Persistent Anxiety Is Associated with Higher Glycemia Post-Transition to Adult Services in Asian Young Adults with Diabetes
- Affiliations
-
- 1Department of Endocrinology, Singapore General Hospital, Singapore.
- 2Academic Clinical Program, Division of Medicine, Singapore General Hospital, Singapore.
- KMID: 2514075
- DOI: http://doi.org/10.4093/dmj.2019.0226
Abstract
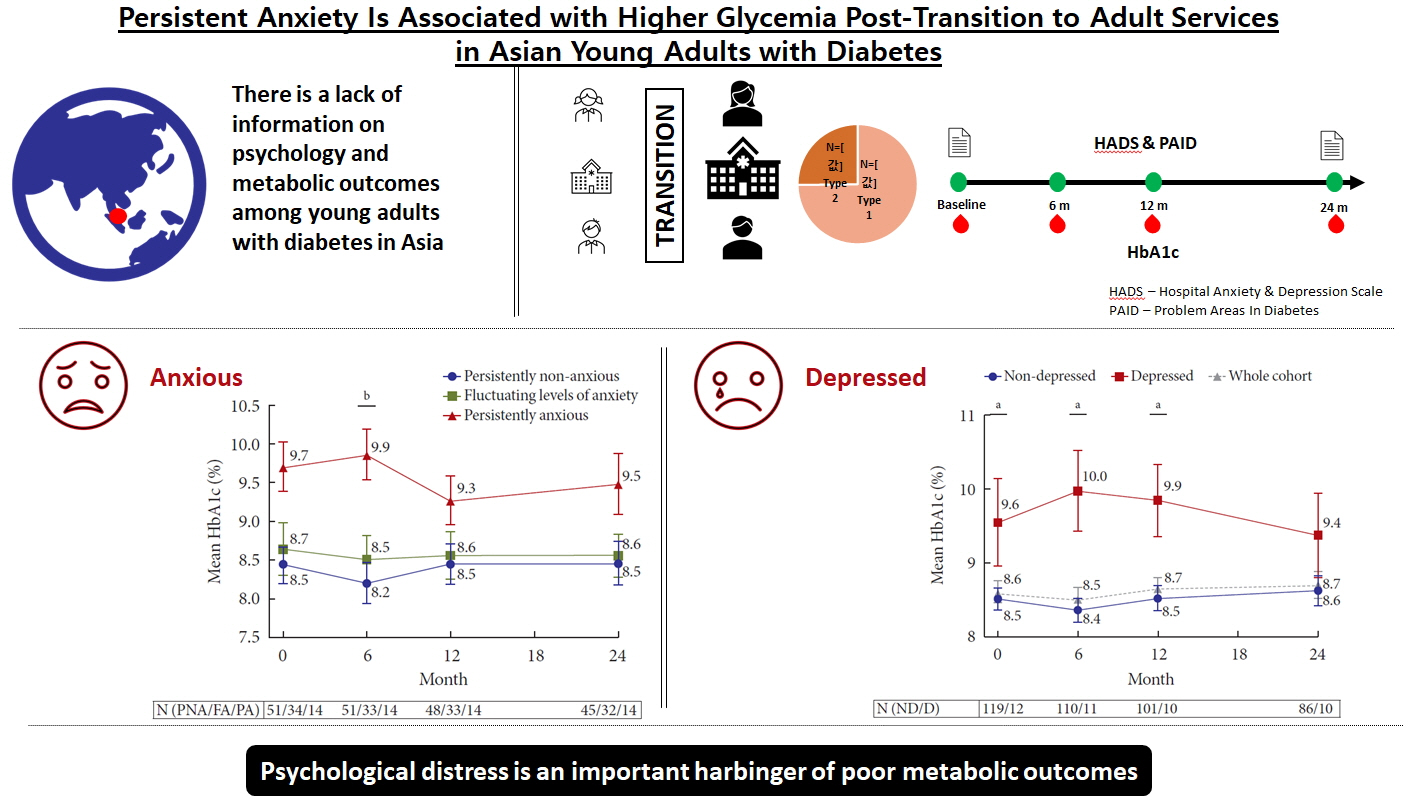
Background There is little longitudinal information on psychological burden and metabolic outcomes in young adults with diabetes (YAD) in Asia. We aimed to evaluate the association between psychological status and glycemia at baseline and 2 years following transition in a cohort of YAD in Singapore.
Methods Subjects with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), aged 17 to 25 years, were recruited from the YAD clinic in Singapore General Hospital. The Hospital Anxiety and Depression and Problem Areas for Diabetes scales were administered at transition (baseline) and at 18 to 24 months. Glycosylated hemoglobin (HbA1c) assessed during routine visits was tracked longitudinally.
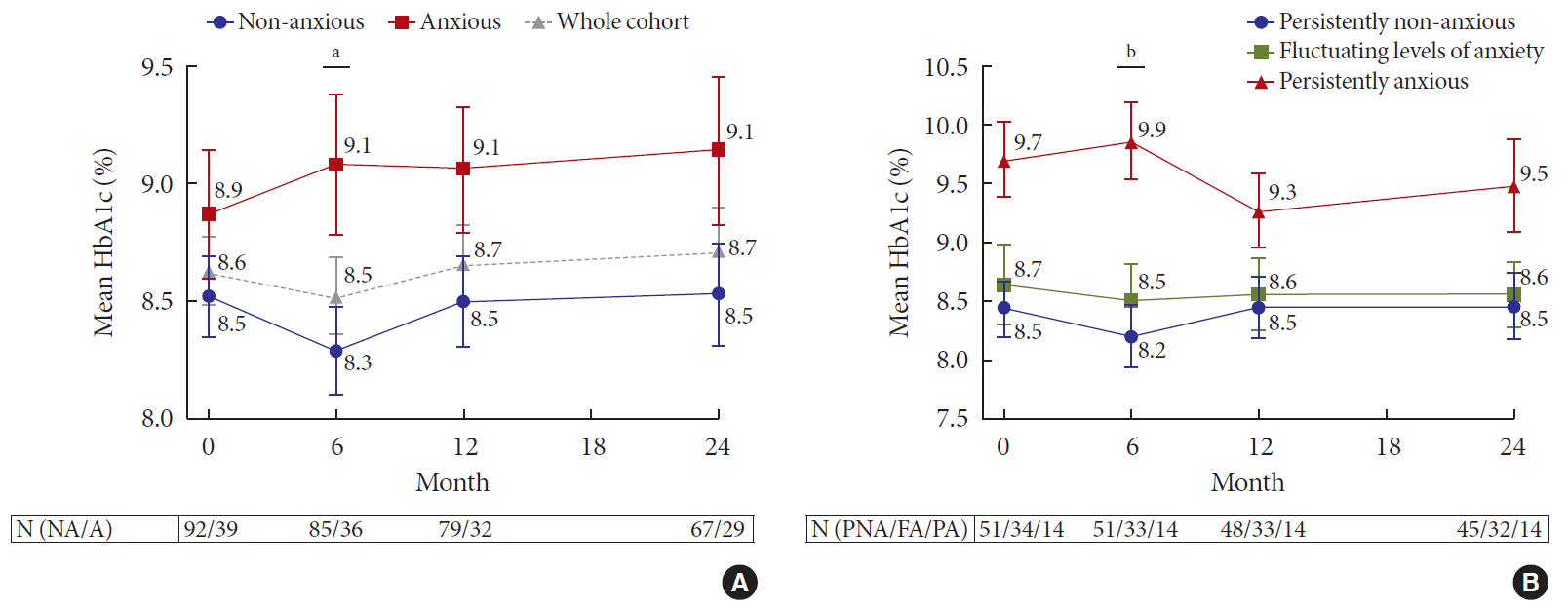
Results A total of 98 T1DM (74.8%) and 33 T2DM (25.2%) subjects were recruited between January 2011 and November 2017. At baseline, mean HbA1c was 8.6%±1.7%. Only 26.0% achieved HbA1c of ≤7.5% and 16.8% achieved HbA1c of <7%. At baseline, prevalence of anxiety was 29.8%. At 24 months, 14.1% had persistent anxiety. Those with persistent anxiety had the highest mean HbA1c, particularly at 6 months (persistently anxious vs. persistently non-anxious: 9.9%±1.2% vs. 8.2%±1.9%,
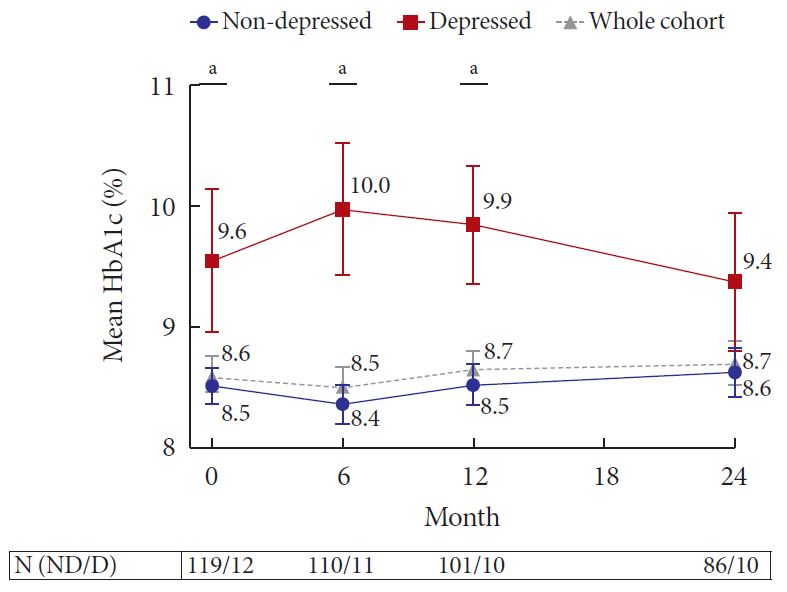
P =0.009). At baseline, 9.2% of subjects had depression. This group also had poorer glycemia at baseline (HbA1c of depressed vs non-depressed: 9.6%±2.1% vs. 8.5%±1.6%,P =0.04), which persisted up to 24 months.Conclusion The majority of YAD in Singapore have suboptimal glycemia. Psychological distress is a critical harbinger of poorer metabolic outcomes.
Figure
Reference
-
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016; 387:1513–1530.2. International Diabetes Federation. IDF diabetes atlas. 8th ed. Brussels: International Diabetes Federation;2017.3. Yeung RO, Zhang Y, Luk A, Yang W, Sobrepena L, Yoon KH, et al. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE programme): a cross-sectional study of a prospective cohort. Lancet Diabetes Endocrinol. 2014; 2:935–943.
Article4. Peters A, Laffel L. American Diabetes Association Transitions Working Group. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. A position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society). Diabetes Care. 2011; 34:2477–2485.5. Daneman D, Nakhla M. Moving on: transition of teens with type 1 diabetes to adult care. Diabetes Spectr. 2011; 24:14–18.
Article6. Adams JD, Hayes J, Hopson B. Transition: understanding and managing personal change. London: Martin Robertson;1976.7. Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, et al. T1D Exchange Clinic Network. Current state of type 1 diabetes treatment in the US: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015; 38:971–978.
Article8. McKnight JA, Wild SH, Lamb MJ, Cooper MN, Jones TW, Davis EA, et al. Glycaemic control of type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabet Med. 2015; 32:1036–1050.9. Petitti DB, Klingensmith GJ, Bell RA, Andrews JS, Dabelea D, Imperatore G, et al. SEARCH for Diabetes in Youth Study Group. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr. 2009; 155:668–672.
Article10. DiMeglio LA, Acerini CL, Codner E, Craig ME, Hofer SE, Pillay K, et al. ISPAD Clinical Practice Consensus Guidelines 2018: glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatr Diabetes. 2018; 19 Suppl 27:105–114.
Article11. American Diabetes Association. 13. Children and adolescents: standards of medical care in diabetes. 2019. Diabetes Care. 2019; 42 Suppl 1:S148–S164.12. Lewis K, Hermayer K. All grown up: moving from pediatric to adult diabetes care. Am J Med Sci. 2013; 345:278–283.
Article13. Bernstein CM, Stockwell MS, Gallagher MP, Rosenthal SL, Soren K. Mental health issues in adolescents and young adults with type 1 diabetes: prevalence and impact on glycemic control. Clin Pediatr (Phila). 2013; 52:10–15.14. Hislop AL, Fegan PG, Schlaeppi MJ, Duck M, Yeap BB. Prevalence and associations of psychological distress in young adults with type 1 diabetes. Diabet Med. 2008; 25:91–96.
Article15. Onda Y, Nishimura R, Morimoto A, Sano H, Utsunomiya K, Tajima N, et al. Diabetes Epidemiology Research International (DERI) Mortality Study Group. DERI) Mortality Study Group. Age at transition from pediatric to adult care has no relationship with mortality for childhood-onset type 1 diabetes in Japan: Diabetes Epidemiology Research International (DERI) Mortality Study. PLoS One. 2016; 11:e0150720.16. Ng WY, Lee YS, Todd AL, Lui KF, Loke KY, Thai AC. Tyrosine phosphatase-like protein (IA-2) and glutamic acid decarboxylase (GAD65) autoantibodies: a study of Chinese patients with diabetes mellitus. Autoimmunity. 2002; 35:119–124.
Article17. Ko GT, Chan JC, Yeung VT, Chow CC, Li JK, Lau MS, et al. Antibodies to glutamic acid decarboxylase in young Chinese diabetic patients. Ann Clin Biochem. 1998; 35(Pt 6):761–767.
Article18. The DCCT Research Group. Effects of age, duration and treatment of insulin-dependent diabetes mellitus on residual beta-cell function: observations during eligibility testing for the Diabetes Control and Complications Trial (DCCT). J Clin Endocrinol Metab. 1987; 65:30–36.19. DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ. 2002; 325:746.20. Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, et al. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014; 37:2864–2883.
Article21. National Glycohemoglobin Standardization Program: Certified methods and laboratories. cited 2020 May 20. Available from: http://www.ngsp.org/certified.asp.22. Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003; 1:29.23. Welch GW, Jacobson AM, Polonsky WH. The problem areas in diabetes scale. An evaluation of its clinical utility. Diabetes Care. 1997; 20:760–766.
Article24. Li C, Barker L, Ford ES, Zhang X, Strine TW, Mokdad AH. Diabetes and anxiety in US adults: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabet Med. 2008; 25:878–881.
Article25. Kampling H, Mittag O, Herpertz S, Baumeister H, Kulzer B, Petrak F. Can trajectories of glycemic control be predicted by depression, anxiety, or diabetes-related distress in a prospective cohort of adults with newly diagnosed type 1 diabetes? Results of a five-year follow-up from the German multicenter diabetes cohort study (GMDC-Study). Diabetes Res Clin Pract. 2018; 141:106–117.
Article26. Lee WR. The changing demography of diabetes mellitus in Singapore. Diabetes Res Clin Pract. 2000; 50 Suppl 2:S35–S39.
Article27. Jaacks LM, Liu W, Ji L, Mayer-Davis EJ. Type 1 diabetes stigma in China: a call to end the devaluation of individuals living with a manageable chronic disease. Diabetes Res Clin Pract. 2015; 107:306–307.
Article28. Browne JL, Ventura A, Mosely K, Speight J. ‘I’m not a druggie, I’m just a diabetic’: a qualitative study of stigma from the perspective of adults with type 1 diabetes. BMJ Open. 2014; 4:e005625.
Article29. Liu NF, Brown AS, Folias AE, Younge MF, Guzman SJ, Close KL, et al. Stigma in people with type 1 or type 2 diabetes. Clin Diabetes. 2017; 35:27–34.
Article30. Brazeau AS, Nakhla M, Wright M, Henderson M, Panagiotopoulos C, Pacaud D, et al. Stigma and its association with glycemic control and hypoglycemia in adolescents and young adults with type 1 diabetes: cross-sectional study. J Med Internet Res. 2018; 20:e151.
Article31. Rechenberg K, Whittemore R, Grey M. Anxiety in youth with type 1 diabetes. J Pediatr Nurs. 2017; 32:64–71.
Article32. Sivertsen B, Petrie KJ, Wilhelmsen-Langeland A, Hysing M. Mental health in adolescents with type 1 diabetes: results from a large population-based study. BMC Endocr Disord. 2014; 14:83.
Article33. Smith KJ, Deschenes SS, Schmitz N. Investigating the longitudinal association between diabetes and anxiety: a systematic review and meta-analysis. Diabet Med. 2018; 35:677–693.
Article34. Ali GC, Ryan G, De Silva MJ. Validated screening tools for common mental disorders in low and middle income countries: a systematic review. PLoS One. 2016; 11:e0156939.
Article35. Reddy P, Philpot B, Ford D, Dunbar JA. Identification of depression in diabetes: the efficacy of PHQ-9 and HADS-D. Br J Gen Pract. 2010; 60:e239–e245.
Article36. Zhang Y, Ting RZ, Yang W, Jia W, Li W, Ji L, et al. China Depression in Chinese Patients with Type 2 Diabetes (DD2) Study Group. Depression in Chinese patients with type 2 diabetes: associations with hyperglycemia, hypoglycemia, and poor treatment adherence. J Diabetes. 2015; 7:800–808.37. Kleinman A. Culture and depression. N Engl J Med. 2004; 351:951–953.
Article38. Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000; 23:934–942.
Article39. Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008; 31:2383–2390.
Article40. de Wit M, Delemarre-van de Waal HA, Bokma JA, Haasnoot K, Houdijk MC, Gemke RJ, et al. Follow-up results on monitoring and discussing health-related quality of life in adolescent diabetes care: benefits do not sustain in routine practice. Pediatr Diabetes. 2010; 11:175–181.
Article41. Fisher E, Lazar L, Shalitin S, Yackobovitch-Gavan M, de Vries L, Oron T, et al. Association between glycemic control and clinic attendance in emerging adults with type 1 diabetes: a tertiary center experience. J Diabetes Res. 2018; 2018:9572817.
Article42. Shulman R, Luo J, Shah BR. Mental health visits and low socio-economic status in adolescence are associated with complications of type 1 diabetes in early adulthood: a population-based cohort study. Diabet Med. 2018; 35:920–928.
Article43. Semenkovich K, Patel PP, Pollock AB, Beach KA, Nelson S, Masterson JJ, et al. Academic abilities and glycaemic control in children and young people with type 1 diabetes mellitus. Diabet Med. 2016; 33:668–673.
Article44. Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016; 39:2126–2140.45. Nip ASY, Reboussin BA, Dabelea D, Bellatorre A, Mayer-Davis EJ, Kahkoska AR, et al. SEARCH for Diabetes in Youth Study Group. Disordered eating behaviors in youth and young adults with type 1 or type 2 diabetes receiving insulin therapy: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2019; 42:859–866.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diabetes in Adolescence, Appropriate Transition to Adult Clinic
- A national survey of transition from pediatric to adult healthcare providers for adolescents and young adults with type 1 diabetes: perspectives of pediatric endocrinologists in Korea
- A Young Adult’s Life with Diabetes Based on a Social Ecological Model
- The mediating effects of post-pandemic health promotion behaviors in the relationship between anxiety and quality of life in young adults in South Korea: a cross-sectional study
- Understanding and Approaching Low Motivation in Young Adults with Diabetes Mellitus