Anat Cell Biol.
2021 Mar;54(1):10-17. 10.5115/acb.20.179.
Defining the popliteal fossa by bony landmarks and mapping of the courses of the neurovascular structures for application in popliteal fossa surgery
- Affiliations
-
- 1Department of Anatomy, School of Medicine, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa
- 2Department of Anatomy and Cellular Biology, College of Medicine and Health Sciences, Khalifa University, Abu Dhabi, United Arab Emirates
- 3Department of Orthopaedic Surgery and Sports Medicine, Burjeel Hospital for Advanced Surgery, Dubai, United Arab Emirates
- 4Medical School, University of Pretoria, Pretoria, South Africa
- KMID: 2514577
- DOI: http://doi.org/10.5115/acb.20.179
Abstract
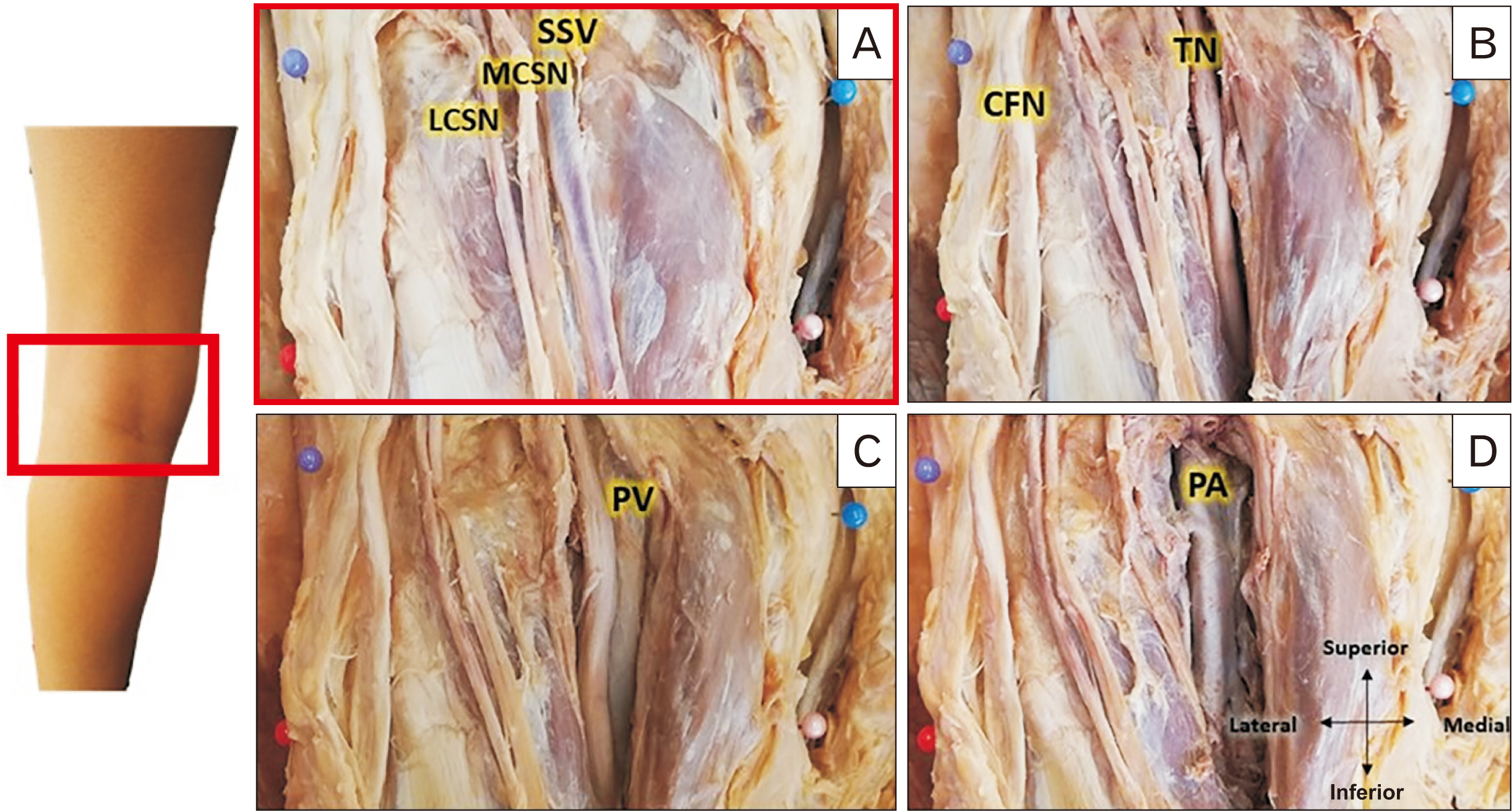
- Surgical access to the posterior knee poses a high-risk for neurovascular damage. The study aimed to define the popliteal fossa by reliable bony landmarks and comprehensively mapping the neurovascular structures for application in posterior knee surgery. Forty-five (20 male, 25 female) embalmed adult cadaveric knees were included. The position of the small saphenous vein (SSV), medial cutaneous sural nerve (MCSN) and lateral cutaneous sural nerv (LCSN), tibial nerve (TN) and common fibular nerve (CFN) nerves, and popliteal vein (PV) and popliteal artery (PA) were determined in relation to either medial (MFE) or lateral (LFE) femoral epicondyles, medial (MTC) and lateral (LTC) tibial condyles and the midpoint between the MFE and MTC and LFEF and LTC. The distance between the MFE and the PA, PV, TN, MCSN, and SSV was 38.4±12.1 mm, 38.4±12.9 mm, 39.4±10.2 mm, 39.2±14.0 mm and 37.6±12.5 mm respectively for males and 34.6±4.9 mm, 32.8±5.6 mm and 38.0±8.1 mm 38.8±10.1 mm and 37.9±8.2 mm respectively for females. The distance between LFE and the CFN and LCSN was 13.4±8.2 mm and 24.9±7.3 mm respectively for males and 8.4±9.1 mm and 18.4±10.4 mm respectively in females. This study defined the popliteal fossa by reliable bony landmarks and provided a comprehensive map of the neurovascular structures and will help to avoid injuries to the important neurovascular structures.
Keyword
Figure
Reference
-
References
1. Faucett SC, Gannon J, Chahla J, Ferrari MB, LaPrade RF. 2017; Posterior surgical approach to the knee. Arthrosc Tech. 6:e391–5. DOI: 10.1016/j.eats.2016.10.013. PMID: 28580257. PMCID: PMC5443038.
Article2. Alpert JM, McCarty LP, Bach BR Jr. 2008; The direct posterior approach to the knee: surgical and anatomic approach. J Knee Surg. 21:44–9. DOI: 10.1055/s-0030-1247791. PMID: 18300671.
Article3. Dagur G, Gandhi J, Smith N, Khan SA. 2017; Anatomical approach to clinical problems of popliteal fossa. Curr Rheumatol Rev. 13:126–38. DOI: 10.2174/1573397112666161128102959. PMID: 27894238.
Article4. Landis JR, Koch GG. 1977; The measurement of observer agreement for categorical data. Biometrics. 33:159–74. DOI: 10.2307/2529310. PMID: 843571.
Article5. Chen H, Wu L. 2015; Surgical options for posterior tibial plateau fracture. Int J Clin Exp Med. 8:21421–7. PMID: 26885086. PMCID: PMC4723931.6. Thi C, Van Huy N, Nguyen NC, Thanh TH. 2018; Applied anatomy of common peroneal nerve: a cadaveric study. Int J Med Pharm. 6:6–10. DOI: 10.15640/ijmp.v6n1a2.
Article7. Hyland S, Sinkler MA, Varacallo M. 2020. Anatomy, bony pelvis and lower limb, popliteal region. StatPearls Publishing;Treasure Island:8. Kim TK, Savino RM, McFarland EG, Cosgarea AJ. 2002; Neurovascular complications of knee arthroscopy. Am J Sports Med. 30:619–29. DOI: 10.1177/03635465020300042501. PMID: 12130419.
Article9. Sora MC, Dresenkamp J, Gabriel A, Matusz P, Wengert GJ, Bartl R. 2015; The relationship of neurovascular structures to the posterior medial aspect of the knee: an anatomic study using plastinated cross-sections. Rom J Morphol Embryol. 56:1035–41. PMID: 26662136.10. Byun S, Gordon J, Morris S, Jacob T, Pather N. 2019; A computed tomography and magnetic resonance imaging study of the variations of the sciatic nerve branches of the pediatric knee: implications for peripheral nerve blockade. Clin Anat. 32:836–50. DOI: 10.1002/ca.23412. PMID: 31125132.
Article11. Aktan Ikiz ZA, Uçerler H, Bilge O. 2005; The anatomic features of the sural nerve with an emphasis on its clinical importance. Foot Ankle Int. 26:560–7. DOI: 10.1177/107110070502600712. PMID: 16045849.12. Paraskevas GK, Natsis K, Tzika M, Ioannidis O. 2014; Fascial entrapment of the sural nerve and its clinical relevance. Anat Cell Biol. 47:144–7. DOI: 10.5115/acb.2014.47.2.144. PMID: 24987554. PMCID: PMC4076424.
Article13. Nguyen AD, Boling MC, Levine B, Shultz SJ. 2009; Relationships between lower extremity alignment and the quadriceps angle. Clin J Sport Med. 19:201–6. DOI: 10.1097/JSM.0b013e3181a38fb1. PMID: 19423972. PMCID: PMC2881465.
Article14. Hafez MA, Sheikhedrees SM, Saweeres ES. 2016; Anthropometry of Arabian arthritic knees: comparison to other ethnic groups and implant dimensions. J Arthroplasty. 31:1109–16. DOI: 10.1016/j.arth.2015.11.017. PMID: 26791047.
Article15. Miyatake N, Sugita T, Aizawa T, Sasaki A, Maeda I, Kamimura M, Fujisawa H, Takahashi A. 2016; Comparison of intraoperative anthropometric measurements of the proximal tibia and tibial component in total knee arthroplasty. J Orthop Sci. 21:635–9. DOI: 10.1016/j.jos.2016.06.003. PMID: 27380729.
Article16. Ubelaker DH, DeGaglia CM. 2017; Population variation in skeletal sexual dimorphism. Forensic Sci Int. 278:407.e1–7. DOI: 10.1016/j.forsciint.2017.06.012. PMID: 28698063.
Article17. Hohmann E, Keough N, Glatt V, Tetsworth K, Putz R, Imhoff A. 2019; The mechanical properties of fresh versus fresh/frozen and preserved (thiel and formalin) long head of biceps tendons: a cadaveric investigation. Ann Anat. 221:186–91. DOI: 10.1016/j.aanat.2018.05.002. PMID: 29879483.
Article18. Eisma R, Lamb C, Soames RW. 2013; From formalin to thiel embalming: what changes? One anatomy department's experiences. Clin Anat. 26:564–71. DOI: 10.1002/ca.22222. PMID: 23408386.
Article19. Kennel L, Martin DMA, Shaw H, Wilkinson T. 2018; Learning anatomy through thiel- vs. formalin-embalmed cadavers: student perceptions of embalming methods and effect on functional anatomy knowledge. Anat Sci Educ. 11:166–74. DOI: 10.1002/ase.1715. PMID: 28719722.
Article