Korean Circ J.
2020 Oct;50(10):940-948. 10.4070/kcj.2020.0131.
Two-Sample Mendelian Randomization Study of Lipid levels and Ischemic Heart Disease
- Affiliations
-
- 1Department of Epidemiology and Health Promotion, Institute for Health Promotion, Graduate School of Public Health, Yonsei University, Seoul, Korea
- 2Health Insurance Policy Research Institute, National Health Insurance Service, Wonju, Korea
- 3Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2507012
- DOI: http://doi.org/10.4070/kcj.2020.0131
Abstract
- Background and Objectives
Associations between blood lipids and risk of ischemic heart disease (IHD) have been reported in observational studies. However, due to confounding and reverse causation, observational studies are influenced by bias, thus their results show inconsistency in the effects of lipid levels on IHD. In this study, we evaluate whether lipid levels have an effect on the risk of IHD in a Korean population.
Methods
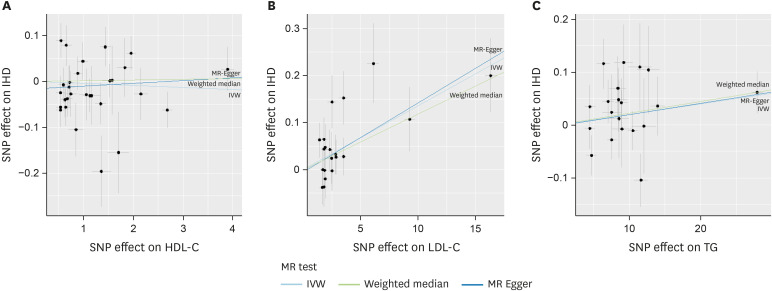
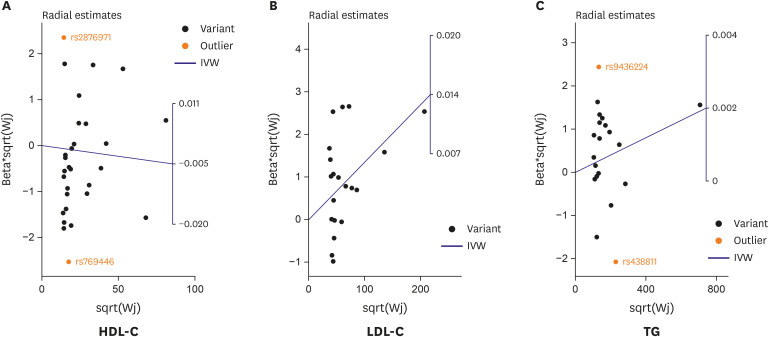
A 2-sample Mendelian randomization (MR) study, using the genetic variants associated with lipid levels as the instrumental variables was performed. Genetic variants significantly associated with lipid concentrations were obtained from the Korean Genome and Epidemiology Study (n=35,000), and the same variants on IHD were obtained from the Korean Cancer Prevention Study-II (n=13,855). Inverse variance weighting (IVW), weighted median, and MR-Egger approaches were used to assess the causal association between lipid levels and IHD. Radial MR methods were applied to remove outliers subject to pleiotropic bias.
Results
Causal association between low-density lipoprotein-cholesterol (LDL-C) and IHD was observed in the IVW method (odds ratio, 1.013; 95% confidence interval, 1.007–1.109). However, high-density lipoprotein-cholesterol (HDL-C) and triglyceride (TG) did not show causal association with IHD. In the Radial MR analysis of the relationship between HDL-C, TG and IHD, outliers were detected. Interestingly, after removing the outliers, a causal association between TG and IHD was found.
Conclusions
High levels LDL-C and TG were causally associated with increased IHD risk in a Korean population, these results are potentially useful as evidence of a significant causal relationship.
Figure
Cited by 3 articles
-
Lipid and Ischemic Heart Disease Revisited: Mendelian Randomization Analysis
Jidong Sung
Korean Circ J. 2020;50(10):949-950. doi: 10.4070/kcj.2020.0328.Role of Genetics in Preventive Cardiology: Focused on Dyslipidemia
Sang-Hak Lee
Korean Circ J. 2021;51(11):899-907. doi: 10.4070/kcj.2021.0239.Another Reason to Cut Down on Alcohol?
Hyeon Chang Kim
Korean Circ J. 2022;52(3):231-232. doi: 10.4070/kcj.2021.0419.
Reference
-
1. Tarchalski J, Guzik P, Wysocki H. Correlation between the extent of coronary atherosclerosis and lipid profile. Mol Cell Biochem. 2003; 246:25–30. PMID: 12841339.
Article2. Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017; 38:2459–2472. PMID: 28444290.
Article3. Di Angelantonio E, Sarwar N, Perry P, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009; 302:1993–2000. PMID: 19903920.
Article4. McBride P. Triglycerides and risk for coronary artery disease. Curr Atheroscler Rep. 2008; 10:386–390. PMID: 18706279.
Article5. Sheehan NA, Didelez V, Burton PR, Tobin MD. Mendelian randomisation and causal inference in observational epidemiology. PLoS Med. 2008; 5:e177. PMID: 18752343.
Article6. Linsel-Nitschke P, Götz A, Erdmann J, et al. Lifelong reduction of LDL-cholesterol related to a common variant in the LDL-receptor gene decreases the risk of coronary artery disease--a Mendelian Randomisation study. PLoS One. 2008; 3:e2986. PMID: 18714375.
Article7. Voight BF, Peloso GM, Orho-Melander M, et al. Plasma HDL cholesterol and risk of myocardial infarction: a Mendelian randomisation study. Lancet. 2012; 380:572–580. PMID: 22607825.8. Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013; 61:427–436. PMID: 23265341.
Article9. Burgess S, Freitag DF, Khan H, Gorman DN, Thompson SG. Using multivariable Mendelian randomization to disentangle the causal effects of lipid fractions. PLoS One. 2014; 9:e108891. PMID: 25302496.
Article10. Shah S, Casas JP, Drenos F, et al. Causal relevance of blood lipid fractions in the development of carotid atherosclerosis: Mendelian randomization analysis. Circ Cardiovasc Genet. 2013; 6:63–72. PMID: 23275344.11. Holmes MV, Asselbergs FW, Palmer TM, et al. Mendelian randomization of blood lipids for coronary heart disease. Eur Heart J. 2015; 36:539–550. PMID: 24474739.12. Elosua R, Sayols-Baixeras S. The genetics of ischemic heart disease: from current knowledge to clinical implications. Rev Esp Cardiol (Engl Ed). 2017; 70:754–762. PMID: 28623161.
Article13. Lawlor DA. Commentary: Two-sample Mendelian randomization: opportunities and challenges. Int J Epidemiol. 2016; 45:908–915. PMID: 27427429.
Article14. Kim Y, Han BG; KoGES group. Cohort profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017; 46:1350. PMID: 28938752.
Article15. Jee YH, Emberson J, Jung KJ, et al. Cohort profile: The Korean Cancer Prevention Study-II (KCPS-II) Biobank. Int J Epidemiol. 2018; 47:385–386f. PMID: 29186422.
Article16. Kimm H, Yun JE, Lee SH, Jang Y, Jee SH. Validity of the diagnosis of acute myocardial infarction in Korean national medical health insurance claims data: the Korean heart study (1). Korean Circ J. 2012; 42:10–15. PMID: 22363378.
Article17. Didelez Y, Sheehan N. Mendelian randomization as an instrumental variable approach to causal inference. Stat Methods Med Res. 2007; 16:309–314. PMID: 17715159.
Article18. Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016; 40:304–314. PMID: 27061298.
Article19. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015; 44:512–525. PMID: 26050253.
Article20. Hemani G, Zheng J, Elsworth B, et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife. 2018; 7:e34408. PMID: 29846171.21. Bowden J, Spiller W, Del Greco M F, et al. Improving the visualization, interpretation and analysis of two-sample summary data Mendelian randomization via the Radial plot and Radial regression. Int J Epidemiol. 2018; 47:1264–1278. PMID: 29961852.
Article22. Navar AM. The evolving story of triglycerides and coronary heart disease risk. JAMA. 2019; 321:347–349. PMID: 30694301.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lipid and Ischemic Heart Disease Revisited: Mendelian Randomization Analysis
- Bilirubin and risk of ischemic heart disease in Korea: a two-sample Mendelian randomization study
- Genetically Mediated Lipid Metabolism and Risk of Insulin Resistance: Insights from Mendelian Randomization Studies
- Mendelian Randomization Analysis in Observational Epidemiology
- No association between genetically predicted C-reactive protein levels and colorectal cancer survival in Korean: two-sample Mendelian randomization analysis