J Korean Med Sci.
2021 Mar;36(11):e77. 10.3346/jkms.2021.36.e77.
Effect of Transport Time on the Use of Reperfusion Therapy for Patients with Acute Ischemic Stroke in Korea
- Affiliations
-
- 1Department of Neurology, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- 2Institute of Medical Science, Jeju National University, Jeju, Korea
- 3Department of Neurology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 4Department of Neurology, Eulji University Hospital, Daejeon, Korea
- 5Department of Neurology, Eulji General Hospital, Eulji University, Seoul, Korea
- 6Department of Neurology, Seoul Medical Center, Seoul, Korea
- 7Department of Neurology, Ilsan Paik Hospital, Inje University, Goyang, Korea
- 8Department of Neurology, Soonchunhyang University College of Medicine, Seoul, Korea
- 9Department of Neurology, Yeungnam University Hospital, Daegu, Korea
- 10Department of Neurology, Dongguk University Ilsan Hospital, Goyang, Korea
- 11Department of Neurology, Dong-A University College of Medicine, Busan, Korea
- 12Department of Neurology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 13Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Korea
- 14Clinical Research Center, Asan Medical Center, Seoul, Korea
- 15Department of Neurology, University of California San Francisco, San Francisco, CA, USA
- KMID: 2514053
- DOI: http://doi.org/10.3346/jkms.2021.36.e77
Abstract
- Background
We investigated the association between geographic proximity to hospitals and the administration rate of reperfusion therapy for acute ischemic stroke.
Methods
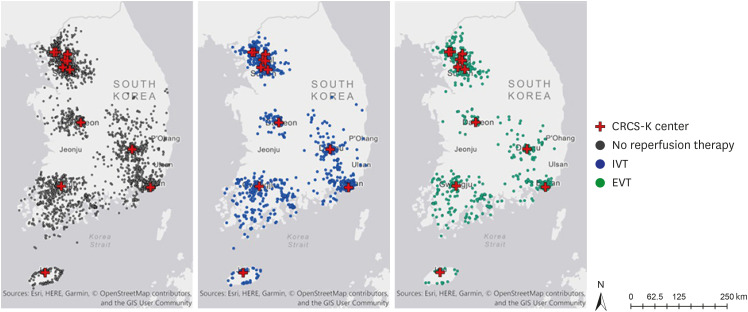
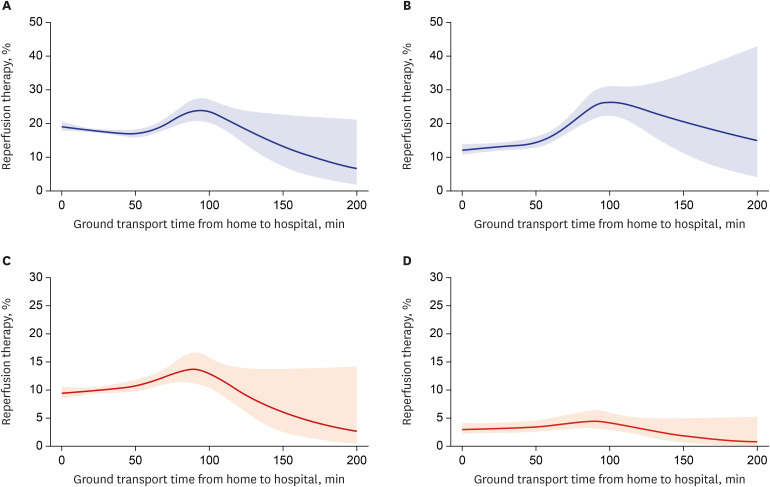
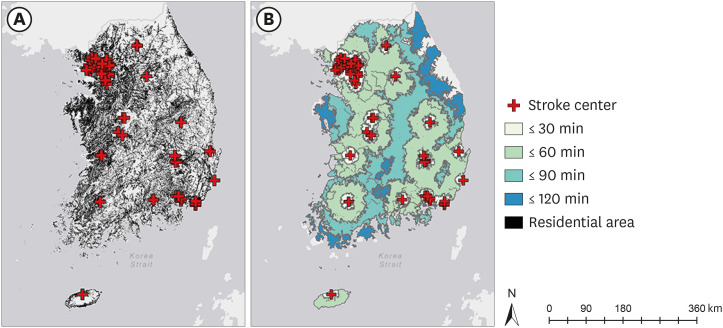
We identified patients with acute ischemic stroke who visited the hospital within 12 hours of symptom onset from a prospective nationwide multicenter stroke registry. Reperfusion therapy was classified as intravenous thrombolysis (IVT), endovascular therapy (EVT), or combined therapy. The association between the proportion of patients who were treated with reperfusion therapy and the ground transport time was evaluated using a spline regression analysis adjusted for patient-level characteristics. We also estimated the proportion of Korean population that lived within each 30-minute incremental service area from 67 stroke centers accredited by the Korean Stroke Society.
Results
Of 12,172 patients (mean age, 68 ± 13 years; men, 59.7%) who met the eligibility criteria, 96.5% lived within 90 minutes of ground transport time from the admitting hospital. The proportion of patients treated with IVT decreased significantly when stroke patients lived beyond 90 minutes of the transport time (P = 0.006). The proportion treated with EVT also showed a similar trend with the transport time. Based on the residential area, 98.4% of Korean population was accessible to 67 stroke centers within 90 minutes.
Conclusion
The use of reperfusion therapy for acute stroke decreased when patients lived beyond 90 minutes of the ground transport time from the hospital. More than 95% of the South Korean population was accessible to 67 stroke centers within 90 minutes of the ground transport time.
Figure
Cited by 1 articles
-
Annual Case Volume and One-Year Mortality for Endovascular Treatment in Acute Ischemic Stroke
Jun Yup Kim, Jihoon Kang, Beom Joon Kim, Seong-Eun Kim, Do Yeon Kim, Keon-Joo Lee, Hong-Kyun Park, Yong-Jin Cho, Jong-Moo Park, Kyung Bok Lee, Jae-Kwan Cha, Ji Sung Lee, Juneyoung Lee, Ki Hwa Yang, Ock Ran Hong, Ji Hyeon Shin, Jung Hyun Park, Philip B. Gorelick, Hee-Joon Bae
J Korean Med Sci. 2022;37(36):e270. doi: 10.3346/jkms.2022.37.e270.
Reference
-
1. Jansen JO, Morrison JJ, Wang H, He S, Lawrenson R, Hutchison JD, et al. Access to specialist care: optimizing the geographic configuration of trauma systems. J Trauma Acute Care Surg. 2015; 79(5):756–765. PMID: 26335775.2. Di Domenicantonio R, Cappai G, Sciattella P, Belleudi V, Di Martino M, Agabiti N, et al. The tradeoff between travel time from home to hospital and door to balloon time in determining mortality among STEMI patients undergoing PCI. PLoS One. 2016; 11(6):e0158336. PMID: 27336859.
Article3. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004; 109(10):1223–1225. PMID: 15007008.4. Harmsen AM, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: a systematic review. Injury. 2015; 46(4):602–609. PMID: 25627482.
Article5. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316(12):1279–1288. PMID: 27673305.
Article6. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384(9958):1929–1935. PMID: 25106063.
Article7. Choi JC, Hsia RY, Kim AS. Regional availability of mechanical embolectomy for acute ischemic stroke in California, 2009 to 2010. Stroke. 2015; 46(3):762–768. PMID: 25657180.
Article8. Acharya AB, Nyirenda JC, Higgs GB, Bloomfield MS, Cruz-Flores S, Connor LT, et al. Distance from home to hospital and thrombolytic utilization for acute ischemic stroke. J Stroke Cerebrovasc Dis. 2011; 20(4):295–301. PMID: 20634096.
Article9. Kunisawa S, Morishima T, Ukawa N, Ikai H, Otsubo T, Ishikawa KB, et al. Association of geographical factors with administration of tissue plasminogen activator for acute ischemic stroke. J Am Heart Assoc. 2013; 2(5):e000336. PMID: 24045119.
Article10. Ader J, Wu J, Fonarow GC, Smith EE, Shah S, Xian Y, et al. Hospital distance, socioeconomic status, and timely treatment of ischemic stroke. Neurology. 2019; 93(8):e747–57. PMID: 31320472.
Article11. Rosselló X, Huo Y, Pocock S, Van de Werf F, Chin CT, Danchin N, et al. Global geographical variations in ST-segment elevation myocardial infarction management and post-discharge mortality. Int J Cardiol. 2017; 245:27–34. PMID: 28750924.
Article12. Schwamm LH, Pancioli A, Acker JE 3rd, Goldstein LB, Zorowitz RD, Shephard TJ, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Stroke. 2005; 36(3):690–703. PMID: 15689577.13. Muñoz Venturelli P, Robinson T, Lavados PM, Olavarría VV, Arima H, Billot L, et al. Regional variation in acute stroke care organisation. J Neurol Sci. 2016; 371:126–130. PMID: 27871433.
Article14. Mullen MT, Branas CC, Kasner SE, Wolff C, Williams JC, Albright KC, et al. Optimization modeling to maximize population access to comprehensive stroke centers. Neurology. 2015; 84(12):1196–1205. PMID: 25740858.
Article15. The World Bank Data. Population density. Updated 2020. Accessed March 27, 2020. https://data.worldbank.org/indicator/EN.POP.DNST.16. Kim BJ, Han MK, Park TH, Park SS, Lee KB, Lee BC, et al. Current status of acute stroke management in Korea: a report on a multicenter, comprehensive acute stroke registry. Int J Stroke. 2014; 9(4):514–518. PMID: 24256115.
Article17. Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015; 17(1):38–53. PMID: 25692106.
Article18. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24(1):35–41. PMID: 7678184.
Article19. Ko Y, Lee S, Chung JW, Han MK, Park JM, Kang K, et al. MRI-based algorithm for acute ischemic stroke subtype classification. J Stroke. 2014; 16(3):161–172. PMID: 25328874.
Article20. Korean Statistical Information Service. Population of the administrative district. Updated 2019. Accessed March 1, 2020. http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040A3.21. Ma H, Campbell BC, Parsons MW, Churilov L, Levi CR, Hsu C, et al. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019; 380(19):1795–1803. PMID: 31067369.
Article22. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378(8):708–718. PMID: 29364767.
Article23. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378(1):11–21. PMID: 29129157.24. Paul CL, Ryan A, Rose S, Attia JR, Kerr E, Koller C, et al. How can we improve stroke thrombolysis rates? A review of health system factors and approaches associated with thrombolysis administration rates in acute stroke care. Implement Sci. 2016; 11(1):51. PMID: 27059183.
Article25. Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013–2014: National averages and disparities. J Korean Med Sci. 2020; 35(20):e167. PMID: 32449325.
Article26. Seo KD, Suh SH. Endovascular treatment in acute ischemic stroke: a nationwide survey in Korea. Neurointervention. 2018; 13(2):84–89. PMID: 30196678.
Article27. Kang J, Kim SE, Park HK, Cho YJ, Kim JY, Lee KJ, et al. Routing to endovascular treatment of ischemic stroke in Korea: recognition of need for process improvement. J Korean Med Sci. 2020; 35(41):e347. PMID: 33107228.
Article28. The World Bank Data. Urban population. Updated 2020. Accessed December 14, 2020. https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS?locations=KR.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reperfusion therapy in acute ischemic stroke
- Mobile Real-time Tracking of Acute Stroke Patients and Instant, Secure Inter-team Communication - the Join App
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis
- Diagnosis and Treatment of Acute Ischemic Stroke Guided by Stroke MRI