Endocrinol Metab.
2020 Sep;35(3):602-609. 10.3803/EnM.2020.741.
Clinical Outcomes of N1b Papillary Thyroid Cancer Patients Treated with Two Different Doses of Radioiodine Ablation Therapy
- Affiliations
-
- 1Department of 1Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Nuclear Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2508010
- DOI: http://doi.org/10.3803/EnM.2020.741
Abstract
- Background
The optimal dose of radioactive iodine (RAI) therapy for N1b papillary thyroid carcinoma (PTC) is controversial. We evaluated the clinical outcome of N1b PTC patients treated with either 100 or 150 mCi of RAI.
Methods
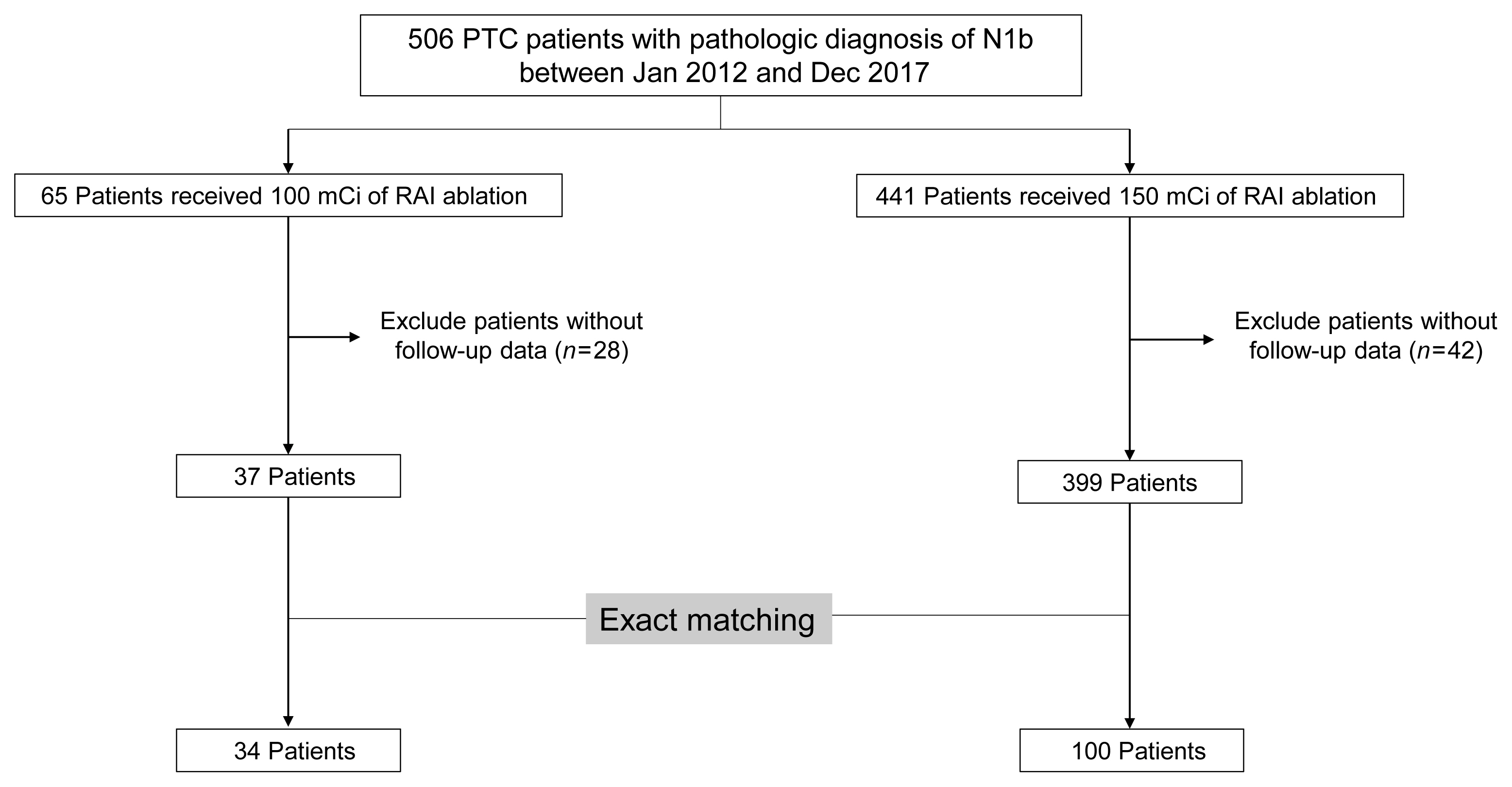
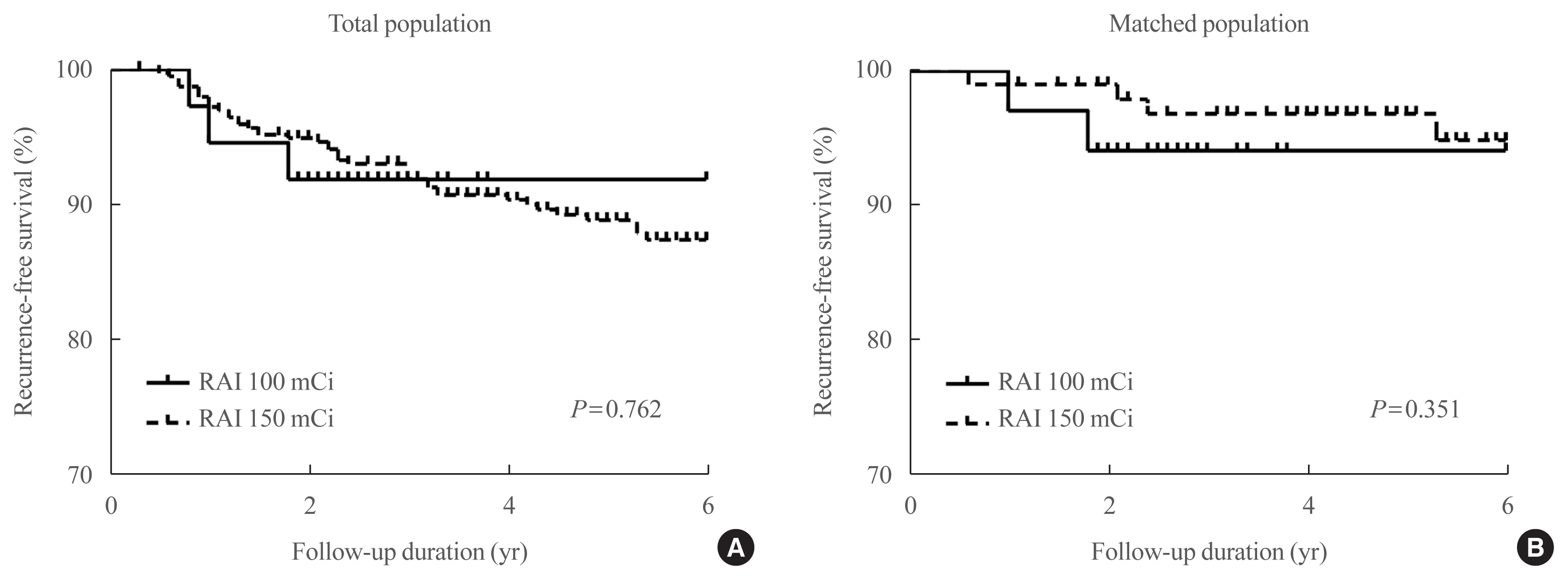
We retrospectively analyzed N1b PTC patients who underwent total thyroidectomy and postoperative RAI therapy at a tertiary referral center between 2012 and 2017. As the baseline characteristics differed between treatment groups, we performed exact matching for various pathological factors according to RAI dose. We evaluated the response to therapy and recurrence-free survival (RFS) in the matched patients. Structural recurrent/persistent disease was defined as new structural disease detected after initial therapy, which was confirmed by cytology or pathology.
Results
Of the total 436 patients, 37 (8.5%) received 100 mCi of RAI and 399 (91.5%) received 150 mCi of RAI. After an exact 1:3 matching, 34 patients in the 100 mCi group and 100 patients in the 150 mCi group remained. There was no significant difference in response to therapy between the groups in the matched population (P=0.63). An excellent response was achieved in 70.6% (n=24) of patients in the 100 mCi group and 76.0% (n=76) in the 150 mCi group. Two (5.9%) patients in the 100 mCi group and four (4.0%) in the 150 mCi group had recurrence and there was no significant difference in RFS between the groups in the matched population (P=0.351).
Conclusion
There were no differences in response to therapy and RFS in N1b PTC patients according to RAI dose.
Keyword
Figure
Reference
-
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133.
Article2. Schlumberger M, Catargi B, Borget I, Deandreis D, Zerdoud S, Bridji B, et al. Strategies of radioiodine ablation in patients with low-risk thyroid cancer. N Engl J Med. 2012; 366:1663–73.
Article3. Sabra MM, Grewal RK, Ghossein RA, Tuttle RM. Higher administered activities of radioactive iodine are associated with less structural persistent response in older, but not younger, papillary thyroid cancer patients with lateral neck lymph node metastases. Thyroid. 2014; 24:1088–95.
Article4. Podnos YD, Smith D, Wagman LD, Ellenhorn JD. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg. 2005; 71:731–4.
Article5. Zaydfudim V, Feurer ID, Griffin MR, Phay JE. The impact of lymph node involvement on survival in patients with papillary and follicular thyroid carcinoma. Surgery. 2008; 144:1070–7.
Article6. Leboulleux S, Rubino C, Baudin E, Caillou B, Hartl DM, Bidart JM, et al. Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab. 2005; 90:5723–9.
Article7. Ito Y, Kudo T, Takamura Y, Kobayashi K, Miya A, Miyauchi A. Lymph node recurrence in patients with N1b papillary thyroid carcinoma who underwent unilateral therapeutic modified radical neck dissection. World J Surg. 2012; 36:593–7.
Article8. Baek SK, Jung KY, Kang SM, Kwon SY, Woo JS, Cho SH, et al. Clinical risk factors associated with cervical lymph node recurrence in papillary thyroid carcinoma. Thyroid. 2010; 20:147–52.
Article9. Lee SH, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, et al. Risk factors for recurrence after treatment of N1b papillary thyroid carcinoma. Ann Surg. 2019; 269:966–71.
Article10. Liu YQ, Li H, Liu JR, Lin YS. Unfavorable responses to radioiodine therapy in N1b papillary thyroid cancer: a propensity score matching study. Endocr Pract. 2019; 25:1286–94.
Article11. Beierwaltes WH, Rabbani R, Dmuchowski C, Lloyd RV, Eyre P, Mallette S. An analysis of “ablation of thyroid remnants” with I-131 in 511 patients from 1947–1984: experience at University of Michigan. J Nucl Med. 1984; 25:1287–93.12. Jeon MJ, Kim WG, Park WR, Han JM, Kim TY, Song DE, et al. Modified dynamic risk stratification for predicting recurrence using the response to initial therapy in patients with differentiated thyroid carcinoma. Eur J Endocrinol. 2013; 170:23–30.
Article13. Kim WB. A closer look at papillary thyroid carcinoma. Endocrinol Metab (Seoul). 2015; 30:1–6.
Article14. Yi KH. The revised 2016 Korean Thyroid Association guidelines for thyroid nodules and cancers: differences from the 2015 American Thyroid Association guidelines. Endocrinol Metab (Seoul). 2016; 31:373–8.
Article15. Lamartina L, Grani G, Durante C, Borget I, Filetti S, Schlumberger M. Follow-up of differentiated thyroid cancer: what should (and what should not) be done. Nat Rev Endocrinol. 2018; 14:538–51.
Article16. Jeong SY, Lee SW, Kim WW, Jung JH, Lee WK, Ahn BC, et al. Clinical outcomes of patients with T4 or N1b well-differentiated thyroid cancer after different strategies of adjuvant radioiodine therapy. Sci Rep. 2019; 9:5570.
Article17. Mallick U, Harmer C, Yap B, Wadsley J, Clarke S, Moss L, et al. Ablation with low-dose radioiodine and thyrotropin alfa in thyroid cancer. N Engl J Med. 2012; 366:1674–85.
Article18. Han JM, Kim WG, Kim TY, Jeon MJ, Ryu JS, Song DE, et al. Effects of low-dose and high-dose postoperative radioiodine therapy on the clinical outcome in patients with small differentiated thyroid cancer having microscopic extrathyroidal extension. Thyroid. 2014; 24:820–5.
Article19. Caglar M, Bozkurt FM, Akca CK, Vargol SE, Bayraktar M, Ugur O, et al. Comparison of 800 and 3700 MBq iodine-131 for the postoperative ablation of thyroid remnant in patients with low-risk differentiated thyroid cancer. Nucl Med Commun. 2012; 33:268–74.
Article20. Castagna MG, Cevenini G, Theodoropoulou A, Maino F, Memmo S, Claudia C, et al. Post-surgical thyroid ablation with low or high radioiodine activities results in similar outcomes in intermediate risk differentiated thyroid cancer patients. Eur J Endocrinol. 2013; 169:23–9.
Article21. Sellers M, Beenken S, Blankenship A, Soong SJ, Turbat-Herrera E, Urist M, et al. Prognostic significance of cervical lymph node metastases in differentiated thyroid cancer. Am J Surg. 1992; 164:578–81.
Article22. Rosario PW, Borges MA, Purisch S. Preparation with recombinant human thyroid-stimulating hormone for thyroid remnant ablation with 131I is associated with lowered radiotoxicity. J Nucl Med. 2008; 49:1776–82.23. Kloos RT, Duvuuri V, Jhiang SM, Cahill KV, Foster JA, Burns JA. Nasolacrimal drainage system obstruction from radioactive iodine therapy for thyroid carcinoma. J Clin Endocrinol Metab. 2002; 87:5817–20.
Article24. Jeong SY, Kim HW, Lee SW, Ahn BC, Lee J. Salivary gland function 5 years after radioactive iodine ablation in patients with differentiated thyroid cancer: direct comparison of pre- and postablation scintigraphies and their relation to xerostomia symptoms. Thyroid. 2013; 23:609–16.
Article25. Mandel SJ, Mandel L. Radioactive iodine and the salivary glands. Thyroid. 2003; 13:265–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Augmentation of Radioiodine Uptake by Pulmonary Metastasis of Papillary Thyroid Carcinoma Treated with Dabrafenib and Trametinib
- Low Dose versus High Dose Radioiodine Therapy
- Recent Advances in Radioiodine Therapy for Thyroid Cancer
- Comparison of Diagnostic and Post-therapy Radioiodine Scan in Well-Differentiated Thyroid Cancer and the Clinical Outcome
- Radioiodine Therapy in a Patient with Papillary Thyroid Carcinoma associated with Breast Uptake ; Hyperprolactinemia due to Empty Sella Syndrome