J Surg Ultrasound.
2020 Nov;7(2):29-35. 10.46268/jsu.2020.7.2.29.
Randomized Comparison of Thrombus Resolution Outcome between Direct Xa Inhibitor Anticoagulant and Warfarin In Acute Deep Vein Thrombosis
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Daegu Catholic University School of Medicine, Daegu, Korea
- KMID: 2511914
- DOI: http://doi.org/10.46268/jsu.2020.7.2.29
Abstract
- Purpose
Newly developed factor Xa inhibitor anticoagulants (Xaban) produced non-inferior outcomes in terms of venous thromboembolism (VTE) recurrence and safety. On the other hand, thrombus resolution (TR), a factor associated with VTE recurrence and post-thrombotic syndrome, was not expressed clearly in these studies. This study compared the long-term TR outcomes in patients treated with Xaban or warfarin.
Methods
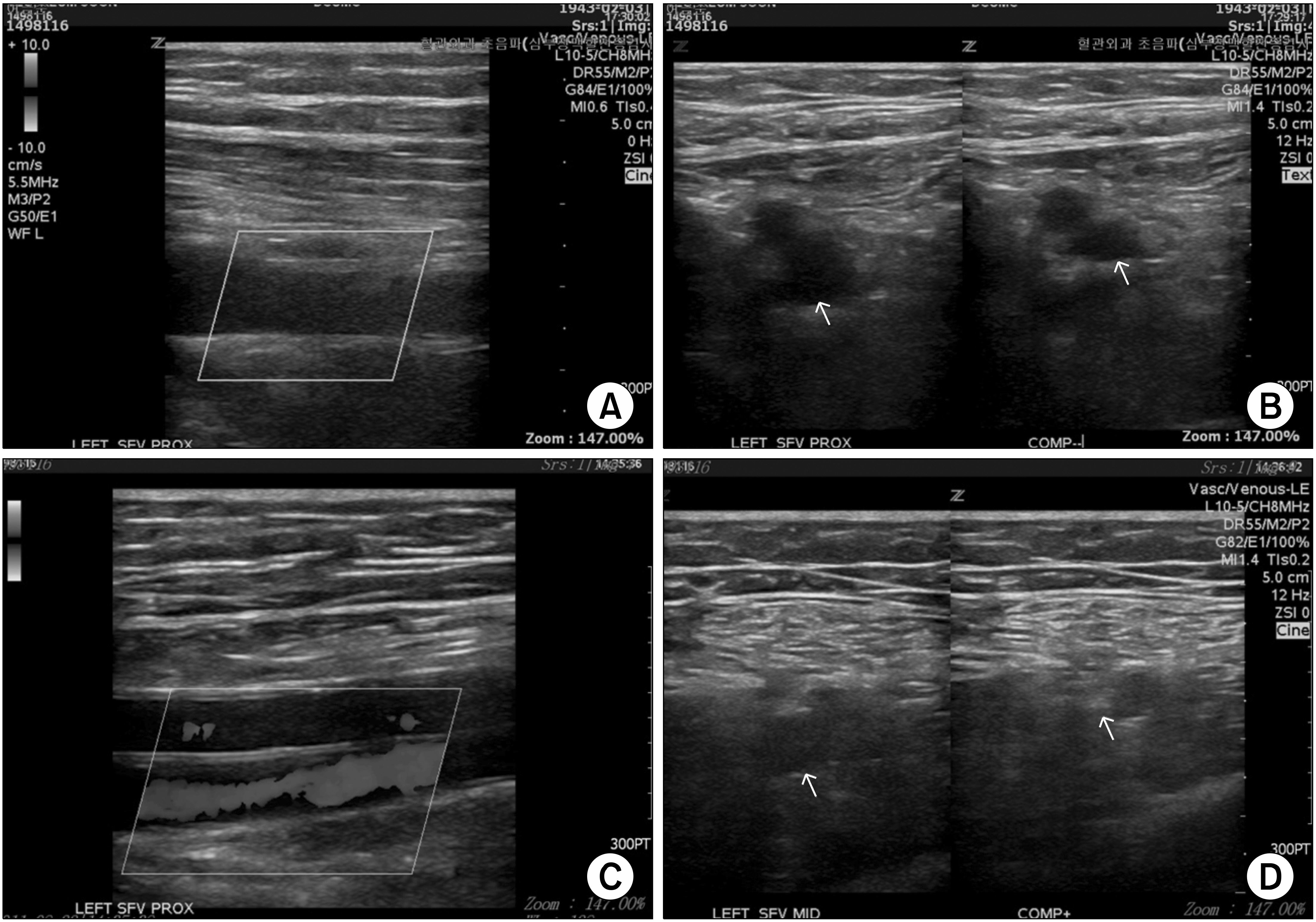
Fifty-seven acute deep vein thrombosis (DVT) patients were enrolled. After the initial heparin therapy, randomly assigned patients received oral Xaban or warfarin. The time in the therapeutic range was maintained at more than 60% during the anticoagulation period. After 3–12 months on the medication, a duplex scan was performed to diagnose the thrombus changes.
Results
Unprovoked DVT occurred in 80.7% of patients (46/57), and the mean age was 60.1 ± 13.99 years; 26 patients were female. Concurrent pulmonary embolism was diagnosed in 20 patients (52.6%) in the Xaban group and 10 (52.6%) in the warfarin group. The complete TR rate for the proximal venous segment was 47.4% (18/38) for the Xaban group and 57.9% (11/19) for the warfarin group. Complete DVT TR was observed in 26.3% of patients (10/38) in the Xaban group and 42.1% (8/19) in the warfarin group. No significant difference was observed between the proximal (P = 0.657) and complete TR rates (P = 0.227) between the two groups.
Conclusion
Xaban administration for acute DVT showed no difference in TR compared to warfarin. Xaban could also be an easy-to-use anticoagulation treatment option because it does not require monitoring and has a short half-life.
Keyword
Figure
Reference
-
1. Prandoni P, Noventa F, Ghirarduzzi A, Pengo V, Bernardi E, Pesavento R, et al. 2007; The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 92:199–205. DOI: 10.3324/haematol.10516. PMID: 17296569.
Article2. Iorio A, Kearon C, Filippucci E, Marcucci M, Macura A, Pengo V, et al. 2010; Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 170:1710–6. DOI: 10.1001/archinternmed.2010.367. PMID: 20975016.3. Prandoni P, Lensing AW, Prins MH, Bernardi E, Marchiori A, Bagatella P, et al. 2002; Residual venous thrombosis as a predictive factor of recurrent venous thromboembolism. Ann Intern Med. 137:955–60. DOI: 10.7326/0003-4819-137-12-200212170-00008. PMID: 12484710.
Article4. Young L, Ockelford P, Milne D, Rolfe-Vyson V, Mckelvie S, Harper P. 2006; Post-treatment residual thrombus increases the risk of recurrent deep vein thrombosis and mortality. J Thromb Haemost. 4:1919–24. DOI: 10.1111/j.1538-7836.2006.02120.x. PMID: 16836658.
Article5. Kahn SR, Shrier I, Julian JA, Ducruet T, Arsenault L, Miron MJ, et al. 2008; Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 149:698–707. DOI: 10.7326/0003-4819-149-10-200811180-00004. PMID: 19017588.
Article6. Killewich LA, Bedford GR, Beach KW, Strandness DE Jr. 1989; Spontaneous lysis of deep venous thrombi: rate and outcome. J Vasc Surg. 9:89–97. DOI: 10.1016/0741-5214(89)90223-1. PMID: 2911146.
Article7. Murphy TP, Cronan JJ. 1990; Evolution of deep venous thrombosis: a prospective evaluation with US. Radiology. 543–8. DOI: 10.1148/radiology.177.2.2217798. PMID: 2217798.
Article8. Caprini JA, Arcelus JI, Reyna JJ, Motykie GD, Mohktee D, Zebala LP, et al. 1999; Deep vein thrombosis outcome and the level of oral anticoagulation therapy. J Vasc Surg. 30:805–11. DOI: 10.1016/S0741-5214(99)70004-2. PMID: 10550177.
Article9. Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, et al. 2013; Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 369:799–808. DOI: 10.1056/NEJMoa1302507. PMID: 23808982.
Article10. Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, et al. 2010; Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 363:2499–510. DOI: 10.1056/NEJMoa1007903. PMID: 21128814.
Article11. Büller HR, Décousus H, Grosso MA, Mercuri M, Middeldorp S, Prins MH, et al. 2013; Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 369:1406–15. DOI: 10.1056/NEJMoa1306638. PMID: 23991658.
Article12. Carrier M, Rodger MA, Wells PS, Righini M, LE Gal G. 2011; Residual vein obstruction to predict the risk of recurrent venous thromboembolism in patients with deep vein thrombosis: a systematic review and meta-analysis. J Thromb Haemost. 9:1119–25. DOI: 10.1111/j.1538-7836.2011.04254.x. PMID: 21382171.
Article13. Killewich LA, Macko RF, Cox K, Franklin DR, Benjamin ME, Lilly MP, et al. 1997; Regression of proximal deep venous thrombosis is associated with fibrinolytic enhancement. J Vasc Surg. 26:861–8. DOI: 10.1016/S0741-5214(97)70101-0. PMID: 9372826.
Article14. Siragusa S, Malato A, Anastasio R, Cigna V, Milio G, Amato C, et al. 2008; Residual vein thrombosis to establish duration of anticoagulation after a first episode of deep vein thrombosis: the Duration of Anticoagulation based on Compression UltraSonography (DACUS) study. Blood. 112:511–5. DOI: 10.1182/blood-2008-01-131656. PMID: 18497320.
Article15. Incampo F, Carrieri C, Galasso R, Scaraggi FA, Di Serio F, Woodhams B, et al. 2013; Effect of warfarin treatment on thrombin activatable fibrinolysis inhibitor (TAFI) activation and TAFI-mediated inhibition of fibrinolysis. J Thromb Haemost. 11:315–24. DOI: 10.1111/jth.12102. PMID: 23256818.
Article16. Brownson K, Satoskar S, Reynolds J, Sumpio B, Sarac T, Scoutt L, et al. 2016; Thrombus resolution as guide to anticoagulation therapy for provoked deep vein thrombosis: TRUDVT pilot study. J Vasc Surg Venous Lymphat Disord. 4:149. DOI: 10.1016/j.jvsv.2015.10.040.
Article17. Douketis JD, Crowther MA, Foster GA, Ginsberg JS. 2001; Does the location of thrombosis determine the risk of disease recurrence in patients with proximal deep vein thrombosis? Am J Med. 110:515–9. DOI: 10.1016/S0002-9343(01)00661-1. PMID: 11343664.18. Macedo AF, Bell J, McCarron C, Conroy R, Richardson J, Scowcroft A, et al. 2015; Determinants of oral anticoagulation control in new warfarin patients: analysis using data from Clinical Practice Research Datalink. Thromb Res. 136:250–60. DOI: 10.1016/j.thromres.2015.06.007. PMID: 26073321.
Article19. Johnson BF, Manzo RA, Bergelin RO, Strandness DE Jr. 1995; Relationship between changes in the deep venous system and the development of the postthrombotic syndrome after an acute episode of lower limb deep vein thrombosis: a one- to six-year follow-up. J Vasc Surg. 21:307–12. discussion 313DOI: 10.1016/S0741-5214(95)70271-7. PMID: 7853603.
Article20. Ouriel K, Greenberg RK, Green RM, Massullo JM, Goines DR. 1999; A volumetric index for the quantification of deep venous thrombosis. J Vasc Surg. 30:1060–6. DOI: 10.1016/S0741-5214(99)70044-3. PMID: 10587390.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deep Vein Thrombosis and Neurovascular Injury after Total Hip Arthroplasty
- Portal Vein Thrombosis Associated with Antiphospholipid Syndrome
- Recent advances in the management of venous thromboembolism
- Recurrent acute portal vein thrombosis in liver cirrhosis treated by rivaroxaban
- Guidance for Endoscopic Procedures in Patients Taking Novel Oral Anticoagulants