Ann Rehabil Med.
2020 Dec;44(6):438-449. 10.5535/arm.20081.
Prevalence and Characteristics of Neuropathic Pain in Patients With Spinal Cord Injury Referred to a Rehabilitation Center
- Affiliations
-
- 1Department of Rehabilitation Medicine, National Rehabilitation Center, Seoul, Korea
- KMID: 2510811
- DOI: http://doi.org/10.5535/arm.20081
Abstract
Objective
To identify the prevalence and characteristics of neuropathic pain (NP) in patients with spinal cord injury (SCI) and to investigate associations between NP and demographic or disease-related variables.
Methods
We retrospectively reviewed medical records of patients with SCI whose pain was classified according to the International Spinal Cord Injury Pain classifications at a single hospital. Multiple statistical analyses were employed. Patients aged <19 years, and patients with other neurological disorders and congenital conditions were excluded.
Results
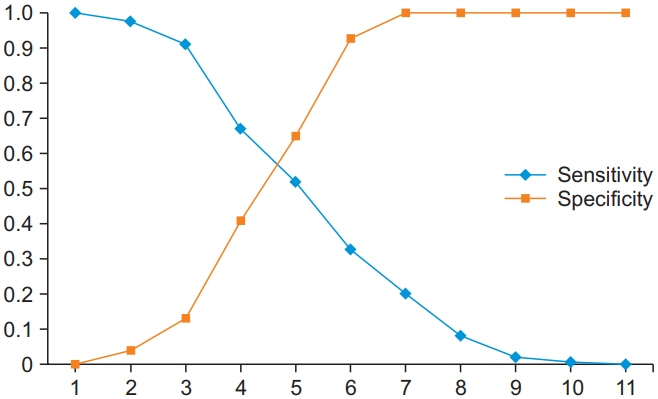
Of 366 patients, 253 patients (69.1%) with SCI had NP. Patients who were married or had traumatic injury or depressive mood had a higher prevalence rate. When other variables were controlled, marital status and depressive mood were found to be predictors of NP. There was no association between the prevalence of NP and other demographic or clinical variables. The mean Numeric Rating Scale (NRS) of NP was 4.52, and patients mainly described pain as tingling, squeezing, and painful cold. Females and those with below-level NP reported more intense pain. An NRS cut-off value of 4.5 was determined as the most appropriate value to discriminate between patients taking pain medication and those who did not.
Conclusion
In total, 69.1% of patients with SCI complained of NP, indicating that NP was a major complication. Treatment planning for patients with SCI and NP should consider that marital status, mood, sex, and pain subtype may affect NP, which should be actively managed in patients with an NRS ≥4.5.
Keyword
Figure
Reference
-
1. Budh NC, Lund I, Ertzgaard P, Holtz A, Hultling C, Levi R, et al. Pain in a Swedish spinal cord injury population. Clin Rehabil. 2003; 17:685–90.
Article2. van Gorp S, Kessels AG, Joosten EA, Kleef MV, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015; 19:5–14.
Article3. Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003; 103:249–57.
Article4. Burke D, Fullen BM, Stokes D, Lennon O. Neuropathic pain prevalence following spinal cord injury: a systematic review and meta-analysis. Eur J Pain. 2017; 21:29–44.
Article5. Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International spinal cord injury pain classification. Part I. Background and description. March 6-7, 2009. Spinal Cord. 2012; 50:413–7.6. Mahnig S, Landmann G, Stockinger L, Opsommer E. Pain assessment according to the international spinal cord injury pain classification in patients with spinal cord injury referred to a multidisciplinary pain center. Spinal Cord. 2016; 54:809–15.
Article7. Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord. 2005; 43:704–12.
Article8. Friedman AH, Nashold BS Jr. DREZ lesions for relief of pain related to spinal cord injury. J Neurosurg. 1986; 65:465–9.
Article9. Margolis JM, Juneau P, Sadosky A, Cappelleri JC, Bryce TN, Nieshoff EC. Health care resource utilization and medical costs of spinal cord injury with neuropathic pain in a commercially insured population in the United States. Arch Phys Med Rehabil. 2014; 95:2279–87.
Article10. Werhagen L, Budh CN, Hultling C, Molander C. Neuropathic pain after traumatic spinal cord injury: relations to gender, spinal level, completeness, and age at the time of injury. Spinal Cord. 2004; 42:665–73.11. Perry KN, Nicholas MK, Middleton J. Spinal cord injury-related pain in rehabilitation: a cross-sectional study of relationships with cognitions, mood and physical function. Eur J Pain. 2009; 13:511–7.
Article12. Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011; 34:535–46.
Article13. Beck AT, Steer RA, Brown GK. Beck Depression Inventory. 2nd ed. San Antonio, TX: Psychological Corp;1996.14. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982; 17:37–49.
Article15. Akpinar P, Atici A, Ozkan FU, Aktas I, Kulcu DG, Sari A, et al. Reliability of the modified Ashworth scale and modified Tardieu scale in patients with spinal cord injuries. Spinal Cord. 2017; 55:944–9.
Article16. Cho DY, Shin HI, Kim HR, Lee BS, Kim GR, Leigh JH, et al. Reliability and validity of the Korean version of the spinal cord independence measure III. Am J Phys Med Rehabil. 2020; 99:305–9.
Article17. Adriaansen JJ, Post MW, de Groot S, van Asbeck FW, Stolwijk-Swuste JM, Tepper M, et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med. 2013; 45:1016–22.
Article18. Werhagen L, Aito S, Tucci L, Strayer J, Hultling C. 25 years or more after spinal cord injury: clinical conditions of individuals in the Florence and Stockholm areas. Spinal Cord. 2012; 50:243–6.
Article19. Putzke JD, Richards JS, Hicken BL, Ness TJ, Kezar L, DeVivo M. Pain classification following spinal cord injury: the utility of verbal descriptors. Spinal Cord. 2002; 40:118–27.
Article20. Vall J, Costa CM, Tde JS, Costa SB. Neuropathic pain characteristics in patients from Curitiba (Brazil) with spinal cord injury. Arq Neuropsiquiatr. 2011; 69:64–8.
Article21. Teixeira MJ, Paiva WS, Assis MS, Fonoff ET, Bor-SengShu E, Cecon AD. Neuropathic pain in patients with spinal cord injury: report of 213 patients. Arq Neuropsiquiatr. 2013; 71:600–3.
Article22. Stormer S, Gerner HJ, Gruninger W, Metzmacher K, Follinger S, Wienke C, et al. Chronic pain/dysaesthesiae in spinal cord injury patients: results of a multicentre study. Spinal Cord. 1997; 35:446–55.
Article23. Perry KN, Nicholas MK, Middleton J, Siddall P. Psychological characteristics of people with spinal cord injury-related persisting pain referred to a tertiary pain management center. J Rehabil Res Dev. 2009; 46:57–67.24. Nakipoglu-Yuzer GF, Atci N, Ozgirgin N. Neuropathic pain in spinal cord injury. Pain Physician. 2013; 16:259–64.25. Gedde MH, Lilleberg HS, Abmus J, Gilhus NE, Rekand T. Traumatic vs non-traumatic spinal cord injury: a comparison of primary rehabilitation outcomes and complications during hospitalization. J Spinal Cord Med. 2019; 42:695–701.
Article26. Werhagen L, Hultling C, Molander C. The prevalence of neuropathic pain after non-traumatic spinal cord lesion. Spinal Cord. 2007; 45:609–15.
Article27. McKinley WO. Nontraumatic spinal cord injury: etiology, incidence and outcome. In : Kirshblum S, Campagnolo DI, DeLisa JA, editors. Spinal cord medicine. Philadelphia, PA: Lippincott Williams & Wilkins;2002. p. 471–79.28. Putzke JD, Richards JS, Hicken BL, DeVivo MJ. Interference due to pain following spinal cord injury: important predictors and impact on quality of life. Pain. 2002; 100:231–42.
Article29. Heutink M, Post MW, Luthart P, Schuitemaker M, Slangen S, Sweers J, et al. Long-term outcomes of a multidisciplinary cognitive behavioural programme for coping with chronic neuropathic spinal cord injury pain. J Rehabil Med. 2014; 46:540–5.
Article30. Lees JG, Fivelman B, Duffy SS, Makker PG, Perera CJ, Moalem-Taylor G. Cytokines in neuropathic pain and associated depression. In : Finn DP, Leonard BE, editors. Pain in psychiatric disorders. Basel, Switzerland: Karger;2015. p. 51–66.31. Aquarone RL, Nogueira PC. Central neuropathic pain: implications on quality of life of spinal cord injury patients. Revista Dor. 2015; 16:280–4.
Article32. Giardino ND, Jensen MP, Turner JA, Ehde DM, Cardenas DD. Social environment moderates the association between catastrophizing and pain among persons with a spinal cord injury. Pain. 2003; 106:19–25.
Article33. Forchheimer MB, Richards JS, Chiodo AE, Bryce TN, Dyson-Hudson TA. Cut point determination in the measurement of pain and its relationship to psychosocial and functional measures after traumatic spinal cord injury: a retrospective model spinal cord injury system analysis. Arch Phys Med Rehabil. 2011; 92:419–24.
Article34. Celik EC, Erhan B, Lakse E. The clinical characteristics of neuropathic pain in patients with spinal cord injury. Spinal Cord. 2012; 50:585–9.
Article35. Jang JY, Lee SH, Kim M, Ryu JS. Characteristics of neuropathic pain in patients with spinal cord injury. Ann Rehabil Med. 2014; 38:327–34.
Article36. Attal N, Cruccu G, Baron R, Haanpaa M, Hansson P, Jensen TS, Nurmikko T, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010; 17:1113–e88.
Article37. Nagoshi N, Kaneko S, Fujiyoshi K, Takemitsu M, Yagi M, Iizuka S, et al. Characteristics of neuropathic pain and its relationship with quality of life in 72 patients with spinal cord injury. Spinal Cord. 2016; 54:656–61.
Article38. Berkley KJ. Sex differences in pain. Behav Brain Sci. 1997; 20:371–80.
Article39. Gaudet AD, Ayala MT, Schleicher WE, Smith EJ, Bateman EM, Maier SF, et al. Exploring acute-to-chronic neuropathic pain in rats after contusion spinal cord injury. Exp Neurol. 2017; 295:46–54.
Article40. Hanley MA, Masedo A, Jensen MP, Cardenas D, Turner JA. Pain interference in persons with spinal cord injury: classification of mild, moderate, and severe pain. J Pain. 2006; 7:129–33.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Neuropathic Pain in Patients With Spinal Cord Injury
- Intractable Abdominal Pain in a Patient With Spinal Cord Injury: A Case Report
- Spinal Gap Junction Channels in Neuropathic Pain
- The Treatment of Central Pain after Spinal Cord Injury
- Dysesthetic Pain Syndrome in Spinal Cord Injury Patients