Nationwide Study Using the Korean National Cancer Screening Survey 2023
Giap Viet Nguyen, Kyeongmin Lee, Hyeon Ji Lee, EunKyo Kang, Mina Suh, Jae Kwan Jun, Kui Son Choi
Cancer Res Treat. 2025;57(2):539-546. doi: 10.4143/crt.2024.879.
Reference
-
References
1. Jung KW, Won YJ, Kong HJ, Lee ES. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2016. Cancer Res Treat. 2019; 51:417–30.
Article2. Lee KS, Chang HS, Lee SM, Park EC. Economic burden of cancer in Korea during 2000–2010. Cancer Res Treat. 2015; 47:387–98.
Article3. Suh M, Choi KS, Park B, Lee YY, Jun JK, Lee DH, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004–2013. Cancer Res Treat. 2016; 48:1–10.
Article4. Suh M, Choi KS, Lee YY, Park B, Jun JK. Cancer screening in Korea, 2012: results from the Korean National Cancer Screening Survey. Asian Pac J Cancer Prev. 2013; 14:6459–63.
Article5. Surveillance Research Program Joinpoint trend analysis software, version 4801 [Internet]. Bethesda, MD: National Cancer Institute;2020. [cited 2020 May 14]. Available from: https://surveillance.cancer.gov/joinpoint/ .6. Screening and Immunisations Team, NHS Digital. Breast Screening Programme England, statistics for 2017–18 [Internet]. London: Health and Social Care Information Centre;2019. [cited 2020 Jun 30]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/breast-screening-programme .7. Screening and Immunisations Team, NHS Digital. Cervical Screening Programme England, statistics for 2017–18 [Internet]. London: Health and Social Care Information Centre;2018. [cited 2020 Jun 30]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-programme .8. Smith RA, Andrews KS, Brooks D, Fedewa SA, Manassaram-Baptiste D, Saslow D, et al. Cancer screening in the United States, 2018: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. 2018; 68:297–316.
Article9. Sauvaget C, Nishino Y, Konno R, Tase T, Morimoto T, Hisamichi S. Challenges in breast and cervical cancer control in Japan. Lancet Oncol. 2016; 17:e305–12.
Article10. Yoshida M, Kondo K, Tada T. The relation between the cancer screening rate and the cancer mortality rate in Japan. J Med Invest. 2010; 57:251–9.11. Summary report of comprehensive survey of living conditions 2016 [Internet]. Tokyo: Ministry of Health, Labour and Welfare, Household Statistics Office;2017. [cited 2020 Jun 2]. Available from: https://www.mhlw.go.jp/english/database/db-hss/cslc-report2016.html .12. Uchida K, Ohashi H, Kinoshita S, Nogi H, Kato K, Toriumi Y, et al. Breast cancer screening and the changing population pyramid of Japan. Breast Cancer. 2015; 22:172–6.
Article13. Matsuura Y, Yoshioka M, Nakata A, Haraga M, Hachisuga T, Mori K. Trends in uterine cervical cancer screening at physical health checkups for company employees in Japan. J UOEH. 2019; 41:327–33.
Article14. Hamashima C, Goto R. Potential capacity of endoscopic screening for gastric cancer in Japan. Cancer Sci. 2017; 108:101–7.
Article15. Sano Y, Byeon JS, Li XB, Wong MC, Chiu HM, Rerknimitr R, et al. Colorectal cancer screening of the general population in East Asia. Dig Endosc. 2016; 28:243–9.
Article16. Snijders PJ, Verhoef VM, Arbyn M, Ogilvie G, Minozzi S, Banzi R, et al. High-risk HPV testing on self-sampled versus clinician-collected specimens: a review on the clinical accuracy and impact on population attendance in cervical cancer screening. Int J Cancer. 2013; 132:2223–36.17. Braz NS, Lorenzi NP, Sorpreso IC, Aguiar LM, Baracat EC, Soares-Junior JM. The acceptability of vaginal smear self-collection for screening for cervical cancer: a systematic review. Clinics (Sao Paulo). 2017; 72:183–7.
Article18. Carrasquillo O, Seay J, Amofah A, Pierre L, Alonzo Y, McCann S, et al. HPV Self-sampling for cervical cancer screening among ethnic minority women in South Florida: a randomized trial. J Gen Intern Med. 2018; 33:1077–83.
Article19. Jager M, Demb J, Asghar A, Selby K, Mello EM, Heskett KM, et al. Mailed outreach is superior to usual care alone for colorectal cancer screening in the USA: a systematic review and meta-analysis. Dig Dis Sci. 2019; 64:2489–96.
Article20. Davis MM, Freeman M, Shannon J, Coronado GD, Stange KC, Guise JM, et al. A systematic review of clinic and community intervention to increase fecal testing for colorectal cancer in rural and low-income populations in the United States: how, what and when? BMC Cancer. 2018; 18:40.
Article21. Hong S, Shin HY, Lee B, Hwang NR, Hwang SH, Jun JK. Increase in the colorectal cancer screening rate by a round-mailed fecal immunochemical testing kit and associated factors in underserved regions of Korea: a community-based intervention study. Gut Liver. 2020; 14:323–30.
Article22. Shim SH, Kim H, Sohn IS, Hwang HS, Kwon HS, Lee SJ, et al. Nationwide cervical cancer screening in Korea: data from the National Health Insurance Service Cancer Screening Program and National Cancer Screening Program, 2009–2014. J Gynecol Oncol. 2017; 28:e63.
Article23. Lee EY, Lee YY, Suh M, Choi E, Mai TTX, Cho H, et al. Socioeconomic inequalities in stomach cancer screening in Korea, 2005–2015: after the introduction of the National Cancer Screening Program. Yonsei Med J. 2018; 59:923–9.
Article24. Cho YH, Kim DH, Cha JM, Jeen YT, Moon JS, Kim JO, et al. Patients’ preferences for primary colorectal cancer screening: a survey of the National Colorectal Cancer Screening Program in Korea. Gut Liver. 2017; 11:821–7.
Article25. Tsuruda KM, Sagstad S, Sebuodegard S, Hofvind S. Validity and reliability of self-reported health indicators among women attending organized mammographic screening. Scand J Public Health. 2018; 46:744–51.
Article26. Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of women’s self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiol Biomarkers Prev. 2003; 12:1182–7.27. Baier M, Calonge N, Cutter G, McClatchey M, Schoentgen S, Hines S, et al. Validity of self-reported colorectal cancer screening behavior. Cancer Epidemiol Biomarkers Prev. 2000; 9:229–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in Cancer-Screening Rates in Korea: Findings from the National Cancer Screening Survey, 2004-2023
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2011
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey (KNCSS), 2004-2010
- Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004-2013
- Trends in Cancer Screening Rates among Korean Men and Women: Results from the Korean National Cancer Screening Survey, 2004-2012