Obstet Gynecol Sci.
2020 Nov;63(6):719-725. 10.5468/ogs.19075.
Correlation between obesity and pelvic organ prolapse in Korean women
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ymiz Woman Clinic, Anyang, Korea
- 2Department of Obstetrics and Gynecology, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- KMID: 2511212
- DOI: http://doi.org/10.5468/ogs.19075
Abstract
Objective
This study aimed to evaluate the correlation between obesity and pelvic organ prolapse (POP), both anatomically and symptomatically, in Korean women.
Methods
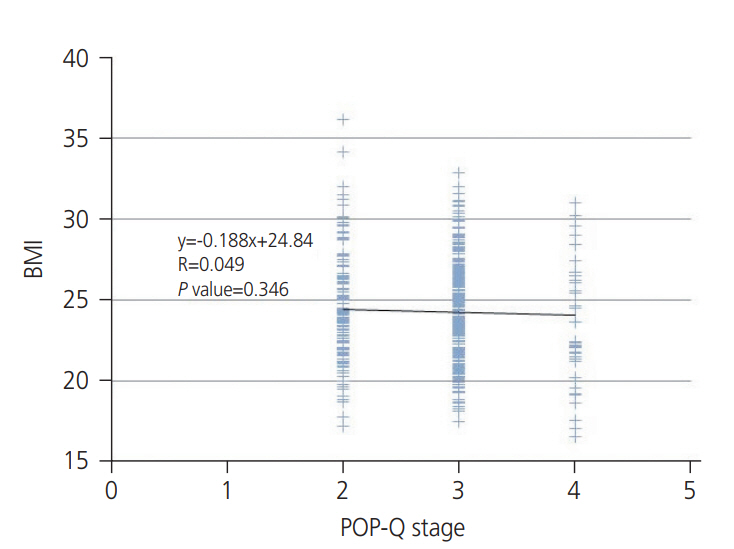
We retrospectively reviewed 476 women who visited the urogynecology clinic between January 2013 and December 2016. All the enrolled women were Korean. We sought to evaluate the relationship between obesity and POP, both anatomically and symptomatically, by using a validated tool. Anatomic assessment was performed by a standardized Pelvic Organ Prolapse Quantification (POP-Q) system and symptomatic assessment was performed by a Pelvic Floor Distress Inventory (PFDI)-20 questionnaire. Obesity measurement was performed by measuring body mass index (BMI).
Results
We enrolled 476 women in our study. There was no statistically significant correlation between BMI and POP-Q or PFDI-20 scores: Ba (P=0.633), Bp (P=0.363), C (P=0.277), Pelvic Organ Prolapse Distress Inventory-6 (P=0.286), Colorectal Anal Distress Inventory-8 (P=0.960), Urinary Distress Inventory-6 (P=0.355), and PFDI-20 (P=0.355). In addition, there was no statistically significant correlation between BMI and POP-Q or PFDI-20 in patients with severe (greater than stage III) POP. We also separately analyzed the differences in the POP-Q points and PFDI-20 scores between the obese and non-obese groups. There was no statistically significant difference between the groups.
Conclusion
We evaluated the correlation between obesity and POP using a validated tool. The present study revealed no significant correlation between obesity and POP severity anatomically or symptomatically in Korean women. This contrasts the results of most studies of Western women. Further studies in Asian women are required in order to confirm our results.
Keyword
Figure
Cited by 3 articles
-
Correlation between the expression of matrix metalloproteinase 9 and the expression of tissue inhibitor of metalloproteinase-1 of uterosacral ligament in uterine prolapse
Dhanny Primantara Johari Santoso, Benny Hasan Purwara, Eppy Darmadi Achmad
Obstet Gynecol Sci. 2022;65(1):46-51. doi: 10.5468/ogs.21156.Current techniques used to perform surgery for anterior and posterior vaginal wall prolapse in South Korea
Soo Rim Kim, Dong Hoon Suh, Woojeong Kim, Myung Jae Jeon
Obstet Gynecol Sci. 2022;65(3):273-278. doi: 10.5468/ogs.21352.How and on whom to perform uterine-preserving surgery for uterine prolapse
Sumin Oh, Myung Jae Jeon
Obstet Gynecol Sci. 2022;65(4):317-324. doi: 10.5468/ogs.22003.
Reference
-
References
1. Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2013; 24:1783–90.
Article2. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997; 89:501–6.
Article3. Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008; 300:1311–6.
Article4. Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol. 1997; 104:579–85.
Article5. Richter HE, Burgio KL, Clements RH, Goode PS, Redden DT, Varner RE. Urinary and anal incontinence in morbidly obese women considering weight loss surgery. Obstet Gynecol. 2005; 106:1272–7.
Article6. Erekson EA, Sung VW, Myers DL. Effect of body mass index on the risk of anal incontinence and defecatory dysfunction in women. Am J Obstet Gynecol. 2008; 198:596. e1-4.
Article7. Leeners B, Geary N, Tobler PN, Asarian L. Ovarian hormones and obesity. Hum Reprod Update. 2017; 23:300–21.
Article8. Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996; 175:10–7.
Article9. Yoo EH, Jeon MJ, Ahn KH, Bai SW. Translation and linguistic validation of Korean version of short form of pelvic floor distress inventory-20, pelvic floor impact questionnaire-7. Obstet Gynecol Sci. 2013; 56:330–2.
Article10. Yoon JL, Cho JJ, Park KM, Noh HM, Park YS. Diagnostic performance of body mass index using the Western Pacific Regional Office of World Health Organization reference standards for body fat percentage. J Korean Med Sci. 2015; 30:162–6.
Article11. Hunskaar S. A systematic review of overweight and obesity as risk factors and targets for clinical intervention for urinary incontinence in women. Neurourol Urodyn. 2008; 27:749–57.
Article12. Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002; 186:1160–6.
Article13. Shalom DF, Lin SN, St Louis S, Winkler HA. Effect of age, body mass index, and parity on Pelvic Organ Prolapse Quantification system measurements in women with symptomatic pelvic organ prolapse. J Obstet Gynaecol Res. 2012; 38:415–9.
Article14. Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017; 217:11–26. e3.
Article15. Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J Pelvic Floor Dysfunct. 2015; 26:1559–73.
Article16. Uustal Fornell E, Wingren G, Kjølhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004; 83:383–9.
Article17. Bradley CS, Zimmerman MB, Wang Q, Nygaard IE; Women’s Health Initiative. Vaginal descent and pelvic floor symptoms in postmenopausal women: a longitudinal study. Obstet Gynecol. 2008; 111:1148–53.18. Washington BB, Erekson EA, Kassis NC, Myers DL. The association between obesity and stage II or greater prolapse. Am J Obstet Gynecol. 2010; 202:503. e1-4.
Article19. Foley JT, Lloyd M, Temple VA. Body mass index trends among adult U.S. Special Olympians, 2005-2010. Adapt Phys Activ Q. 2013; 30:373–86.
Article20. Kim CM, Jeon MJ, Chung DJ, Kim SK, Kim JW, Bai SW. Risk factors for pelvic organ prolapse. Int J Gynaecol Obstet. 2007; 98:248–51.
Article21. Seo JT, Kim JM. Pelvic organ support and prevalence by Pelvic Organ Prolapse-Quantification (POP-Q) in Korean women. J Urol. 2006; 175:1769–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical treatments for vaginal apical prolapse
- The role of mesh and graft in pelvic reconstructive surgery
- Correlation between the posterior vaginal wall and apex in pelvic organ prolapse
- Diagnosis and treatment of Pelvic Organ Prolapse
- Surgical decision making for symptomatic pelvic organ prolapse: evidence-based approach