Prog Med Phys.
2020 Sep;31(3):99-110. 10.14316/pmp.2020.31.3.99.
Proton Therapy Review: Proton Therapy from a Medical
- Affiliations
-
- 1Department of Radiation Oncology & Proton Therapy Center, National Cancer Center, Goyang, Korea
- KMID: 2507482
- DOI: http://doi.org/10.14316/pmp.2020.31.3.99
Abstract
- With hope and concern, the first Korean proton therapy facility was introduced to the National Cancer Center (NCC) in 2007. It added a new chapter to the history of Korean radiation therapy. There have been challenging clinical trials using proton beam therapy, which has seen many impressive results in cancer treatment. Compared to the rapidly increasing number of proton therapy facilities in the world, only one more proton therapy center has been added since 2007 in Korea. The Samsung Medical Center installed a proton therapy facility in 2015. Most radiation oncology practitioners would agree that the physical properties of the proton beam provide a clear advantage in radiation treatment. But the expensive cost of proton therapy facilities is still one of the main reasons that hospitals are reluctant to introduce them in Korea. I herein introduce the history of proton therapy and the cutting edge technology used in proton therapy. In addition, I will cover the role of a medical physicist in proton therapy and the future prospects of proton therapy, based on personal experience in participating in proton therapy programs from the beginning at the NCC.
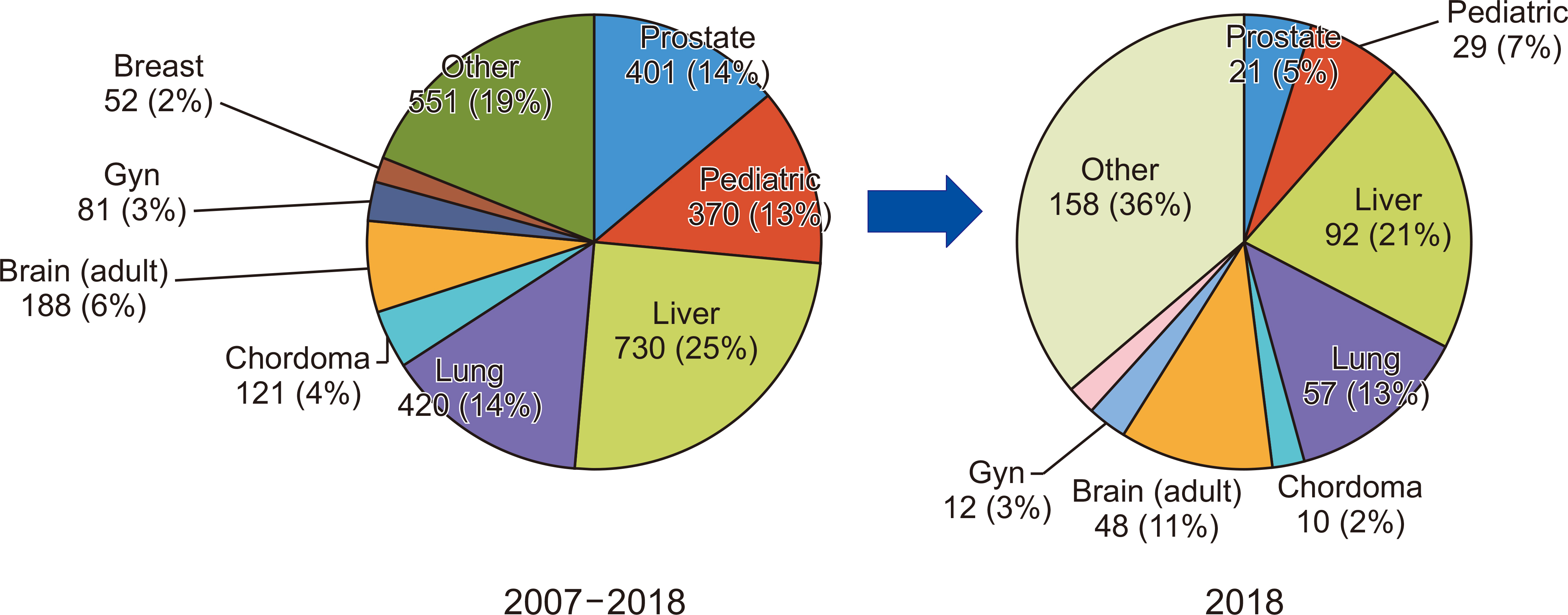
Figure
Cited by 1 articles
-
Feasibility Test of Flat-Type Faraday Cup for Ultrahigh-Dose-Rate Transmission Proton Beam Therapy
Sang-il Pak, Sungkoo Cho, Seohyeon An, Seonghoon Jeong, Dongho Shin, Youngkyung Lim, Jong Hwi Jeong, Haksoo Kim, Se Byeong Lee
Prog Med Phys. 2022;33(4):108-113. doi: 10.14316/pmp.2022.33.4.108.
Reference
-
References
1. Leo WR. The bethe-bloch formula. 1994. Techniques for nuclear and particle physics experiments. 2nd ed. Spriger-Verlag;Berlin, Heidelberg: DOI: 10.1007/978-3-642-57920-2.2. Shin J, Park S, Kim H, Kim M, Jeong C, Cho S, et al. 2015; Proton linear energy transfer measurement using emulsion cloud chamber. Nucl Instrum Methods Phys Res B. 349:201–208. DOI: 10.1016/j.nimb.2014.12.083.
Article3. International Commission on Radiation Units & Measurements. 2007. Report 78: prescribing, recording, and reporting proton-beam therapy. International Commission on Radiation Units & Measurements;Bethesda:4. Baek HJ, Kim TH, Shin D, Kwak JW, Choo DW, Lee SB, et al. 2008; Radiobiological characterization of proton beam at the National Cancer Center in Korea. J Radiat Res. 49:509–515. DOI: 10.1269/jrr.08017. PMID: 18567940.
Article5. Lawrence E, Livingston M. 1931; The production of high speed protons without the use of high voltages. Phys Rev. 38:834. DOI: 10.1103/PhysRev.38.834.
Article6. Giap H, Giap B. 2012; Historical perspective and evolution of charged particle beam therapy. Transl Cancer Res. 1:127–136.7. Particle Therapy Co-Operative Group. 2020. Facilties in operation. Particle Therapy Co-Operative Group;Taipei: Available from: https://www.ptcog.ch . cited 2020 May 13.8. Kim JY. 2012. Korea's first proton therapy center. Proton Therapy Today;Ilsan: Available from: http://www.proton-therapy-today.com/koreas-first-proton-therapy-center/ . cited 2020 May 14.9. Shin D, Yoon M, Kwak J, Shin J, Lee SB, Park SY, et al. 2009; Secondary neutron doses for several beam configurations for proton therapy. Int J Radiat Oncol Biol Phys. 74:260–265. DOI: 10.1016/j.ijrobp.2008.10.090. PMID: 19362245.
Article10. Jeong H, Rah JE, Hwang UJ, Yoo SH, Min BJ, Lee SY, et al. 2011; Estimation of the secondary cancer risk induced by diagnostic imaging radiation during proton therapy. J Radiol Prot. 31:477–487. DOI: 10.1088/0952-4746/31/4/007. PMID: 22089084.
Article11. Li X, Liu G, Janssens G, De Wilde O, Bossier V, Lerot X, et al. 2019; The first prototype of spot-scanning proton arc treatment delivery. Radiother Oncol. 137:130–136. DOI: 10.1016/j.radonc.2019.04.032. PMID: 31100606.
Article12. Ding X, Li X, Zhang JM, Kabolizadeh P, Stevens C, Yan D. 2016; Spot-Scanning Proton Arc (SPArc) therapy: the first robust and delivery-efficient spot-scanning proton arc therapy. Int J Radiat Oncol Biol Phys. 96:1107–1116. DOI: 10.1016/j.ijrobp.2016.08.049. PMID: 27869083.
Article13. Wilson JD, Hammond EM, Higgins GS, Petersson K. 2020; Ultra-high dose rate (FLASH) radiotherapy: silver bullet or fool's gold? Front Oncol. 9:1563. DOI: 10.3389/fonc.2019.01563. PMID: 32010633.
Article14. Patriarca A, Fouillade C, Auger M, Martin F, Pouzoulet F, Nauraye C, et al. 2018; Experimental set-up for FLASH proton irradiation of small animals using a clinical system. Int J Radiat Oncol Biol Phys. 102:619–626. DOI: 10.1016/j.ijrobp.2018.06.403. PMID: 30017793.
Article15. Beyreuther E, Brand M, Hans S, Hideghéty K, Karsch L, Leßmann E, et al. 2019; Feasibility of proton FLASH effect tested by zebrafish embryo irradiation. Radiother Oncol. 139:46–50. DOI: 10.1016/j.radonc.2019.06.024. PMID: 31266652.
Article16. Diffenderfer ES, Verginadis II, Kim MM, Shoniyozov K, Velalopoulou A, Goia D, et al. 2020; Design, implementation, and in vivo validation of a novel proton FLASH radiation therapy system. Int J Radiat Oncol Biol Phys. 106:440–448. DOI: 10.1016/j.ijrobp.2019.10.049. PMID: 31928642.17. Paganetti H. 2012; Range uncertainties in proton therapy and the role of Monte Carlo simulations. Phys Med Biol. 57:R99–R117. DOI: 10.1088/0031-9155/57/11/R99. PMID: 22571913. PMCID: PMC3374500.
Article18. Handrack J, Tessonnier T, Chen W, Liebl J, Debus J, Bauer J, et al. 2017; Sensitivity of post treatment positron emission tomography/computed tomography to detect inter-fractional range variations in scanned ion beam therapy. Acta Oncol. 56:1451–1458. DOI: 10.1080/0284186X.2017.1348628. PMID: 28918686.
Article19. Kurz C, Bauer J, Unholtz D, Richter D, Herfarth K, Debus J, et al. 2016; Initial clinical evaluation of PET-based ion beam therapy monitoring under consideration of organ motion. Med Phys. 43:975–982. DOI: 10.1118/1.4940356. PMID: 26843257.
Article20. Min CH, Kim CH, Youn MY, Kim JW. 2006; Prompt gamma measurements for locating the dose falloff region in the proton therapy. Appl Phys Lett. 89:183517. DOI: 10.1063/1.2378561.
Article21. Gensheimer MF, Yock TI, Liebsch NJ, Sharp GC, Paganetti H, Madan N, et al. 2010; In vivo proton beam range verification using spine MRI changes. Int J Radiat Oncol Biol Phys. 78:268–275. DOI: 10.1016/j.ijrobp.2009.11.060. PMID: 20472369.
Article22. Arjomandy B, Taylor P, Ainsley C, Safai S, Sahoo N, Pankuch M, et al. 2019; AAPM task group 224: comprehensive proton therapy machine quality assurance. Med Phys. 46:e678–e705. DOI: 10.1002/mp.13622. PMID: 31125441.
Article23. Schneider U, Pemler P, Besserer J, Pedroni E, Lomax A, Kaser-Hotz B. 2005; Patient specific optimization of the relation between CT-hounsfield units and proton stopping power with proton radiography. Med Phys. 32:195–199. DOI: 10.1118/1.1833041. PMID: 15719970.
Article24. Jo K, Kim MY, Jeong JH, Jeang EH, Kim H, Park S, et al. 2015; A practical experience of dose modeling for proton pencil beam scanning in KNCC. J Korean Phys Soc. 67:108–115. DOI: 10.3938/jkps.67.108.
Article25. Kim DW, Lim YK, Shin J, Ahn S, Shin MY, Lee SB, et al. 2009; A dose verification method for proton therapy by using a plastic scintillation plate. J Korean Phys Soc. 55:702–708. DOI: 10.3938/jkps.55.702.26. Cho S, Lee N, Song S, Son J, Kim H, Jeong JH, et al. 2018; Toward a novel dosimetry system using acrylic disk radiation sensor for proton pencil beam scanning. Med Phys. 45:5277–5282. DOI: 10.1002/mp.13149. PMID: 30133716.
Article27. Shin J, Kim D, Lim YK, Ahn S, Shin D, Yoon MG, et al. 2010; Monte Carlo modeling and simulation of a passive treatment proton beam delivery system using a modulation wheel. J Korean Phys Soc. 56:153–163. DOI: 10.3938/jkps.56.153.28. Kim DH, Kang YN, Suh TS, Shin J, Kim JW, Yoo SH, et al. 2012; Monte Carlo modeling and validation of a proton treatment nozzle by using the Geant4 toolkit. J Korean Phys Soc. 61:1125–1130. DOI: 10.3938/jkps.61.1125.
Article29. Shin WG, Testa M, Kim HS, Jeong JH, Lee SB, Kim YJ, et al. 2017; Independent dose verification system with Monte Carlo simulations using TOPAS for passive scattering proton therapy at the National Cancer Center in Korea. Phys Med Biol. 62:7598–7616. DOI: 10.1088/1361-6560/aa8663. PMID: 28809759.
Article30. Lee SH, Cho S, You SH, Shin D, Park SY, Lee SB, et al. 2012; Evaluation of radioactivity induced by patient-specific devices in proton therapy. J Korean Phys Soc. 60:125–128. DOI: 10.3938/jkps.60.125.
Article31. Lim YK, Kwak J, Kim DW, Shin D, Yoon M, Park S, et al. 2009; Microscopic gold particle-based fiducial markers for proton therapy of prostate cancer. Int J Radiat Oncol Biol Phys. 74:1609–1616. DOI: 10.1016/j.ijrobp.2009.02.076. PMID: 19616746.
Article32. Kwak J, Shin J, Kim JS, Park SY, Shin D, Yoon M, et al. 2010; Dosimetric influence of implanted gold markers in proton therapy for prostate cancer. Korean J Med Phys. 21:291–297.33. Sánchez-Parcerisa D, López-Aguirre M, Dolcet Llerena A, Udías JM. 2019; MultiRBE: Treatment planning for protons with selective radiobiological effectiveness. Med Phys. 46:4276–4284. DOI: 10.1002/mp.13718. PMID: 31310683.34. Park S, Jeong C, Kang DY, Shin JI, Cho S, Park JH, et al. 2013; Proton-radiography-based quality assurance of proton range compensator. Phys Med Biol. 58:6511–6523. DOI: 10.1088/0031-9155/58/18/6511. PMID: 24002543.
Article35. Kim DW, Lim YK, Ahn SH, Shin J, Shin D, Yoon M, et al. 2011; Prediction of output factor, range, and spread-out Bragg peak for proton therapy. Med Dosim. 36:145–152. DOI: 10.1016/j.meddos.2010.02.006. PMID: 20599372.
Article