Obstet Gynecol Sci.
2020 Nov;63(6):709-718. 10.5468/ogs.20117.
Serum lactate dehydrogenase is a possible predictor of platinum resistance in ovarian cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, National Hospital Organization Kyoto Medical Center, Kyoto, Japan
- 2Department of Gynecology and Obstetrics, Kyoto University Graduate School of Medicine, Kyoto, Japan
- 3Department of Endocrinology, Metabolism, and Hypertension, Clinical Research Institute, National Hospital Organization Kyoto Medical Center, Kyoto, Japan
- KMID: 2511211
- DOI: http://doi.org/10.5468/ogs.20117
Abstract
Objective
The need for tailoring ovarian cancer treatments to individual patients is increasing. This study aimed to evaluate the prognostic value of pretreatment laboratory test data for predicting the response and survival outcomes of platinumbased chemotherapy in ovarian cancer.
Methods
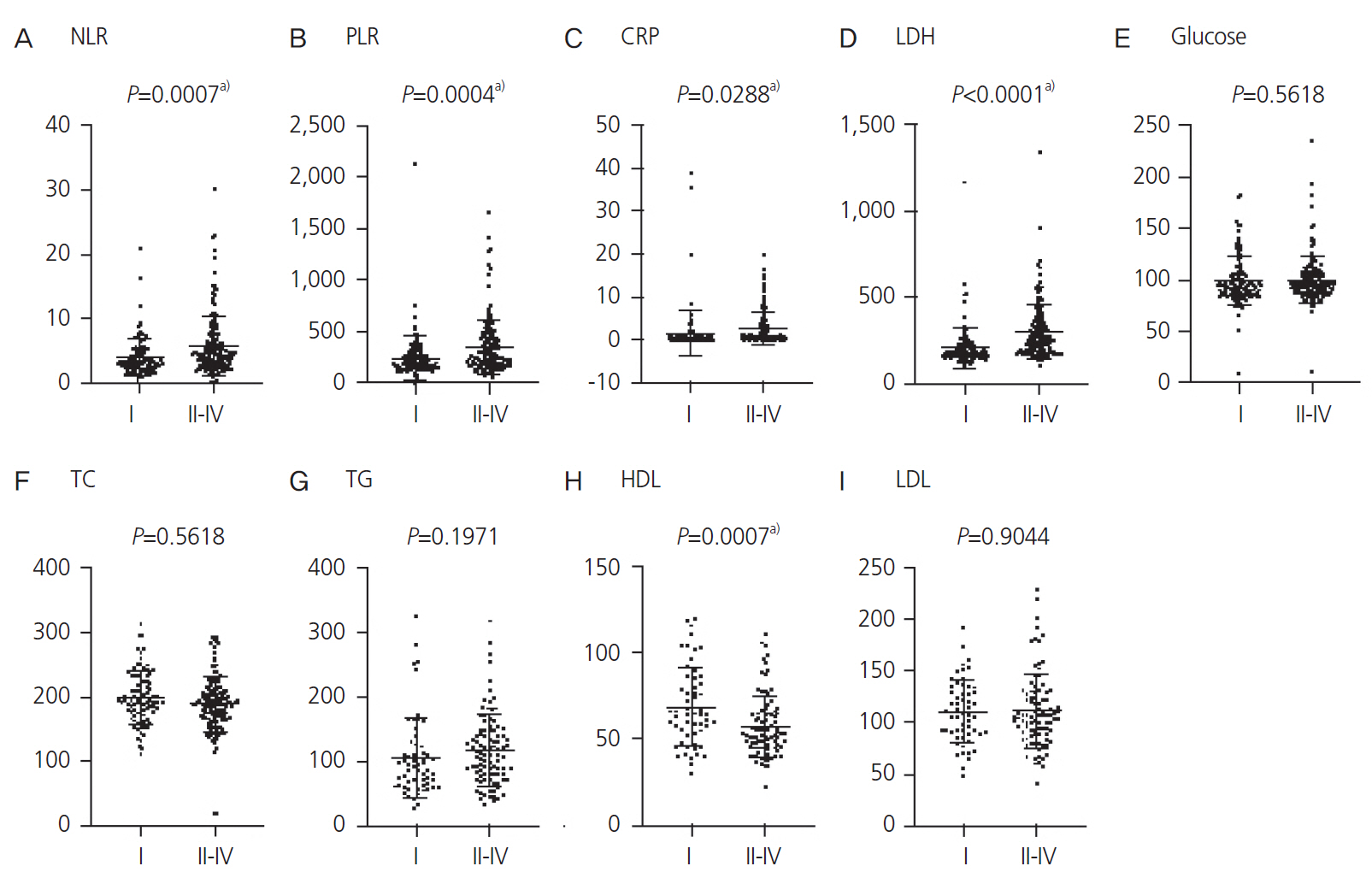
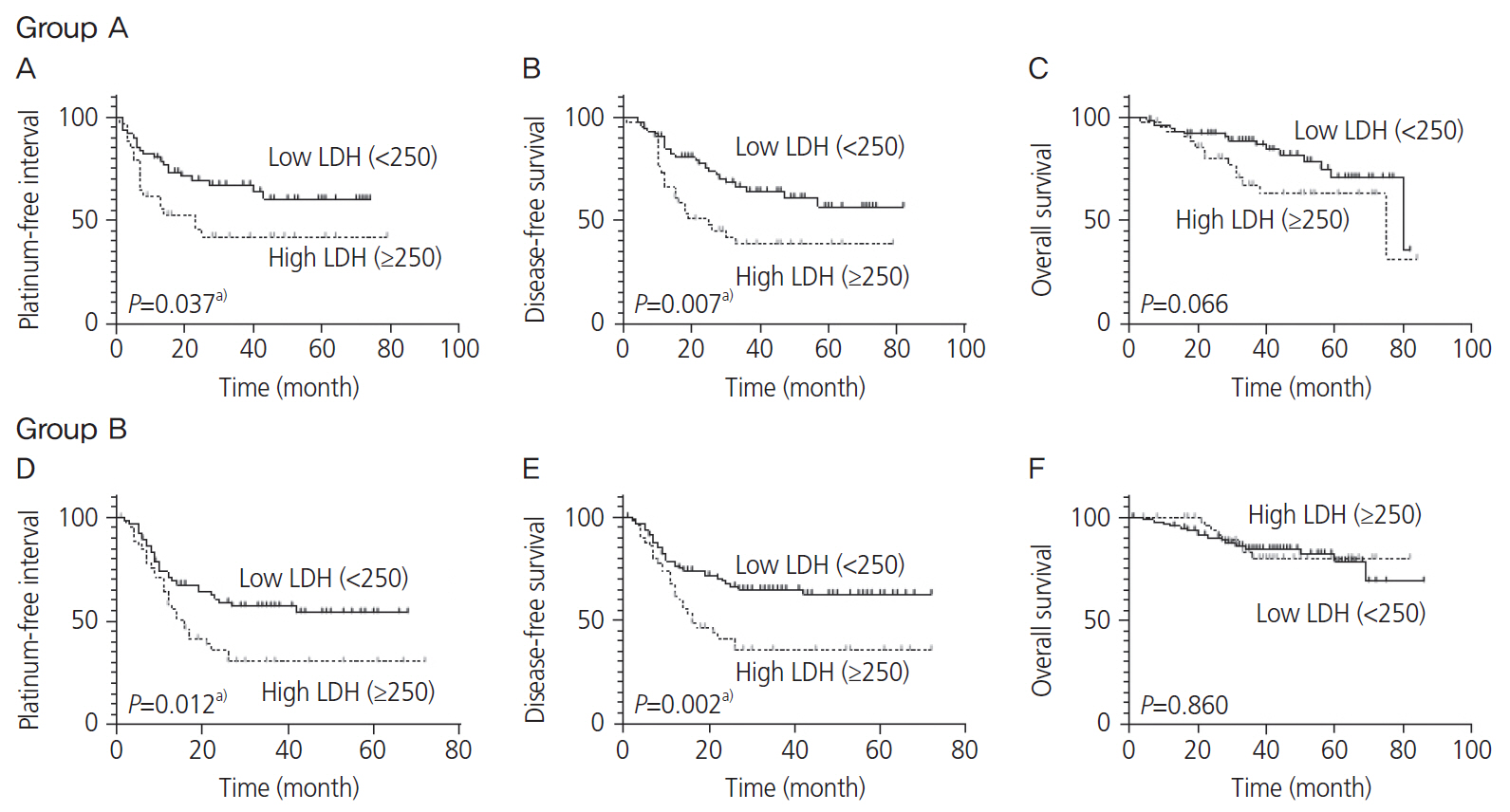
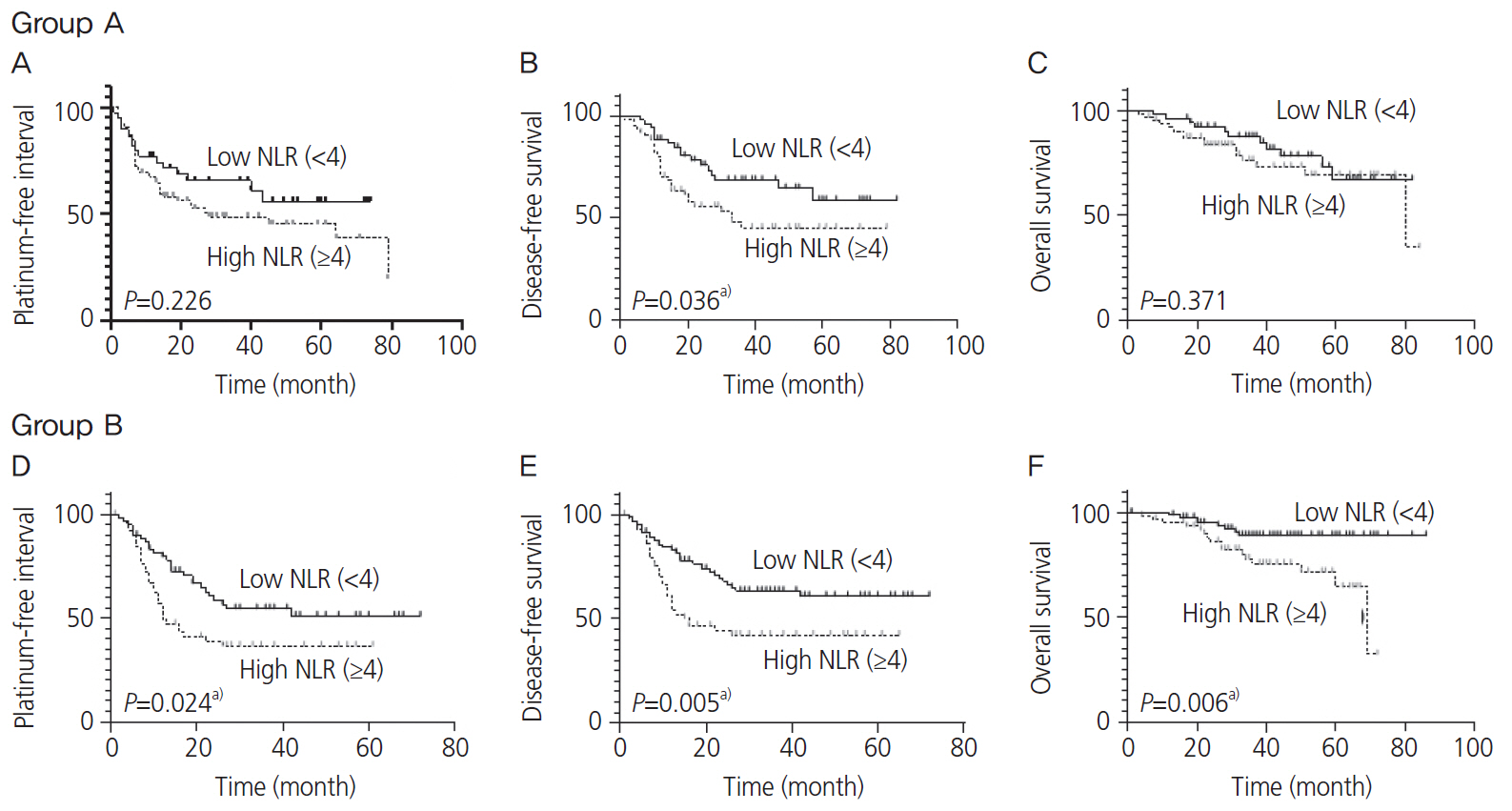
We enrolled 270 patients with ovarian cancer diagnosed at the Kyoto Medical Center (n=120; group A) and Kyoto University (n=150; group B). Data on 9 blood parameters (neutrophil to lymphocyte ratio [NLR], platelet to lymphocyte rate [PLR], C-reactive protein, lactate dehydrogenase [LDH], glucose, total cholesterol, high-density lipoprotein [HDL], low-density lipoprotein, and triglyceride levels), cancer pathology, cancer stage, cytoreduction outcomes, serum cancer antigen 125 levels, platinum-free interval (PFI), disease-free survival (DFS), and overall survival were assessed retrospectively.
Results
NLR, PLR, LDH, and HDL were significantly different in advanced stage patients (P<0.001, <0.001, 0.029, and <0.001, respectively). The Kaplan-Meier curves revealed that high LDH level (≥250 U/L) was associated with reduced PFI (P=0.037 and 0.012) and DFS (P=0.007 and 0.002) in groups A and B, respectively. High NLR (≥4) was associated with reduced DFS in both groups (P=0.036 and 0.005, respectively). LDH showed higher area under the curve (AUC) values in predicting platinum resistance with a PFI of less than 6 months and 12 months (AUC=0.606 and 0.646, respectively) than NLR. In the multivariate analysis, LDH remained significant (P=0.019) after adjusting for the 9 blood parameters.
Conclusion
Serum LDH level may possibly predict platinum resistance and prognosis in ovarian cancer and may be useful when developing precision medicine for individual patients.
Keyword
Figure
Reference
-
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7–34.
Article2. Elattar A, Bryant A, Winter-Roach BA, Hatem M, Naik R. Optimal primary surgical treatment for advanced epithelial ovarian cancer. Cochrane Database Syst Rev. 2011; 2011:CD007565.
Article3. Davis A, Tinker AV, Friedlander M. “Platinum resistant” ovarian cancer: what is it, who to treat and how to measure benefit? Gynecol Oncol. 2014; 133:624–31.
Article4. Gallo M, Sapio L, Spina A, Naviglio D, Calogero A, Naviglio S. Lactic dehydrogenase and cancer: an overview. Front Biosci (Landmark Ed). 2015; 20:1234–49.5. Huijgen HJ, Sanders GT, Koster RW, Vreeken J, Bossuyt PM. The clinical value of lactate dehydrogenase in serum: a quantitative review. Eur J Clin Chem Clin Biochem. 1997; 35:569–79.6. Wulaningsih W, Holmberg L, Garmo H, Malmstrom H, Lambe M, Hammar N, et al. Serum lactate dehydrogenase and survival following cancer diagnosis. Br J Cancer. 2015; 113:1389–96.
Article7. Bastani A, Asghary A, Heidari MH, Karimi-Busheri F. Evaluation of the sensitivity and specificity of serum level of prostasin, CA125, LDH, AFP, and hCG+β in epithelial ovarian cancer patients. Eur J Gynaecol Oncol. 2017; 38:418–24.8. Boran N, Kayikçioğlu F, Yalvaç S, Tulunay G, Ekinci U, Köse MF. Significance of serum and peritoneal fluid lactate dehydrogenase levels in ovarian cancer. Gynecol Obstet Invest. 2000; 49:272–4.
Article9. Xiang J, Zhou L, Zhuang Y, Zhang J, Sun Y, Li S, et al. Lactate dehydrogenase is correlated with clinical stage and grade and is downregulated by si-SATB1 in ovarian cancer. Oncol Rep. 2018; 40:2788–97.10. Liu X, Zhang W, Yin W, Xiao Y, Zhou C, Hu Y, et al. The prognostic value of the serum neuron specific enolase and lactate dehydrogenase in small cell lung cancer patients receiving first-line platinum-based chemotherapy. Medicine (Baltimore). 2017; 96:e8258.
Article11. Feng W, Wang Y, Zhu X. Baseline serum lactate dehydrogenase level predicts survival benefit in patients with metastatic colorectal cancer receiving bevacizumab as first-line chemotherapy: a systematic review and meta-analysis of 7 studies and 1,219 patients. Ann Transl Med. 2019; 7:133.
Article12. Jia Z, Zhang J, Wang Z, Wang B, Wang L, Cao J, et al. An explorative analysis of the prognostic value of lactate dehydrogenase for survival and the chemotherapeutic response in patients with advanced triple-negative breast cancer. Oncotarget. 2018; 9:10714–22.
Article13. Wen Q, Meng X, Xie P, Wang S, Sun X, Yu J. Evaluation of factors associated with platinum-sensitivity status and survival in limited-stage small cell lung cancer patients treated with chemoradiotherapy. Oncotarget. 2017; 8:81405–18.
Article14. Zaal EA, Berkers CR. The influence of metabolism on drug response in cancer. Front Oncol. 2018; 8:500.
Article15. Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009; 324:1029–33.
Article16. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420:860–7.
Article17. Chen G, Zhu L, Yang Y, Long Y, Li X, Wang Y. Prognostic role of neutrophil to lymphocyte ratio in ovarian cancer: a meta-analysis. Technol Cancer Res Treat. 2018; 17:1533033818791500.
Article18. Wang Y, Liu P, Xu Y, Zhang W, Tong L, Guo Z, et al. Preoperative neutrophil-to-lymphocyte ratio predicts response to first-line platinum-based chemotherapy and prognosis in serous ovarian cancer. Cancer Chemother Pharmacol. 2015; 75:255–62.
Article19. Miao Y, Yan Q, Li S, Li B, Feng Y. Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio are predictive of chemotherapeutic response and prognosis in epithelial ovarian cancer patients treated with platinum-based chemotherapy. Cancer Biomark. 2016; 17:33–40.
Article20. Kim YJ, Lee I, Chung YS, Nam E, Kim S, Kim SW, et al. Pretreatment neutrophil-to-lymphocyte ratio and its dynamic change during neoadjuvant chemotherapy as poor prognostic factors in advanced ovarian cancer. Obstet Gynecol Sci. 2018; 61:227–34.
Article21. Tian C, Song W, Tian X, Sun Y. Prognostic significance of platelet-to-lymphocyte ratio in patients with ovarian cancer: a meta-analysis. Eur J Clin Invest. 2018; 48:e12917.
Article22. Hefler LA, Concin N, Hofstetter G, Marth C, Mustea A, Sehouli J, et al. Serum C-reactive protein as independent prognostic variable in patients with ovarian cancer. Clin Cancer Res. 2008; 14:710–4.
Article23. Zhu F, Xu X, Shi B, Zeng L, Wang L, Wu X, et al. The positive predictive value of low-density lipoprotein for recurrence-free survival in ovarian cancer. Int J Gynaecol Obstet. 2018; 143:232–8.
Article24. Li AJ, Elmore RG, Chen IY, Karlan BY. Serum low-density lipoprotein levels correlate with survival in advanced stage epithelial ovarian cancers. Gynecol Oncol. 2010; 116:78–81.
Article25. Lamkin DM, Spitz DR, Shahzad MM, Zimmerman B, Lenihan DJ, Degeest K, et al. Glucose as a prognostic factor in ovarian carcinoma. Cancer. 2009; 115:1021–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the serum and cell lactate dehydrogenase isoenzyme in hematologic malignancies
- Follicular Lactate Dehydrogenase Activity and Steroid Concentrations in the Immature Gilt Ovary
- Diagnostic Efficiency of Peritoneal Fluid and Serum Lactate Dehydrogenase(LDH) in Ovarian Cancer Patients
- Extra-LDH Isoenzyme(LD₆) in Myocardial Infarction with Serious Course: Two cases report
- A case of advanced ovarian cancer which was treated with topotecan after taxol-cisplatin treatment failed