Ann Surg Treat Res.
2020 Dec;99(6):315-319. 10.4174/astr.2020.99.6.315.
Long-term outcomes of abdominal paraganglioma
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2508930
- DOI: http://doi.org/10.4174/astr.2020.99.6.315
Abstract
- Purpose
Paragangliomas (PGL) are rare neuroendocrine tumors derived from chromaffin cells of the autonomic nervous system. We aim to describe our experience and the long-term outcome of abdominal PGL over the last decade.
Methods
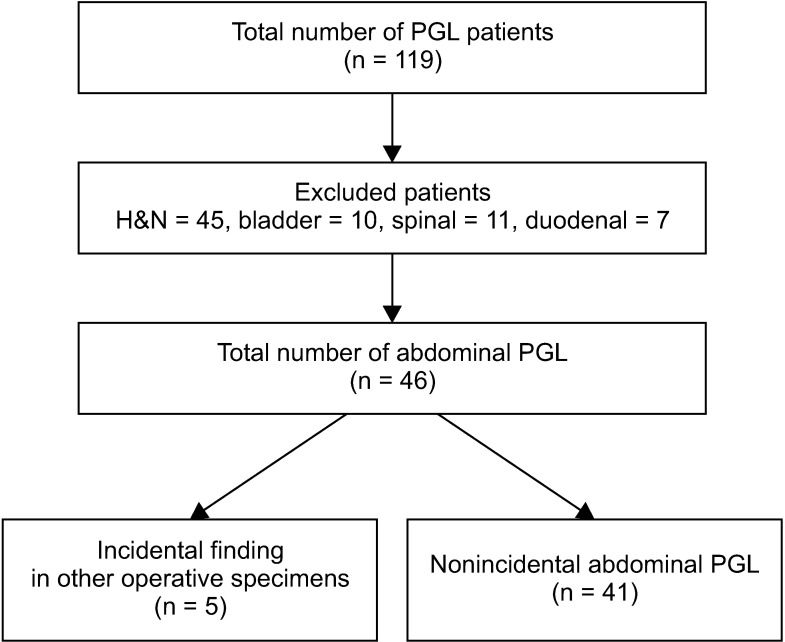
A retrospective review of patients diagnosed with PGL in our hospital between November 2005 and June 2017 was conducted. All nonabdominal PGL were excluded and the clinicopathological features and long-term outcomes of the patients were analyzed.
Results
A total of 46 patients were diagnosed with abdominal PGL. The average age of diagnosis was 55.4 years and there was no sex predilection. The average tumor size was 5.85 cm and they were predominantly located in the infrarenal position (50%). The mean follow-up period was 42 months (range, 1.8–252 months). All patients with metastases had Pheochromocytoma of the Adrenal Gland Scaled Score (PASS) of ≥4. One patient presented with synchronous metastases while 2 developed local recurrence and distant metastases. One presented with only local recurrence. One patient died 5 years after diagnosis.
Conclusion
Abdominal PGL is a rare tumor with excellent long-term prognosis. Recurrence although uncommon, can occur decades after initial diagnosis. Long-term follow-up is therefore recommended for all patients with PGL, especially in patients with PASS of ≥4.
Keyword
Figure
Reference
-
1. Pillai S, Gopalan V, Smith RA, Lam AK. Updates on the genetics and the clinical impacts on phaeochromocytoma and paraganglioma in the new era. Crit Rev Oncol Hematol. 2016; 100:190–208. PMID: 26839173.2. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2014; 99:1915–1942. PMID: 24893135.3. Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005; 366:665–675. PMID: 16112304.4. Chen H, Sippel RS, O'Dorisio MS, Vinik AI, Lloyd RV, Pacak K, et al. The North American Neuroendocrine Tumor Society consensus guideline for the diagnosis and management of neuroendocrine tumors: pheochromocytoma, paraganglioma, and medullary thyroid cancer. Pancreas. 2010; 39:775–783. PMID: 20664475.5. Galan SR, Kann PH. Genet ics and molecular pathogenesis of pheochromocytoma and paraganglioma. Clin Endocrinol (Oxf). 2013; 78:165–175. PMID: 23061808.6. Cunningham SC, Suh HS, Winter JM, Montgomery E, Schulick RD, Cameron JL, et al. Retroperitoneal paraganglioma: single-institution experience and review of the literature. J Gastrointest Surg. 2006; 10:1156–1163. PMID: 16966036.7. Ji XK, Zheng XW, Wu XL, Yu ZP, Shan YF, Zhang QY, et al. Diagnosis and surgical treatment of retroperitoneal paraganglioma: a single-institution experience of 34 cases. Oncol Lett. 2017; 14:2268–2280. PMID: 28789448.8. Xu W, Li H, Ji Z, Yan W, Zhang Y, Zhang X, et al. Retroperitoneal laparoscopic management of paraganglioma: a single institute experience. PLoS One. 2016; 11:e0149433. PMID: 26885838.9. Walz MK, Alesina PF, Wenger FA, Koch JA, Neumann HP, Petersenn S, et al. Laparoscopic and retroperitoneoscopic treatment of pheochromocytomas and retroperitoneal paragangliomas: results of 161 tumors in 126 patients. World J Surg. 2006; 30:899–908. PMID: 16617419.10. Wang J, Li Y, Xiao N, Duan J, Yang N, Bao J, et al. Retroperitoneoscopic resection of primary paraganglioma: single-center clinical experience and literature review. J Endourol. 2014; 28:1345–1351. PMID: 24955712.11. Alemanno G, Bergamini C, Somigli R, Prosperi P, Bruscino A, Valeri A. Abdominal paragangliomas: a quantitative prognostic score as predictive factor of the feasibility of the laparoscopic approach. Updates Surg. 2017; 69:509–515. PMID: 28537037.12. Kang SW, Kandil E, Kim MJ, Kim KS, Lee CR, Jeong JJ, et al. Posterior retroperitoneoscopic resection of extra-adrenal paraganglioma located in the aorto-caval space. Ann Surg Oncol. 2018; 25:963. PMID: 29330717.13. Williams MD. Paragangliomas of the head and neck: an overview from diagnosis to genetics. Head Neck Pathol. 2017; 11:278–287. PMID: 28321772.14. Thompson LD. Pheochromocytoma of the Adrenal gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol. 2002; 26:551–566. PMID: 11979086.15. Wu D, Tischler AS, Lloyd RV, DeLellis RA, de Krijger R, van Nederveen F, et al. Observer variation in the application of the Pheochromocytoma of the Adrenal Gland Scaled Score. Am J Surg Pathol. 2009; 33:599–608. PMID: 19145205.16. Koh JM, Ahn SH, Kim H, Kim BJ, Sung TY, Kim YH, et al. Validation of pathological grading systems for predicting metastatic potential in pheochromocytoma and paraganglioma. PLoS One. 2017; 12:e0187398. PMID: 29117221.17. Kimura N, Takayanagi R, Takizawa N, Itagaki E, Katabami T, Kakoi N, et al. Pathological grading for predicting metastasis in phaeochromocytoma and paraganglioma. Endocr Relat Cancer. 2014; 21:405–414. PMID: 24521857.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Paraganglioma Arising in the Transverse Mesocolon
- A Case of Extra-adrenal Paraganglioma of the Retroperitoneum
- Paraganglioma of the Cauda Equina: Case Report
- A Case of Retroperitoneal Paraganglioma Accompanying Bile Duct Dilatation
- Incidental Mesenteric Paraganglioma: A Case Report and Literature Review