Heart Failure with Preserved Ejection Fraction: the Major Unmet Need in Cardiology
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2509024
- DOI: http://doi.org/10.4070/kcj.2020.0338
Abstract
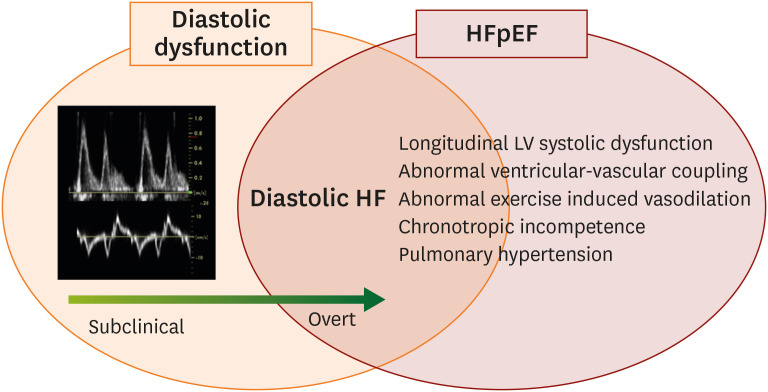
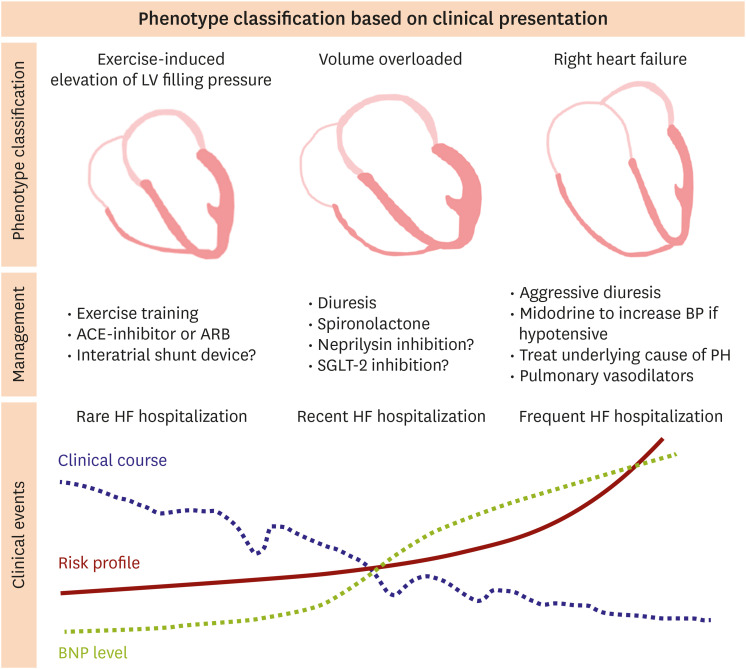
- Heart failure with preserved ejection fraction (HFpEF) has recently been recognized as the single greatest unmet need in cardiovascular medicine. As the population ages and the comorbidity increases, the prevalence of HFpEF increases considerably. Even though there have been large numbers of studies on pathophysiology, diagnosis, and treatment of HFpEF for latest years, there are no current pharmacologic interventions that can reduce mortality. HFpEF is currently understood as a heterogeneous syndrome originated from the interplay of cardiac and extracardiac abnormalities recognized by systemic inflammation, endothelial and coronary microvascular dysfunction, cardiomyocyte dysfunction and skeletal muscle dysfunction. The difficult “jigsaw puzzle” called HFpEF has been filled with some pieces, but it is still not enough to meet clinical needs. Here, we review recent evidences and unsolved problems about HFpEF to improve our understanding of HFpEF. Finally, we hope to accelerate to completion of the problematic “jigsaw puzzle”.
Keyword
Figure
Cited by 3 articles
-
Sex-Specific Trends in the Prevalence of Hypertension and the Number of People With Hypertension: Analysis of the Korea National Health and Nutrition Examination Survey (KNHANES) 1998–2018
Eunsun Seo, Sunjae Jung, Hokyou Lee, Hyeon Chang Kim
Korean Circ J. 2022;52(5):382-392. doi: 10.4070/kcj.2021.0347.Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Definition and Diagnosis
Jae Yeong Cho, Dong-Hyuk Cho, Jong-Chan Youn, Darae Kim, Sang Min Park, Mi-Hyang Jung, Junho Hyun, Jimi Choi, Hyun-Jai Cho, Seong-Mi Park, Jin-Oh Choi, Wook-Jin Chung, Byung-Su Yoo, Seok-Min Kang,
Korean Circ J. 2023;53(4):195-216. doi: 10.4070/kcj.2023.0046.Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Treatment
Jong-Chan Youn, Darae Kim, Jae Yeong Cho, Dong-Hyuk Cho, Sang Min Park, Mi-Hyang Jung, Junho Hyun, Hyun-Jai Cho, Seong-Mi Park, Jin-Oh Choi, Wook-Jin Chung, Byung-Su Yoo, Seok-Min Kang,
Korean Circ J. 2023;53(4):217-238. doi: 10.4070/kcj.2023.0047.
Reference
-
1. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–259. PMID: 16855265.
Article2. Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006; 355:260–269. PMID: 16855266.
Article3. Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2017; 14:591–602. PMID: 28492288.
Article4. Lee JH, Kim MS, Kim EJ, et al. KSHF guidelines for the management of acute heart failure: part I. definition, epidemiology and diagnosis of acute heart failure. Korean Circ J. 2019; 49:1–21. PMID: 30637993.
Article5. Lee JH, Kim MS, Yoo BS, et al. KSHF guidelines for the management of acute heart failure: part II. treatment of acute heart failure. Korean Circ J. 2019; 49:22–45. PMID: 30637994.
Article6. Kim MS, Lee JH, Cho HJ, et al. KSHF guidelines for the management of acute heart failure: part III. specific management of acute heart failure according to the etiology and co-morbidity. Korean Circ J. 2019; 49:46–68. PMID: 30637995.
Article7. Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure--abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med. 2004; 350:1953–1959. PMID: 15128895.
Article8. Oktay AA, Shah SJ. Diagnosis and management of heart failure with preserved ejection fraction: 10 key lessons. Curr Cardiol Rev. 2015; 11:42–52. PMID: 24251461.
Article9. Pfeffer MA, Shah AM, Borlaug BA. Heart failure with preserved ejection fraction in perspective. Circ Res. 2019; 124:1598–1617. PMID: 31120821.
Article10. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2013; 128:1810–1852. PMID: 23741057.11. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18:891–975. PMID: 27207191.12. Shah SJ, Katz DH, Deo RC. Phenotypic spectrum of heart failure with preserved ejection fraction. Heart Fail Clin. 2014; 10:407–418. PMID: 24975905.
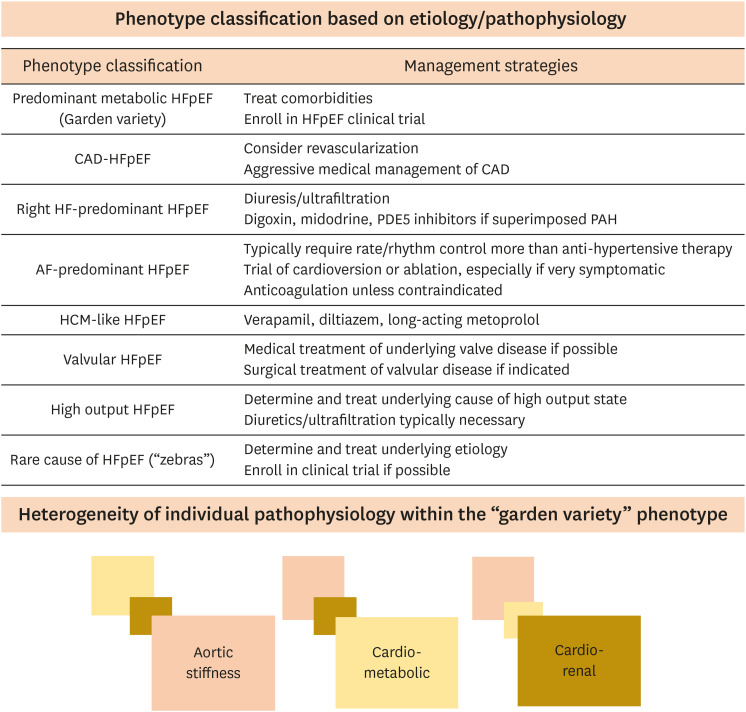
Article13. Shah SJ, Kitzman DW, Borlaug BA, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation. 2016; 134:73–90. PMID: 27358439.14. Lewis GA, Schelbert EB, Williams SG, et al. Biological phenotypes of heart failure with preserved ejection fraction. J Am Coll Cardiol. 2017; 70:2186–2200. PMID: 29050567.
Article15. Silverman DN, Shah SJ. Treatment of heart failure with preserved ejection fraction (HFpEF): the phenotype-guided approach. Curr Treat Options Cardiovasc Med. 2019; 21:20. PMID: 30982123.
Article16. Shah SJ, Katz DH, Selvaraj S, et al. Phenomapping for novel classification of heart failure with preserved ejection fraction. Circulation. 2015; 131:269–279. PMID: 25398313.
Article17. Shah SJ. 20th annual Feigenbaum lecture: echocardiography for precision medicine-digital biopsy to deconstruct biology. J Am Soc Echocardiogr. 2019; 32:1379–1395.e2. PMID: 31679580.
Article18. Obokata M, Kane GC, Reddy YNV, Olson TP, Melenovsky V, Borlaug BA. Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation. 2017; 135:825–838. PMID: 28039229.19. Henning RJ. Diagnosis and treatment of heart failure with preserved left ventricular ejection fraction. World J Cardiol. 2020; 12:7–25. PMID: 31984124.
Article20. Ha JW, Oh JK, Pellikka PA, et al. Diastolic stress echocardiography: a novel noninvasive diagnostic test for diastolic dysfunction using supine bicycle exercise Doppler echocardiography. J Am Soc Echocardiogr. 2005; 18:63–68. PMID: 15637491.
Article21. Ha JW, Andersen OS, Smiseth OA. Diastolic stress test: invasive and noninvasive testing. JACC Cardiovasc Imaging. 2020; 13:272–282. PMID: 31202741.22. Ha JW, Choi D, Park S, et al. Left ventricular diastolic functional reserve during exercise in patients with impaired myocardial relaxation at rest. Heart. 2009; 95:399–404. PMID: 18653572.
Article23. Choi EY, Shim CY, Kim SA, et al. Passive leg-raise is helpful to identify impaired diastolic functional reserve during exercise in patients with abnormal myocardial relaxation. J Am Soc Echocardiogr. 2010; 23:523–530. PMID: 20226626.
Article24. Choi EY, Ha JW, Rim SJ, et al. Incremental value of left ventricular diastolic function reserve index for predicting exercise capacity in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2008; 21:487–492. PMID: 17904804.
Article25. Moon J, Hong YJ, Kim YJ, et al. Extent of late gadolinium enhancement on cardiovascular magnetic resonance imaging and its relation to left ventricular longitudinal functional reserve during exercise in patients with hypertrophic cardiomyopathy. Circ J. 2013; 77:1742–1749. PMID: 23546472.
Article26. Holland DJ, Prasad SB, Marwick TH. Prognostic implications of left ventricular filling pressure with exercise. Circ Cardiovasc Imaging. 2010; 3:149–156. PMID: 20233862.
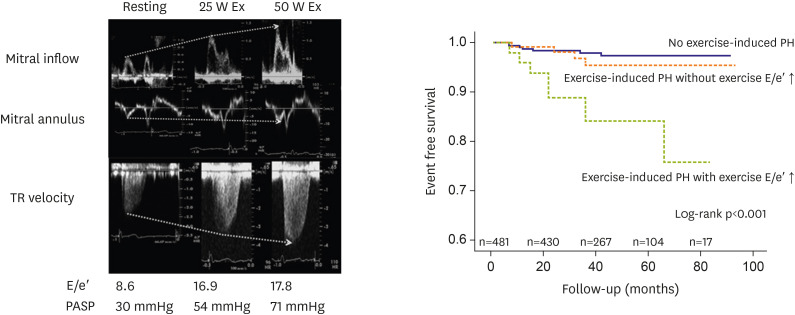
Article27. Shim CY, Kim SA, Choi D, et al. Clinical outcomes of exercise-induced pulmonary hypertension in subjects with preserved left ventricular ejection fraction: implication of an increase in left ventricular filling pressure during exercise. Heart. 2011; 97:1417–1424. PMID: 21653218.
Article28. Kim SA, Shim CY, Kim JM, et al. Impact of left ventricular longitudinal diastolic functional reserve on clinical outcome in patients with type 2 diabetes mellitus. Heart. 2011; 97:1233–1238. PMID: 21653219.
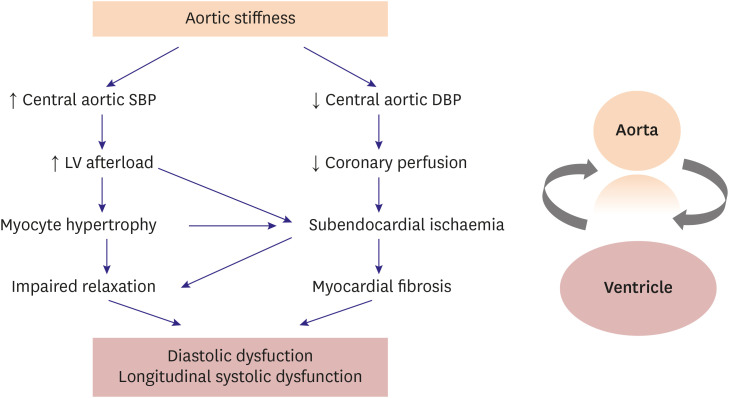
Article29. Mitchell GF. Arterial stiffness and hypertension: chicken or egg? Hypertension. 2014; 64:210–214. PMID: 24799614.30. Shim CY. Arterial-cardiac interaction: the concept and implications. J Cardiovasc Ultrasound. 2011; 19:62–66. PMID: 21860718.
Article31. Shim CY, Hong GR, Ha JW. Ventricular stiffness and ventricular-arterial coupling in heart failure: what is it, how to assess, and why? Heart Fail Clin. 2019; 15:267–274. PMID: 30832817.32. Mottram PM, Haluska BA, Leano R, Carlier S, Case C, Marwick TH. Relation of arterial stiffness to diastolic dysfunction in hypertensive heart disease. Heart. 2005; 91:1551–1556. PMID: 16287739.
Article33. Kim D, Shim CY, Hong GR, et al. Differences in left ventricular functional adaptation to arterial stiffness and neurohormonal activation in patients with hypertension: a study with two-dimensional layer-specific speckle tracking echocardiography. Clin Hypertens. 2017; 23:21. PMID: 29119005.
Article34. Shim CY, Park S, Choi EY, et al. The relationship between ventricular-vascular uncoupling during exercise and impaired left ventricular longitudinal functional reserve in hypertensive patients. J Am Soc Hypertens. 2013; 7:198–205. PMID: 23428411.
Article35. Shim CY, Hong GR, Park S, et al. Impact of central haemodynamics on left ventricular function in individuals with an exaggerated blood pressure response to exercise. J Hypertens. 2015; 33:612–620. PMID: 25479033.
Article36. Lee JS, Shim CY, Wi J, et al. Left ventricular diastolic function is closely associated with mechanical function of the left atrium in patients with paroxysmal atrial fibrillation. Circ J. 2013; 77:697–704. PMID: 23196755.
Article37. Shim CY, Yang WI, Park S, et al. Overweight and its association with aortic pressure wave reflection after exercise. Am J Hypertens. 2011; 24:1136–1142. PMID: 21833042.
Article38. Shim CY, Park S, Choi D, et al. Sex differences in central hemodynamics and their relationship to left ventricular diastolic function. J Am Coll Cardiol. 2011; 57:1226–1233. PMID: 21371640.
Article39. Park S, Ha JW, Shim CY, et al. Gender-related difference in arterial elastance during exercise in patients with hypertension. Hypertension. 2008; 51:1163–1169. PMID: 18259019.
Article40. Kass DA. Ventricular arterial stiffening: integrating the pathophysiology. Hypertension. 2005; 46:185–193. PMID: 15911741.41. Chirinos JA, Segers P, Hughes T, Townsend R. Large-artery stiffness in health and disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019; 74:1237–1263. PMID: 31466622.42. Weber T, Chirinos JA. Pulsatile arterial haemodynamics in heart failure. Eur Heart J. 2018; 39:3847–3854. PMID: 29947746.
Article43. Tan YT, Wenzelburger F, Lee E, et al. The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion. J Am Coll Cardiol. 2009; 54:36–46. PMID: 19555838.44. De Groote P, Lamblin N, Mouquet F, et al. Impact of diabetes mellitus on long-term survival in patients with congestive heart failure. Eur Heart J. 2004; 25:656–662. PMID: 15084370.
Article45. McHugh K, DeVore AD, Wu J, et al. Heart failure with preserved ejection fraction and diabetes: JACC state-of-the-art review. J Am Coll Cardiol. 2019; 73:602–611. PMID: 30732715.46. Shim CY, Park S, Choi EY, et al. Is albuminuria an indicator of myocardial dysfunction in diabetic patients without overt heart disease? A study with Doppler strain and strain rate imaging. Metabolism. 2008; 57:448–452. PMID: 18328343.
Article47. Shim CY, Song BW, Cha MJ, et al. Combination of a peroxisome proliferator-activated receptor-gamma agonist and an angiotensin II receptor blocker attenuates myocardial fibrosis and dysfunction in type 2 diabetic rats. J Diabetes Investig. 2014; 5:362–371.48. Dei Cas A, Khan SS, Butler J, et al. Impact of diabetes on epidemiology, treatment, and outcomes of patients with heart failure. JACC Heart Fail. 2015; 3:136–145. PMID: 25660838.
Article49. Heerspink HJ, Perkins BA, Fitchett DH, Husain M, Cherney DZ. Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation. 2016; 134:752–772. PMID: 27470878.50. Ha JW, Lee HC, Park S, et al. Gender-related difference in left ventricular diastolic elastance during exercise in patients with diabetes mellitus. Circ J. 2008; 72:1443–1448. PMID: 18724019.
Article51. Ha JW, Lee HC, Kang ES, et al. Abnormal left ventricular longitudinal functional reserve in patients with diabetes mellitus: implication for detecting subclinical myocardial dysfunction using exercise tissue Doppler echocardiography. Heart. 2007; 93:1571–1576. PMID: 17449503.
Article52. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–2128. PMID: 26378978.
Article53. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019; 380:347–357. PMID: 30415602.
Article54. Oh CM, Cho S, Jang JY, et al. Cardioprotective potential of an SGLT2 inhibitor against doxorubicin-induced heart failure. Korean Circ J. 2019; 49:1183–1195. PMID: 31456369.
Article55. Lee SG, Lee SJ, Lee JJ, et al. Anti-inflammatory effect for atherosclerosis progression by sodium-glucose cotransporter 2 (SGLT-2) inhibitor in a normoglycemic rabbit model. Korean Circ J. 2020; 50:443–457. PMID: 32153145.
Article56. Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med. 2002; 347:305–313. PMID: 12151467.
Article57. Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA. 1991; 266:231–236. PMID: 1829117.
Article58. Obokata M, Reddy YN, Pislaru SV, Melenovsky V, Borlaug BA. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation. 2017; 136:6–19. PMID: 28381470.
Article59. Tadic M, Cuspidi C. Obesity and heart failure with preserved ejection fraction: a paradox or something else? Heart Fail Rev. 2019; 24:379–385. PMID: 30610456.
Article60. Wolfe BM, Kvach E, Eckel RH. Treatment of obesity: weight loss and bariatric surgery. Circ Res. 2016; 118:1844–1855. PMID: 27230645.61. Fung JW, Li TS, Choy DK, et al. Severe obstructive sleep apnea is associated with left ventricular diastolic dysfunction. Chest. 2002; 121:422–429. PMID: 11834652.
Article62. McNicholas WT, Bonsigore MR. Management Committee of EU COST ACTION B26. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007; 29:156–178. PMID: 17197482.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-Invasive Hemodynamic Assessment of Heart Failure With Preserved Ejection Fraction
- Heart failure with preserved ejection fraction: insights from recent clinical researches
- Precision Cardiology: Phenotype-targeted Therapies for HFmrEF and HFpEF
- Optimal Management of Heart Failure with Preserve Ejection Fraction
- Simple and Practical Way of Assessing Diastolic Function: Diastolic Heart Failure Revisited