J Stroke.
2021 Jan;23(1):103-112. 10.5853/jos.2020.02404.
General Anesthesia versus Conscious Sedation in Mechanical Thrombectomy
- Affiliations
-
- 1Department of Neurology, Ludwig Maximilian University (LMU), Munich, Germany
- 2Department of Neurology & Stroke, Eberhard-Karls University of Tübingen, Tübingen, Germany
- 3Institute of Neuroradiology, Ludwig Maximilian University (LMU), Munich, Germany
- 4Department of Radiology, University Hospital Würzburg, Würzburg, Germany
- 5Institute for Stroke and Dementia Research, Ludwig Maximilian University (LMU), Munich, Germany
- 6Department of Anesthesiology, Ludwig Maximilian University (LMU), Munich, Germany
- 7The Institute for Medical Information Biometry and Epidemiology (IBE), Ludwig Maximilian University (LMU), Munich, Germany
- 8Munich Cluster for Systems Neurology (SyNergy), Munich, Germany
- 9German Center for Vertigo and Balance Disorders, Ludwig Maximilian University (LMU), Munich, Germany
- KMID: 2512359
- DOI: http://doi.org/10.5853/jos.2020.02404
Abstract
- Background and Purpose
Anesthesia regimen in patients undergoing mechanical thrombectomy (MT) is still an unresolved issue.
Methods
We compared the effect of anesthesia regimen using data from the German Stroke Registry-Endovascular Treatment (GSR-ET) between June 2015 and December 2019. Degree of disability was rated by the modified Rankin Scale (mRS), and good outcome was defined as mRS 0–2. Successful reperfusion was assumed when the modified thrombolysis in cerebral infarction scale was 2b–3.
Results
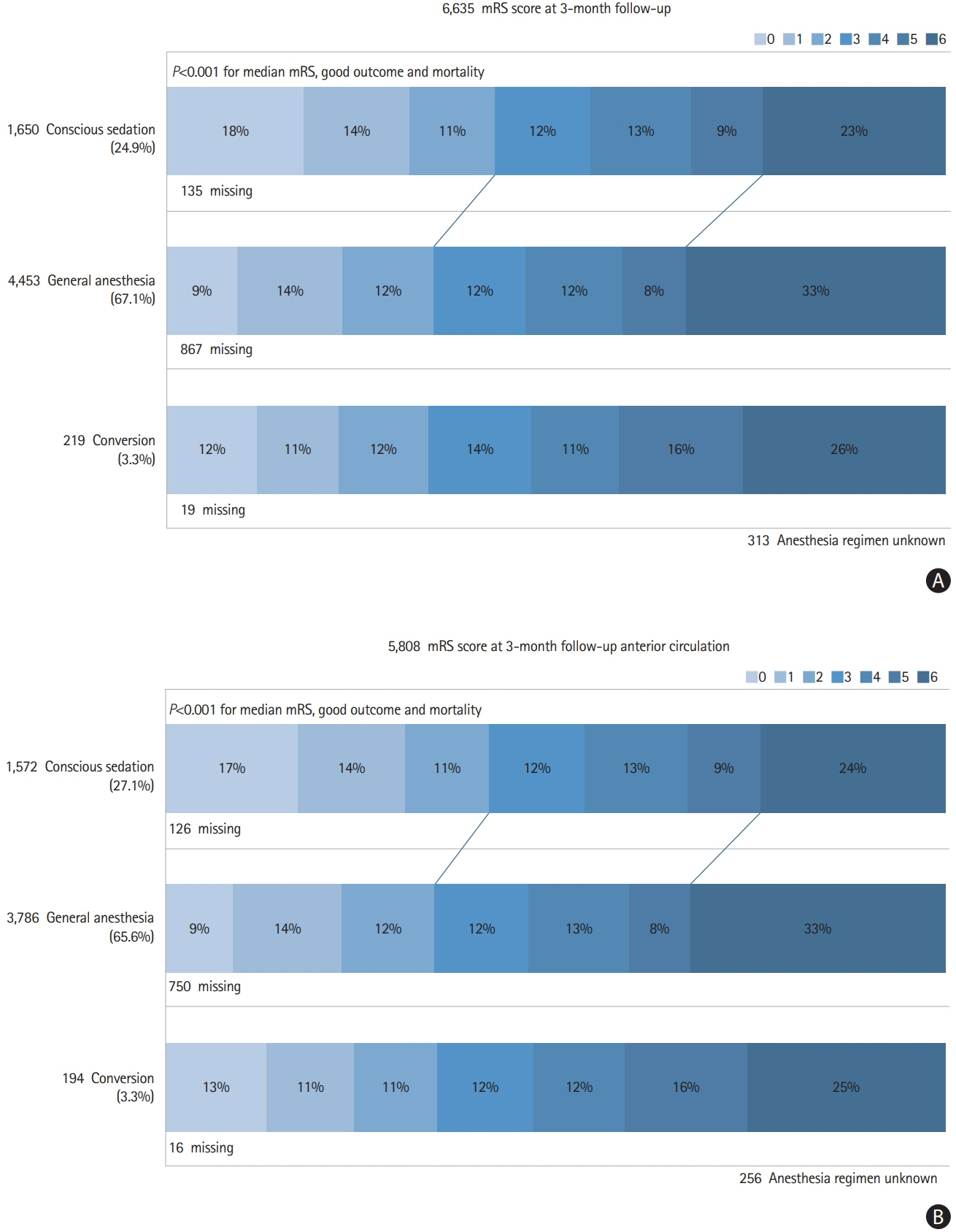
Out of 6,635 patients, 67.1% (n=4,453) patients underwent general anesthesia (GA), 24.9% (n=1,650) conscious sedation (CS), and 3.3% (n=219) conversion from CS to GA. Rate of successful reperfusion was similar across all three groups (83.0% vs. 84.2% vs. 82.6%, P=0.149). Compared to the CA-group, the GA-group had a delay from admission to groin (71.0 minutes vs. 61.0 minutes, P<0.001), but a comparable interval from groin to flow restoration (41.0 minutes vs. 39.0 minutes). The CS-group had the lowest rate of periprocedural complications (15.0% vs. 21.0% vs. 28.3%, P<0.001). The CS-group was more likely to have a good outcome at follow-up (42.1% vs. 34.2% vs. 33.5%, P<0.001) and a lower mortality rate (23.4% vs. 34.2% vs. 26.0%, P<0.001). In multivariable analysis, GA was associated with reduced achievement of good functional outcome (odds ratio [OR], 0.82; 95% confidence interval [CI], 0.71 to 0.94; P=0.004) and increased mortality (OR, 1.42; 95% CI, 1.23 to 1.64; P<0.001). Subgroup analysis for anterior circulation strokes (n=5,808) showed comparable results.
Conclusions
We provide further evidence that CS during MT has advantages over GA in terms of complications, time intervals, and functional outcome.
Figure
Reference
-
References
1. Schönenberger S, Hendén PL, Simonsen CZ, Uhlmann L, Klose C, Pfaff JAR, et al. Association of general anesthesia vs procedural sedation with functional outcome among patients with acute ischemic stroke undergoing thrombectomy: a systematic review and meta-analysis. JAMA. 2019; 322:1283–1293.2. Campbell BCV, van Zwam WH, Goyal M, Menon BK, Dippel DWJ, Demchuk AM, et al. Effect of general anaesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient data. Lancet Neurol. 2018; 17:47–53.3. Cappellari M, Pracucci G, Forlivesi S, Saia V, Nappini S, Nencini P, et al. General anesthesia versus conscious sedation and local anesthesia during thrombectomy for acute ischemic stroke. Stroke. 2020; 51:2036–2044.
Article4. Wollenweber FA, Tiedt S, Alegiani A, Alber B, Bangard C, Berrouschot J, et al. Functional outcome following stroke thrombectomy in clinical practice. Stroke. 2019; 50:2500–2506.
Article5. Alegiani AC, Dorn F, Herzberg M, Wollenweber FA, Kellert L, Siebert E, et al. Systematic evaluation of stroke thrombectomy in clinical practice: the German stroke registry endovascular treatment. Int J Stroke. 2019; 14:372–380.6. Ringleb PA, Hamann GF, Röther J, Jansen O, Groden C, Veltkamp R. Akuttherapie des ischämischen schlaganfalls: rekanalisierende therapie [Therapy of acute ischemic stroke: recanalisation therapy guideline]. Aktuelle Neurol. 2016; 43:82–91.7. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO)-European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019; 11:535–538.8. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.
Article9. Bekelis K, Missios S, MacKenzie TA, Tjoumakaris S, Jabbour P. Anesthesia technique and outcomes of mechanical thrombectomy in patients with acute ischemic stroke. Stroke. 2017; 48:361–366.
Article10. Powers CJ, Dornbos D 3rd, Mlynash M, Gulati D, Torbey M, Nimjee SM, et al. Thrombectomy with conscious sedation compared with general anesthesia: a DEFUSE 3 analysis. AJNR Am J Neuroradiol. 2019; 40:1001–1005.
Article11. Shan W, Yang D, Wang H, Xu L, Zhang M, Liu W, et al. General anesthesia may have similar outcomes with conscious sedation in thrombectomy patients with acute ischemic stroke: a real-world registry in China. Eur Neurol. 2018; 80:7–13.
Article12. Goldhoorn RB, Bernsen MLE, Hofmeijer J, Martens JM, Lingsma HF, Dippel DWJ, et al. Anesthetic management during endovascular treatment of acute ischemic stroke in the MR CLEAN Registry. Neurology. 2020; 94:e97–e106.
Article13. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.14. Flottmann F, Leischner H, Broocks G, Faizy TD, Aigner A, Deb-Chatterji M, et al. Emergency conversion to general anesthesia is a tolerable risk in patients undergoing mechanical thrombectomy. AJNR Am J Neuroradiol. 2020; 41:122–127.
Article15. Ren C, Xu G, Liu Y, Liu G, Wang J, Gao J. Effect of conscious sedation vs. general anesthesia on outcomes in patients undergoing mechanical thrombectomy for acute ischemic stroke: a prospective randomized clinical trial. Front Neurol. 2020; 11:170.
Article16. Schönenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S, Purrucker JC, et al. Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA. 2016; 316:1986–1996.17. Simonsen CZ, Sørensen LH, Juul N, Johnsen SP, Yoo AJ, Andersen G, et al. Anesthetic strategy during endovascular therapy: general anesthesia or conscious sedation? (GOLIATH - General or Local Anesthesia in Intra Arterial Therapy): a single-center randomized trial. Int J Stroke. 2016; 11:1045–1052.
Article18. Petersen NH, Ortega-Gutierrez S, Wang A, Lopez GV, Strander S, Kodali S, et al. Decreases in blood pressure during thrombectomy are associated with larger infarct volumes and worse functional outcome. Stroke. 2019; 50:1797–1804.
Article19. Mundiyanapurath S, Stehr A, Wolf M, Kieser M, Möhlenbruch M, Bendszus M, et al. Pulmonary and circulatory parameter guided anesthesia in patients with ischemic stroke undergoing endovascular recanalization. J Neurointerv Surg. 2016; 8:335–341.
Article20. Kety SS, Schmidt CF. The effects of altered arterial tensions of carbon dioxide and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Invest. 1948; 27:484–492.21. Brinjikji W, Murad MH, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF. Conscious sedation versus general anesthesia during endovascular acute ischemic stroke treatment: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015; 36:525–529.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthesia and Sedation
- A Retrospective Statistical Study on Sedation Cases in Department of Pediatric Dentistry at Dankook University Dental Hospital for 5 Years
- Titration of Effect Site Concentration of Propofol for Conscious Sedation in Elderly Patients
- Sedation at Sedation Clinic of Department of Dentistry in Hanyang University Medical Center (II)
- Trends of conscious sedation in the Department of Pediatric Dentistry at the Dankook University Dental Hospital for 11 Years