Korean J Transplant.
2020 Dec;34(4):257-264. 10.4285/kjt.20.0048.
The feasibility of organ transplantation during the COVID-19 outbreak: experiences from South Korea
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2510264
- DOI: http://doi.org/10.4285/kjt.20.0048
Abstract
- Background
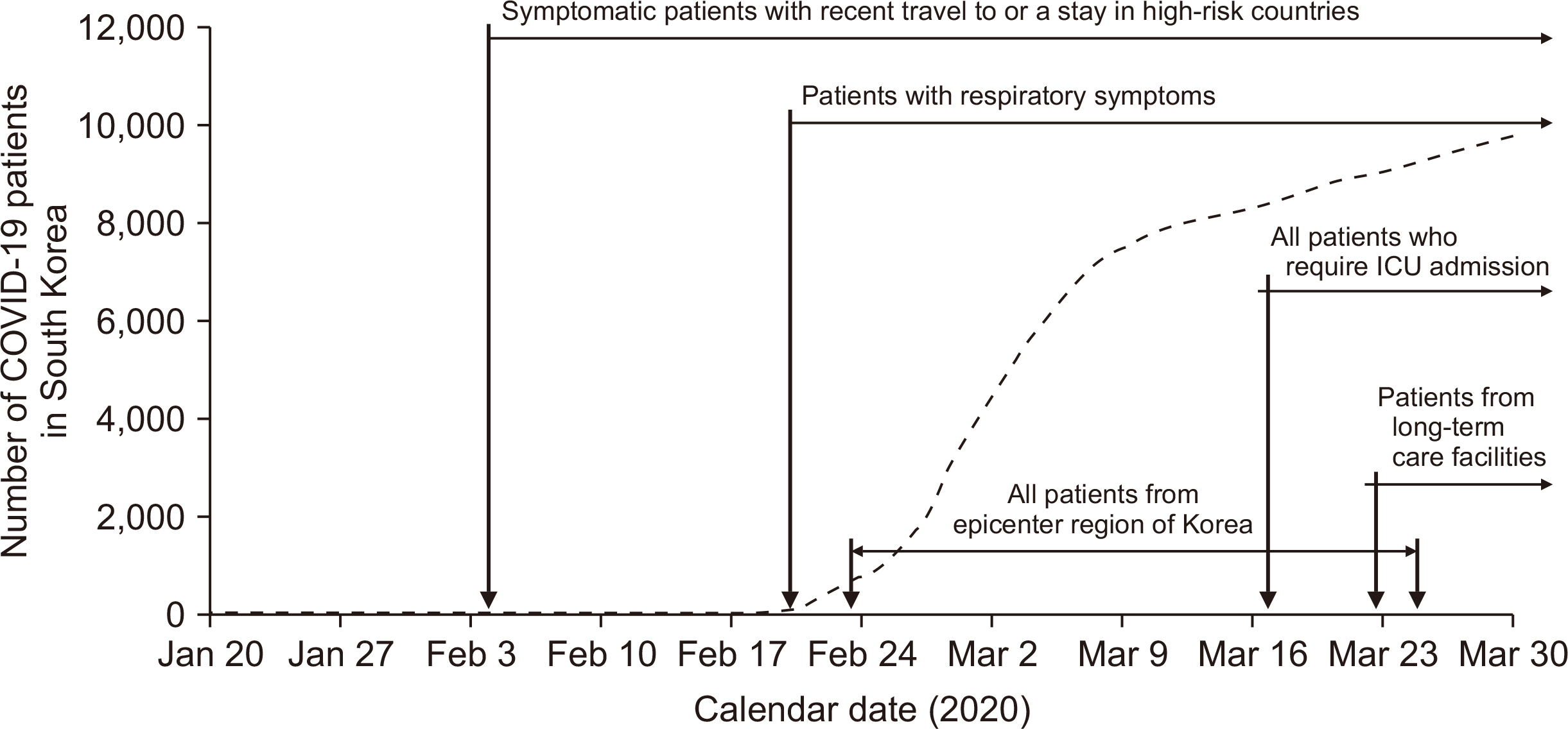
The coronavirus disease 2019 (COVID-19) has forced healthcare systems to reduce transplant activities in order to preserve resources and minimize the risk of nosocomial transmission. Although transplantation societies around the world have proposed interim recommendations, little is known about the safety of transplant surgery under pandemic conditions and how transplant medicine should move forward after the peak of the pandemic.
Methods
We describe our experiences regarding the continuation of living and deceased donor transplantation under infection control measures during the COVID-19 outbreak in South Korea. We reviewed consecutive liver and kidney transplantations at Severance Hospital and analyzed national transplantation activities in South Korea.
Results
Transplantation activities with living and deceased donors remained stable during the COVID-19 outbreak compared to the same period in 2019. We performed 94 transplantations (58 kidney, 35 liver, and 1 simultaneous liver-kidney) during the COVID-19 outbreak. Twenty-five patients underwent desensitization therapy prior to transplant (nine ABO-incompatible kidney, eight human leukocyte antigen-incompatible kidney, and eight ABO-incompatible liver). No transplant recipients in our center contracted COVID-19. In South Korea, national transplant activities with living and deceased donors remained stable in 2020 compared to 2019.
Conclusions
Organ transplantation during pandemics appears to be feasible with appropriate infection prevention measures.
Keyword
Figure
Cited by 2 articles
-
An analysis of the number of liver and kidney transplantations during COVID-19 pandemic in Korea
Jung-Ja Hong, Shin Hwang, Deog-Bok Moon, Young Hoon Kim, Sung Shin, In-Ok Kim, Sae-Rom Lee, Ah-Young Lee, Jiwon Woo
Korean J Transplant. 2021;35(4):247-252. doi: 10.4285/kjt.21.0030.Safely navigating kidney transplantation during the COVID-19 pandemic: the Singapore General Hospital’s experience
Carolyn Shan-Yeu Tien, Ian Tatt Liew, Quan Yao Ho, Sobhana Thangaraju, Maslinna Binte Abdul Rahman, Constance Lee, Nicole Chelsi Xin Hui Leah, Xia He, Li Ting Siew, Terence Yi Shern Kee
Korean J Transplant. 2023;37(2):95-102. doi: 10.4285/kjt.23.0020.
Reference
-
1. World Health Organization. WHO coronavirus disease (COVID-19) dashboard [Internet]. World Health Organization;Geneva: Available from: https://covid19.who.int/. cited 2020 May 18.2. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. 2020; Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 395:1054–62. DOI: 10.1016/S0140-6736(20)30566-3. PMID: 32171076. PMCID: PMC7270627.
Article3. Gori A, Dondossola D, Antonelli B, Mangioni D, Alagna L, Reggiani P, et al. 2020; Coronavirus disease 2019 and transplantation: a view from the inside. Am J Transplant. 20:1939–40. DOI: 10.1111/ajt.15853. PMID: 32181969.
Article4. Michaels MG, La Hoz RM, Danziger-Isakov L, Blumberg EA, Kumar D, Green M, et al. 2020; Coronavirus disease 2019: implications of emerging infections for transplantation. Am J Transplant. 20:1768–72. DOI: 10.1111/ajt.15832. PMID: 32090448.
Article5. Kumar D, Manuel O, Natori Y, Egawa H, Grossi P, Han SH, et al. 2020; COVID-19: a global transplant perspective on successfully navigating a pandemic. Am J Transplant. 20:1773–9. DOI: 10.1111/ajt.15876. PMID: 32202064. PMCID: PMC7228301.
Article6. Angelico R, Trapani S, Manzia TM, Lombardini L, Tisone G, Cardillo M. 2020; The COVID-19 outbreak in Italy: initial implications for organ transplantation programs. Am J Transplant. 20:1780–4. DOI: 10.1111/ajt.15904. PMID: 32243677.
Article7. Boyarsky BJ, Po-Yu Chiang T, Werbel WA, Durand CM, Avery RK, Getsin SN, et al. 2020; Early impact of COVID-19 on transplant center practices and policies in the United States. Am J Transplant. 20:1809–18. DOI: 10.1111/ajt.15915. PMID: 32282982. PMCID: PMC7262146.
Article8. Korean Network for Organ Sharing. Current status for organs transplantation [Internet]. Korean Network for Organ Sharing;Cheongju: Available from: https://www.konos.go.kr/. cited 2020 May 15.9. Lee J, Huh KH. 2020; Kidney transplantation trends in South Korea during the COVID-19 pandemic. Kidney Int. 98:512–3. DOI: 10.1016/j.kint.2020.05.044. PMID: 32569651. PMCID: PMC7305711.
Article10. Korean Society for Transplantation. 2020. Guidance on coronavirus disease 2019 (COVID-19) for transplant clinicians [Internet]. Korean Society for Transplantation;Seoul: Available from: https://www.mykst.org. cited 2020 March 21.11. Lee J, Lee JG, Kim S, Song SH, Kim BS, Kim HO, et al. 2016; The effect of rituximab dose on infectious complications in ABO-incompatible kidney transplantation. Nephrol Dial Transplant. 31:1013–21. DOI: 10.1093/ndt/gfw017. PMID: 27190360.
Article12. Lee J, Lee JG, Lee JJ, Kim MS, Ju MK, Choi GH, et al. 2015; Results of ABO-incompatible liver transplantation using a simplified protocol at a single institution. Transplant Proc. 47:723–6. DOI: 10.1016/j.transproceed.2015.02.004. PMID: 25891718.
Article13. COVID-19 National Emergency Response Center; Epidemiology & Case Management Team; Korea Centers for Disease Control & Prevention. 2020; Contact transmission of COVID-19 in South Korea: novel investigation techniques for tracing contacts. Osong Public Health Res Perspect. 11:60–3. DOI: 10.24171/j.phrp.2020.11.1.09. PMID: 32149043. PMCID: PMC7045882.14. Song JY, Yun JG, Noh JY, Cheong HJ, Kim WJ. 2020; Covid-19 in South Korea: challenges of subclinical manifestations. N Engl J Med. 382:1858–9. DOI: 10.1056/NEJMc2001801. PMID: 32251568. PMCID: PMC7154984.15. Park S, Choi GJ, Ko H. 2020; Information technology-based tracing strategy in response to COVID-19 in South Korea-privacy controversies. JAMA. 323:2129–30. DOI: 10.1001/jama.2020.6602. PMID: 32324202.
Article16. Fishman JA, Grossi PA. 2020; Novel Coronavirus-19 (COVID-19) in the immunocompromised transplant recipient: #Flatteningthecurve. Am J Transplant. 20:1765–7. DOI: 10.1111/ajt.15890. PMID: 32233057. PMCID: PMC7228206.
Article17. Kumar D, Tellier R, Draker R, Levy G, Humar A. 2003; Severe Acute Respiratory Syndrome (SARS) in a liver transplant recipient and guidelines for donor SARS screening. Am J Transplant. 3:977–81. DOI: 10.1034/j.1600-6143.2003.00197.x. PMID: 12859532. PMCID: PMC7175989.
Article18. Zhong Z, Zhang Q, Xia H, Wang A, Liang W, Zhou W, et al. 2020; Clinical characteristics and immunosuppressant management of coronavirus disease 2019 in solid organ transplant recipients. Am J Transplant. 20:1916–21. DOI: 10.1111/ajt.15928. PMID: 32282986. PMCID: PMC7262295.
Article19. Columbia University Kidney Transplant Program. 2020; Early description of coronavirus 2019 disease in kidney transplant recipients in New York. J Am Soc Nephrol. 31:1150–6. DOI: 10.1681/ASN.2020030375. PMID: 32317402. PMCID: PMC7269361.20. Bhoori S, Rossi RE, Citterio D, Mazzaferro V. 2020; COVID-19 in long-term liver transplant patients: preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol. 5:532–3. DOI: 10.1016/S2468-1253(20)30116-3. PMID: 32278366. PMCID: PMC7146678.
Article21. D'Antiga L. 2020; Coronaviruses and immunosuppressed patients: the facts during the third epidemic. Liver Transpl. 26:832–4. DOI: 10.1002/lt.25756. PMID: 32196933. PMCID: PMC7300680.22. Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, et al. 2020; Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 382:2049–55. DOI: 10.1056/NEJMsb2005114. PMID: 32202722.
Article23. Elizabeth Brindle M, Gawande A. 2020; Managing COVID-19 in surgical systems. Ann Surg. 272:e1–2. DOI: 10.1097/SLA.0000000000003923. PMID: 32209891. PMCID: PMC7188040.24. Tzedakis S, Jeddou H, Houssel-Debry P, Sulpice L, Boudjema K. 2020; COVID-19: thoughts and comments from a tertiary liver transplant center in France. Am J Transplant. 20:1952–53. DOI: 10.1111/ajt.15918. PMID: 32282972. PMCID: PMC7262076.
Article25. Leung K, Wu JT, Liu D, Leung GM. 2020; First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. Lancet. 395:1382–93. DOI: 10.1016/S0140-6736(20)30746-7. PMID: 32277878. PMCID: PMC7195331.
Article26. Ikizler TA. 2020; COVID-19 and dialysis units: what do we know now and what should we do? Am J Kidney Dis. 76:1–3. DOI: 10.1053/j.ajkd.2020.03.008. PMID: 32217082. PMCID: PMC7146661.
Article27. Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. 2020; The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 20:776–7. DOI: 10.1016/S1473-3099(20)30244-9. PMID: 32224313. PMCID: PMC7270047.
Article28. Cao X. 2020; COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 20:269–70. DOI: 10.1038/s41577-020-0308-3. PMID: 32273594. PMCID: PMC7143200.
Article29. Lipsitch M, Swerdlow DL, Finelli L. 2020; Defining the epidemiology of COVID-19: studies needed. N Engl J Med. 382:1194–6. DOI: 10.1056/NEJMp2002125. PMID: 32074416.30. Arons MM, Hatfield KM, Reddy SC, Kimball A, James A, Jacobs JR, et al. 2020; Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 382:2081–90. DOI: 10.1056/NEJMoa2008457. PMID: 32329971. PMCID: PMC7200056.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of COVID-19 on the number of deceased donors and organ transplantation in Western countries
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak
- COVID-19 from the Perspective of a Gastroenterologist
- The first case of brain death organ donation in a positive COVID-19 donors in Korea
- Impact of solid organ transplantation on the effectiveness of COVID-19 vaccination in hospitalized patients with COVID-19: a propensity score-matched cohort study