Obstet Gynecol Sci.
2016 Jul;59(4):253-260. 10.5468/ogs.2016.59.4.253.
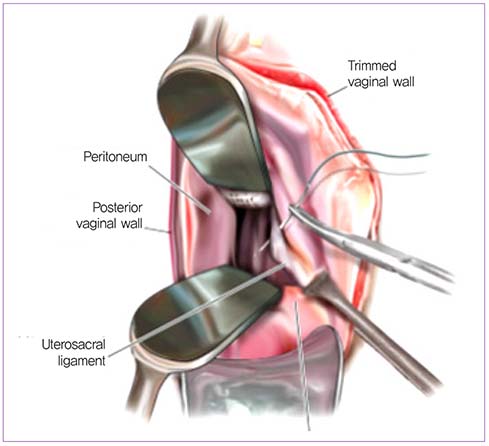
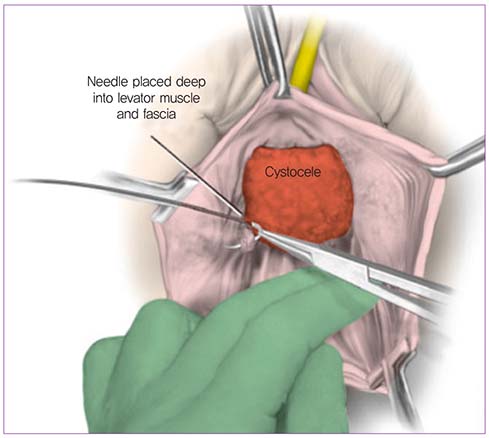
Surgical treatments for vaginal apical prolapse
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea. swbai@yuhs.ac
- KMID: 2329045
- DOI: http://doi.org/10.5468/ogs.2016.59.4.253
Abstract
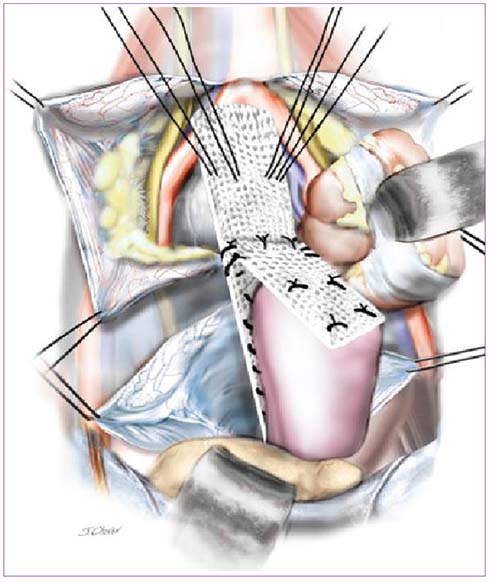
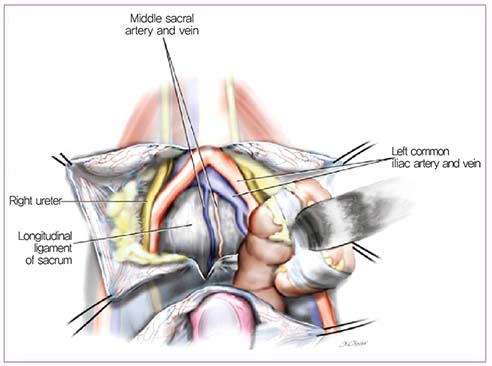
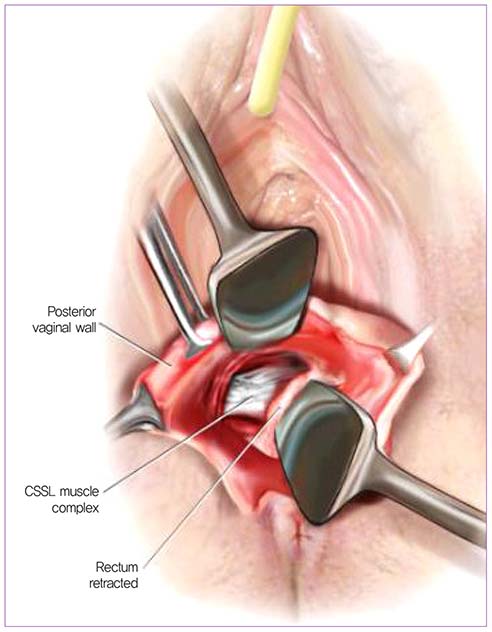
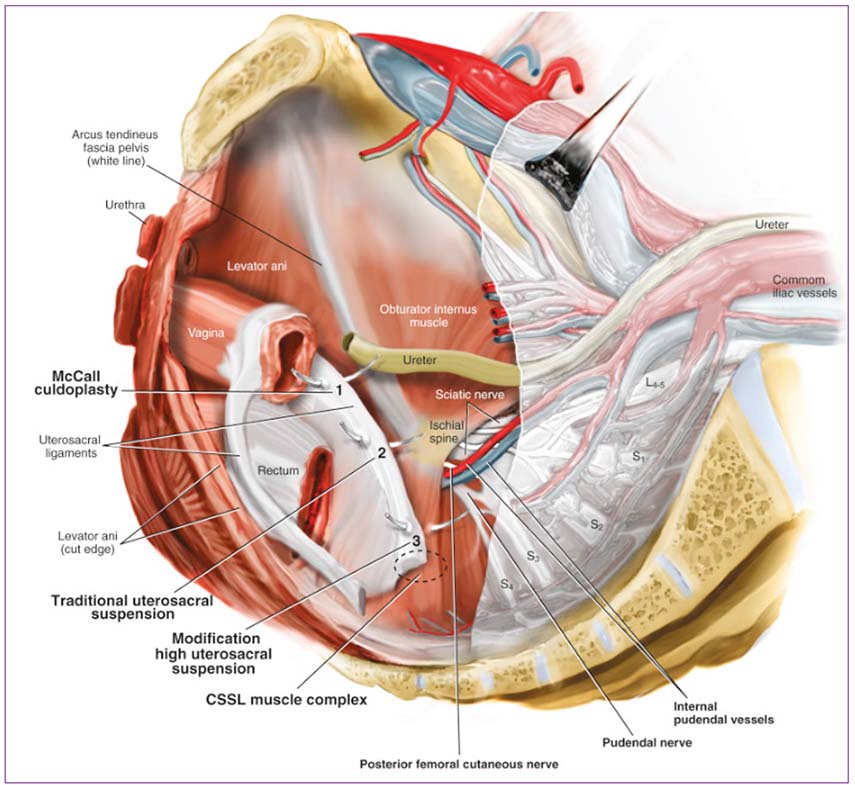
- Pelvic organ prolapse is a common condition, occurring in up to 11% of women in the United States. Often, pelvic organ prolapse recurs after surgery; when it recurs after hysterectomy, it frequently presents as vaginal apical prolapse. There are many different surgical treatments for vaginal apical prolapse; among them, abdominal sacral colpopexy is considered the gold standard. However, recent data reveal that other surgical procedures also result in good outcome. This review discusses the various surgical treatments for vaginal apical prolapse including their risks and benefits.
Figure
Reference
-
1. Machin SE, Mukhopadhyay S. Pelvic organ prolapse: review of the aetiology, presentation, diagnosis and management. Menopause Int. 2011; 17:132–136.2. Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979-1997. Am J Obstet Gynecol. 2003; 188:108–115.3. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997; 89:501–506.4. Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS. Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol. 2001; 98:646–651.5. Karram MM. Vaginal native tissue suture repair of vaginal vault prolapse. In : Baggish MS, Karram MM, editors. Atlas of pelvic anatomy and gynecologic surgery. 4th ed. Philadelphia (PA): Elsevier;2016. p. 647–677.6. Good MM, Abele TA, Balgobin S, Montoya TI, McIntire D, Corton MM. Vascular and ureteral anatomy relative to the midsacral promontory. Am J Obstet Gynecol. 2013; 208:486.e1–486.e7.7. Milani R, Cesana MC, Spelzini F, Sicuri M, Manodoro S, Fruscio R. Iliococcygeus fixation or abdominal sacral colpopexy for the treatment of vaginal vault prolapse: a retrospective cohort study. Int Urogynecol J. 2014; 25:279–284.8. Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013; 24:377–384.9. Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013; 24:1815–1833.10. McCall ML. Posterior culdeplasty: surgical correction of enterocele during vaginal hysterectomy: a preliminary report. Obstet Gynecol. 1957; 10:595–602.11. Webb MJ, Aronson MP, Ferguson LK, Lee RA. Posthysterectomy vaginal vault prolapse: primary repair in 693 patients. Obstet Gynecol. 1998; 92:281–285.12. Sederl J. Surgery in prolapse of a blind-end vagina. Geburtshilfe Frauenheilkd. 1958; 18:824–828.13. Morgan DM, Rogers MA, Huebner M, Wei JT, Delancey JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Obstet Gynecol. 2007; 109:1424–1433.14. Paraiso MF, Ballard LA, Walters MD, Lee JC, Mitchinson AR. Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol. 1996; 175:1423–1430.15. Unger CA, Walters MD. Gluteal and posterior thigh pain in the postoperative period and the need for intervention after sacrospinous ligament colpopexy. Female Pelvic Med Reconstr Surg. 2014; 20:208–211.16. Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol. 2004; 190:20–26.17. Margulies RU, Rogers MA, Morgan DM. Outcomes of transvaginal uterosacral ligament suspension: systematic review and metaanalysis. Am J Obstet Gynecol. 2010; 202:124–134.18. Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. JAMA. 2014; 311:1023–1034.19. Unger CA, Walters MD, Ridgeway B, Jelovsek JE, Barber MD, Paraiso MF. Incidence of adverse events after uterosacral colpopexy for uterovaginal and posthysterectomy vault prolapse. Am J Obstet Gynecol. 2015; 212:603.e1–603.e7.20. Inmon WB. Pelvic relaxation and repair including prolapse of vagina following hysterectomy. South Med J. 1963; 56:577–582.21. Shull BL, Capen CV, Riggs MW, Kuehl TJ. Bilateral attachment of the vaginal cuff to iliococcygeus fascia: an effective method of cuff suspension. Am J Obstet Gynecol. 1993; 168(6 Pt 1):1669–1674.22. Walters MD, Karram MM. Urogynecology and reconstructive pelvic surgery. 4th ed. Philadelphia (PA): Saunders;2014.23. Medina CA, Croce C, Candiotti K, Takacs P. Comparison of vaginal length after iliococcygeus fixation and sacrospinous ligament fixation. Int J Gynaecol Obstet. 2008; 100:267–270.24. Kokanali MK, Cavkaytar S, Aksakal O, Doganay M. McCall Culdoplasty vs. Sacrospinous Ligament Fixation after vaginal hysterectomy: comparison of postoperative vaginal length and sexual function in postmenopausal women. Eur J Obstet Gynecol Reprod Biol. 2015; 194:218–222.25. Serati M, Braga A, Bogani G, Leone Roberti, Sorice P, Ghezzi F, et al. Iliococcygeus fixation for the treatment of apical vaginal prolapse: efficacy and safety at 5 years of follow-up. Int Urogynecol J. 2015; 26:1007–1012.26. Sokol AI, Iglesia CB, Kudish BI, Gutman RE, Shveiky D, Bercik R, et al. One-year objective and functional outcomes of a randomized clinical trial of vaginal mesh for prolapse. Am J Obstet Gynecol. 2012; 206:86.e1–86.e9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Five cases of abdominal sacral colpopexy for the vaginal vault prolapse after total hysterectomy
- Correlation between the posterior vaginal wall and apex in pelvic organ prolapse
- Four Cases of Repair of Post Hysterectomy Vaginal Vault Prolapse
- Efficacy of Posterior IVS for the Patients with Vaginal Vault and Uterine Prolapse
- Prolapse of Fallopian Tube into Vaginal Vault after Hysterectomy: A case report