Clin Endosc.
2020 Sep;53(5):541-549. 10.5946/ce.2019.161.
Endoscopic Full Thickness Resection for Gastrointestinal Tumors - Challenges and Solutions
- Affiliations
-
- 1Department of General Surgery, National University Hospital, Singapore, Singapore
- 2Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- KMID: 2507587
- DOI: http://doi.org/10.5946/ce.2019.161
Abstract
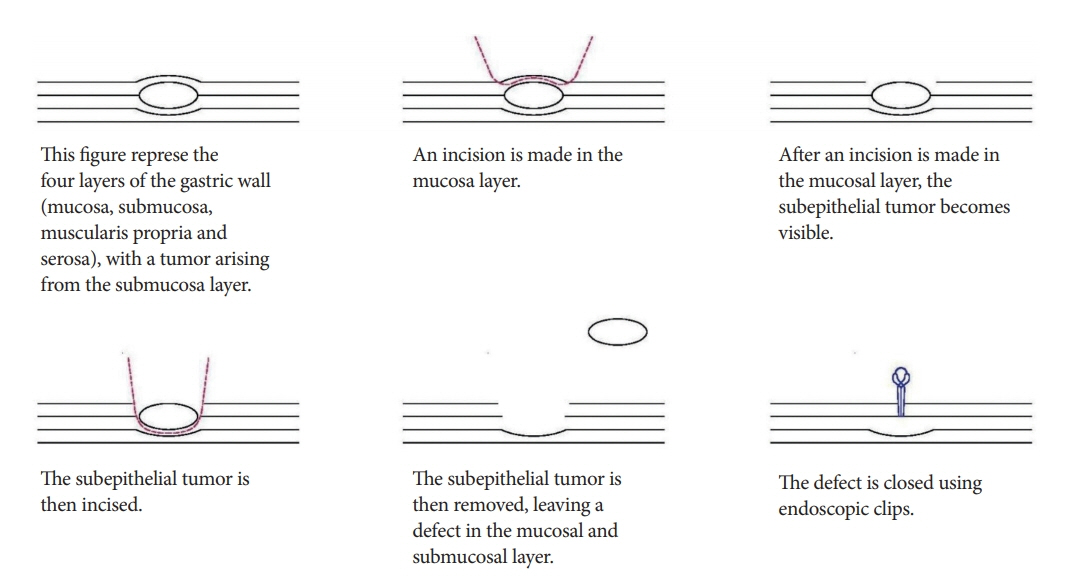
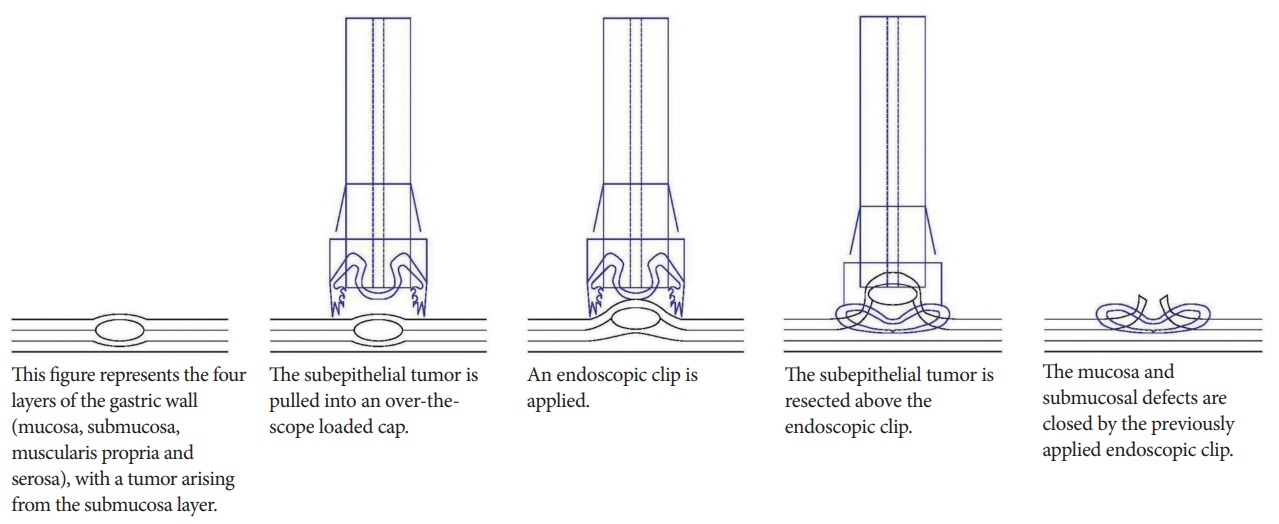
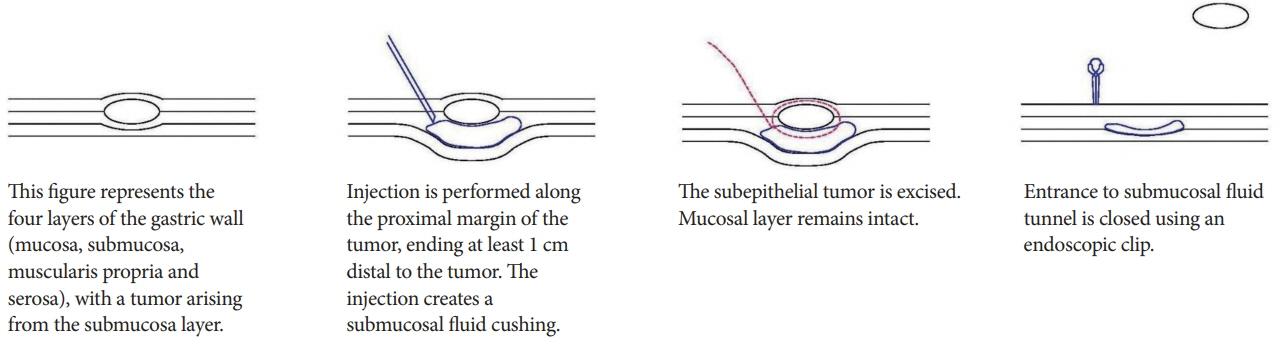
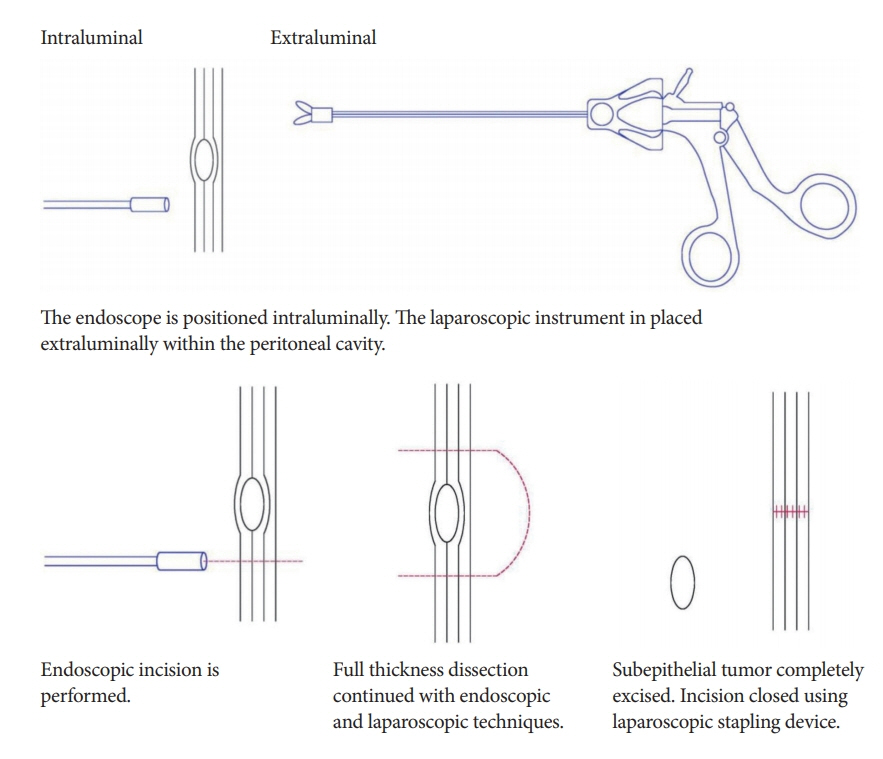
- Standard polypectomy, endoscopic mucosal resection, and endoscopic submucosal dissection (ESD) are established techniques for the treatment of gastrointestinal tumors. However, resection of submucosal tumors via ESD often results in low rates of microscopically margin-negative (R0) resection and high rates of perforation. Endoscopic full thickness resection (EFTR) overcomes this adverse event and aids in the therapeutic management of complex tumors.
Multiple techniques for EFTR have been developed, each with its own advantages and disadvantages. Submucosal tunneling and nonexposed techniques are generally preferable, because the layer of overlying intact mucosa reduces the incidence of intraperitoneal contamination by the gastric fluid and dissemination of the tumor cells. However, adoption of EFTR by endoscopists in clinical practice remains low. The major challenge seems to be the technical difficulty in performing laparoscopic and/or endoscopic suturing using the currently available instruments.
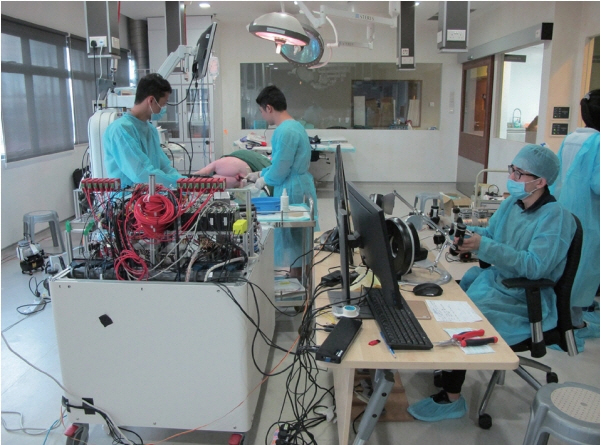
We developed a novel robotic endoscopic platform with suturing capabilities to overcome the technical challenges of suturing. This platform allows easy maneuvering and triangulation of the instruments, thus facilitating endoscopic suturing using robotic arms. Our studies have demonstrated that this robotic endoscopic platform with suturing capabilities is an effective and safe method for performing EFTR with endoscopic suturing.
Figure
Cited by 2 articles
-
Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clin Endosc. 2021;54(5):633-640. doi: 10.5946/ce.2021.216.Endoscopic resection penetrating the muscularis propria for gastric gastrointestinal stromal tumors: advances and challenges
Jin Woong Cho
Clin Endosc. 2024;57(3):329-331. doi: 10.5946/ce.2024.036.
Reference
-
1. Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009; 69:1228–1235.
Article2. Chun SY, Kim KO, Park DS, et al. Endoscopic submucosal dissection as a treatment for gastric subepithelial tumors that originate from the muscularis propria layer: a preliminary analysis of appropriate indications. Surg Endosc. 2013; 27:3271–3279.
Article3. He Z, Sun C, Wang J, et al. Efficacy and safety of endoscopic submucosal dissection in treating gastric subepithelial tumors originating in the muscularis propria layer: a single-center study of 144 cases. Scand J Gastroenterol. 2013; 48:1466–1473.
Article4. Białek A, Wiechowska-Kozłowska A, Pertkiewicz J, et al. Endoscopic submucosal dissection for treatment of gastric subepithelial tumors (with video). Gastrointest Endosc. 2012; 75:276–286.5. Kuellmer A, Mueller J, Caca K, et al. Endoscopic full-thickness resection for early colorectal cancer. Gastrointest Endosc. 2019; 89:1180–1189.e1.
Article6. Dellatore P, Bhagat V, Kahaleh M. Endoscopic full thickness resection versus submucosal tunneling endoscopic resection for removal of submucosal tumors: a review article. Transl Gastroenterol Hepatol. 2019; 4:45.
Article7. Kim SY, Kim KO. Endoscopic treatment of subepithelial tumors. Clin Endosc. 2018; 51:19–27.
Article8. Ye LP, Zhu LH, Zhou XB, Mao XL, Zhang Y. Endoscopic excavation for the treatment of small esophageal subepithelial tumors originating from the muscularis propria. Hepatogastroenterology. 2015; 62:65–68.9. Jeong ID, Jung SW, Bang SJ, Shin JW, Park NH, Kim DH. Endoscopic enucleation for gastric subepithelial tumors originating in the muscularis propria layer. Surg Endosc. 2011; 25:468–474.
Article10. Liu BR, Song JT, Qu B, Wen JF, Yin JB, Liu W. Endoscopic muscularis dissection for upper gastrointestinal subepithelial tumors originating from the muscularis propria. Surg Endosc. 2012; 26:3141–3148.
Article11. Mori H, Rahman A, Kobara H, et al. Current status of exposed endoscopic full-thickness resection and further development of non-exposed endoscopic full-thickness resection. Digestion. 2017; 95:6–15.
Article12. Chen T, Zhou PH, Chu Y, et al. Long-term outcomes of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors. Ann Surg. 2017; 265:363–369.
Article13. Niimi K, Ishibashi R, Mitsui T, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal tumor. Ann Transl Med. 2017; 5:187.
Article14. Mitsui T, Yamashita H, Aikou S, Niimi K, Fujishiro M, Seto Y. Non-exposed endoscopic wall-inversion surgery for gastrointestinal stromal tumor. Transl Gastroenterol Hepatol. 2018; 3:17.
Article15. Kaan HL, Ho KY. Robot-assisted endoscopic resection: current status and future directions. Gut Liver. 2020; 14:150–152.
Article16. Chiu PW, Phee SJ, Wang Z, et al. Feasibility of full-thickness gastric resection using master and slave transluminal endoscopic robot and closure by Overstitch: a preclinical study. Surg Endosc. 2014; 28:319–324.
Article17. Kaan HL, Ho KY. Endoscopic robotic suturing: the way forward. Saudi J Gastroenterol. 2019; 25:272–276.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Full-Thickness Resection for Gastric Subepithelial Lesions Arising from the Muscularis Propria
- Endoscopic Full-thickness Resection for Gastric Tumor
- Omental Patching and Purse-String Endosuture Closure after Endoscopic Full-Thickness Resection in Patients with Gastric Gastrointestinal Stromal Tumors
- Endoscopic Treatment of Subepithelial Tumors
- Current Techniques for Treating Gastrointestinal Stromal Tumors in the Upper Gastrointestinal Tract