Korean Circ J.
2021 Apr;51(4):336-348. 10.4070/kcj.2020.0430.
Effects of Smoking on Long-Term Clinical Outcomes and Lung Cancer in Patients with Acute Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Cardiology, Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Uijeongbu St Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Cardiology, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Division of Cardiology, Department of Internal Medicine, Daejeon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 6Division of Cardiology, Department of Internal Medicine, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 7Division of Cardiology, Department of Internal Medicine, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 8Cardiovascular Center, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2514637
- DOI: http://doi.org/10.4070/kcj.2020.0430
Abstract
- Background and Objectives
Smoking is well-established as a risk factor for coronary artery disease. However, recent studies demonstrated favorable results, including reduced mortality, among smokers, which are referred to as the “smoker's paradox”. This study examined the impact of smoking on clinical outcomes in patients with acute myocardial infarction (AMI) undergoing percutaneous coronary intervention (PCI).
Methods
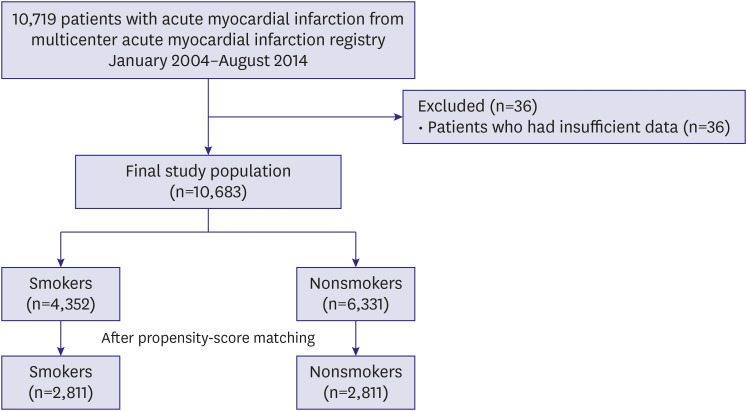
Patients with AMI undergoing PCI between 2004 and 2014 were enrolled and classified according to smoking status. The primary endpoint was a composite of major adverse cardiovascular events (MACE) including cardiac death, myocardial infarction, stroke, and revascularization.
Results
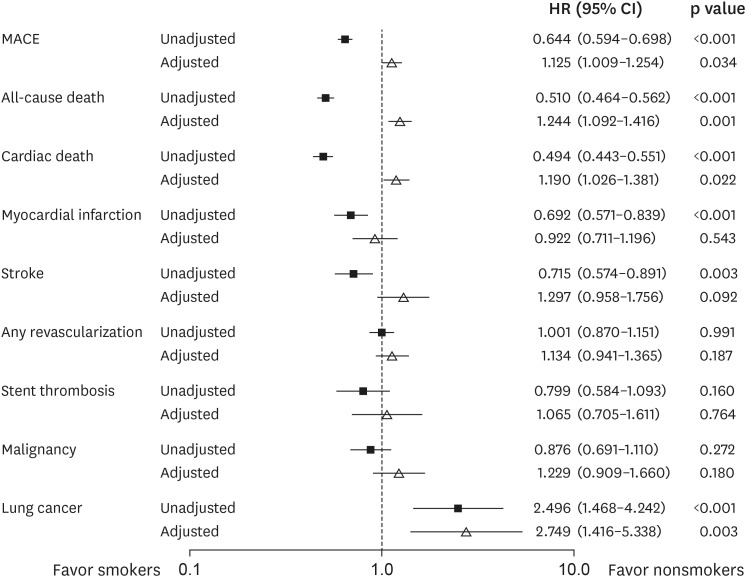
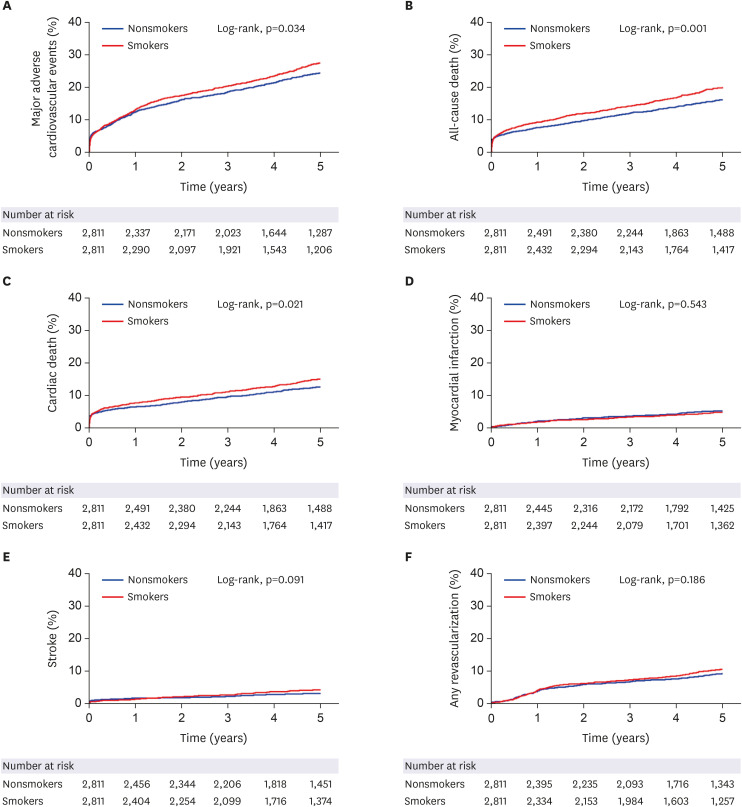
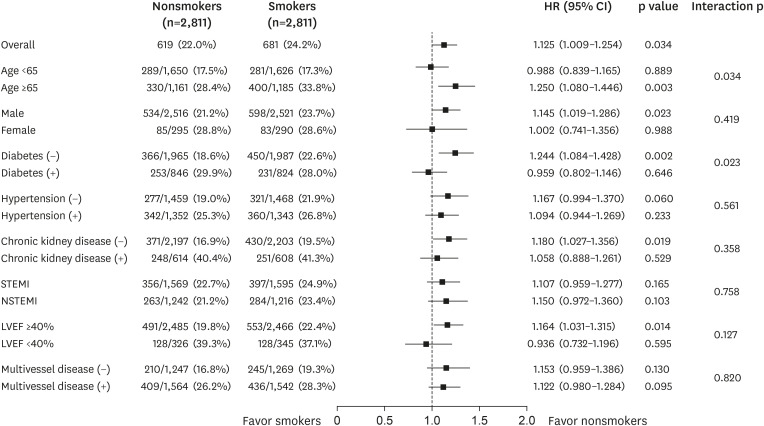
Among the 10,683 patients, 4,352 (40.7%) were current smokers. Smokers were 10.7 years younger and less likely to have comorbidities such as hypertension, diabetes mellitus, chronic kidney disease, stroke, and prior PCI. Smokers had less MACE (hazard ratio [HR], 0.644; 95% confidence interval [CI], 0.594–0.698; p<0.001) and cardiac death (HR, 0.494; 95% CI, 0.443–0.551; p<0.001) compared to nonsmokers during the 5 years in an unadjusted model. However, after propensity-score matching, smokers showed higher risk of MACE (HR, 1.125; 95% CI, 1.009–1.254; p=0.034) and cardiac death (HR, 1.190; 95% CI, 1.026–1.381; p=0.022). Smoking was a strong independent predictor of lung cancer (propensityscore matched HR, 2.749; 95% CI, 1.416–5.338; p=0.003).
Conclusions
In contrast to the unadjusted model, smoking is associated with worse cardiovascular outcome and higher incidence of lung cancer after adjustment of various confounding factors. This result can be explained by the characteristics of smokers, which were young and had fewer comorbidities.
Figure
Cited by 1 articles
-
New Insights on Mechanisms of Nicotine in Neointimal Hyperplasia
Weon Kim
Korean Circ J. 2024;55(1):65-66. doi: 10.4070/kcj.2024.0326.
Reference
-
1. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013; 368:341–350. PMID: 23343063.2. Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004; 43:1731–1737. PMID: 15145091.3. Ezzati M, Henley SJ, Thun MJ, Lopez AD. Role of smoking in global and regional cardiovascular mortality. Circulation. 2005; 112:489–497. PMID: 16027251.4. Gu D, Kelly TN, Wu X, et al. Mortality attributable to smoking in China. N Engl J Med. 2009; 360:150–159. PMID: 19129528.5. Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013; 368:351–364. PMID: 23343064.6. Barbash GI, Reiner J, White HD, et al. Evaluation of paradoxic beneficial effects of smoking in patients receiving thrombolytic therapy for acute myocardial infarction: mechanism of the “smoker's paradox” from the GUSTO-I trial, with angiographic insights. Global Utilization of Streptokinase and Tissue-Plasminogen Activator for Occluded Coronary Arteries. J Am Coll Cardiol. 1995; 26:1222–1229. PMID: 7594035.7. Andrikopoulos GK, Richter DJ, Dilaveris PE, et al. In-hospital mortality of habitual cigarette smokers after acute myocardial infarction; the “smoker's paradox” in a countrywide study. Eur Heart J. 2001; 22:776–784. PMID: 11350110.8. Finney Rutten LJ, Augustson EM, Moser RP, Beckjord EB, Hesse BW. Smoking knowledge and behavior in the United States: sociodemographic, smoking status, and geographic patterns. Nicotine Tob Res. 2008; 10:1559–1570. PMID: 18946775.9. Cheng HG, McBride O, Phillips MR. Relationship between knowledge about the harms of smoking and smoking status in the 2010 Global Adult Tobacco China Survey. Tob Control. 2015; 24:54–61. PMID: 23988861.10. Yadav M, Mintz GS, Généreux P, et al. The smoker's paradox revisited: a patient-level pooled analysis of 18 randomized controlled trials. JACC Cardiovasc Interv. 2019; 12:1941–1950. PMID: 31521646.11. Robertson JO, Ebrahimi R, Lansky AJ, Mehran R, Stone GW, Lincoff AM. Impact of cigarette smoking on extent of coronary artery disease and prognosis of patients with non-ST-segment elevation acute coronary syndromes: an analysis from the ACUITY Trial (Acute Catheterization and Urgent Intervention Triage Strategy). JACC Cardiovasc Interv. 2014; 7:372–379. PMID: 24630881.12. Redfors B, Furer A, Selker HP, et al. Effect of smoking on outcomes of primary PCI in patients with STEMI. J Am Coll Cardiol. 2020; 75:1743–1754. PMID: 32299585.13. Parasuraman S, Zaman AG, Egred M, et al. Smoking status and mortality outcomes following percutaneous coronary intervention. Eur J Prev Cardiol. 2020.14. Gupta T, Kolte D, Khera S, et al. Smoker's paradox in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. J Am Heart Assoc. 2016; 5:e003370. PMID: 27107131.15. Steele L, Palmer J, Lloyd A, Fotheringham J, Iqbal J, Grech ED. The impact of smoking on mortality after acute ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: a retrospective cohort outcome study at 3 years. J Thromb Thrombolysis. 2019; 47:520–526. PMID: 30666553.16. Song C, Fu R, Dou K, et al. Association between smoking and in-hospital mortality in patients with acute myocardial infarction: results from a prospective, multicentre, observational study in China. BMJ Open. 2019; 9:e030252.17. Gottlieb S, Boyko V, Zahger D, et al. Smoking and prognosis after acute myocardial infarction in the thrombolytic era (Israeli Thrombolytic National Survey). J Am Coll Cardiol. 1996; 28:1506–1513. PMID: 8917265.18. Jørgensen , Køber L, Ottesen MM, Torp-Pedersen C, Videbaek J, Kjøller E. The prognostic importance of smoking status at the time of acute myocardial infarction in 6676 patients. TRACE Study Group. J Cardiovasc Risk. 1999; 6:23–27. PMID: 10197289.19. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018; 72:2231–2264. PMID: 30153967.20. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines and the society for cardiovascular angiography and interventions. Circulation. 2011; 124:e574–651. PMID: 22064601.21. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019; 40:87–165. PMID: 30165437.22. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2013; 127:e362–425. PMID: 23247304.23. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014; 130:2354–2394. PMID: 25249586.24. Benowitz NL, Fitzgerald GA, Wilson M, Zhang Q. Nicotine effects on eicosanoid formation and hemostatic function: comparison of transdermal nicotine and cigarette smoking. J Am Coll Cardiol. 1993; 22:1159–1167. PMID: 7691912.25. Michael Pittilo R. Cigarette smoking, endothelial injury and cardiovascular disease. Int J Exp Pathol. 2000; 81:219–230. PMID: 10971743.26. Nicod P, Rehr R, Winniford MD, Campbell WB, Firth BG, Hillis LD. Acute systemic and coronary hemodynamic and serologic responses to cigarette smoking in long-term smokers with atherosclerotic coronary artery disease. J Am Coll Cardiol. 1984; 4:964–971. PMID: 6548482.27. Zhang YJ, Iqbal J, van Klaveren D, et al. Smoking is associated with adverse clinical outcomes in patients undergoing revascularization with PCI or CABG: the SYNTAX trial at 5-year follow-up. J Am Coll Cardiol. 2015; 65:1107–1115. PMID: 25790882.28. Hasdai D, Garratt KN, Grill DE, Lerman A, Holmes DR Jr. Effect of smoking status on the long-term outcome after successful percutaneous coronary revascularization. N Engl J Med. 1997; 336:755–761. PMID: 9052653.29. Sherif MA, Nienaber CA, Toelg R, et al. Impact of smoking on the outcome of patients treated with drug-eluting stents: 1-year results from the prospective multicentre German Drug-Eluting Stent Registry (DES.DE). Clin Res Cardiol. 2011; 100:413–423. PMID: 21116637.30. Shi JF, Liu CC, Ren JS, et al. Economic burden of lung cancer attributable to smoking in China in 2015. Tob Control. 2020; 29:191–199. PMID: 31073096.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cardiac Metastasis from Lung Cancer Presented with Persistent ST Segment Elevation Simulating Acute Myocardial Infarction
- Can time delay be shortened in the treatment of acute myocardial infarction?: Experience from Korea acute myocardial infarction registry
- Management of long-term lung cancer survivors in Korea
- Clinical Study of Risk Factors in Patients with Acute Myocardial Infarction
- Long-term outcomes in ST-elevation myocardial infarction patients treated according to hospital visit time