Ann Surg Treat Res.
2020 Oct;99(4):221-229. 10.4174/astr.2020.99.4.221.
Impacts on outcomes and management of preoperative magnetic resonance cholangiopancreatography in patients scheduled for laparoscopic cholecystectomy: for whom it should be considered?
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2506653
- DOI: http://doi.org/10.4174/astr.2020.99.4.221
Abstract
- Purpose
We evaluated the impact of preoperative magnetic resonance cholangiopancreatography (MRCP) on patient outcomes, and found which patients should be considered for MRCP before cholecystectomy.
Methods
We performed retrospective analysis of 2,072 patients that underwent cholecystectomy for benign gallbladder disease from January 2014 to June 2017. Patients were grouped as CT only group (n = 737) and MRCP group (n = 1,335), including both CT and MRCP (n = 1,292) or MRCP only (n = 43). The main outcome measure was associated with complications after cholecystectomy, and the secondary outcomes were hospital stay, readmission, and events that could impact patient management due to addition of MRCP.
Results
There were no statistical differences in occurrence of intraoperative or postoperative complications or readmission rate between the 2 groups. Hospital stay was about 0.6 days longer in the MRCP group. However, MRCP group was more susceptible to complications due to underlying patient demographics (older age, higher frequency of diabetes, and higher level of the inflammatory markers). MRCP diagnosed common bile duct (CBD) stones in 6.5% of patients (84/1,292) without CBD stones in CT, and bile duct anomalies were identified in 41 patients (3.2%). Elevated γ-GT was the only independent factor for additional detection of CBD stones (adjusted odds ratio [OR], 2.89; P = 0.029) and subsequent biliary procedures (adjusted OR, 3.34; P = 0.018) when additional MRCP was performed.
Conclusion
MRCP is valuable for identification of bile duct variation and CBD stones. Preoperative MRCP can be considered, particularly in patients with elevated γ-GT, for proper preoperative management and avoidance of complications.
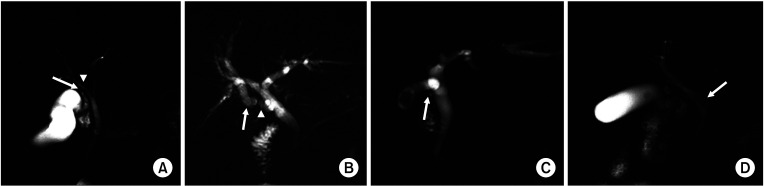
Figure
Reference
-
1. Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: liver, biliary tract, and pancreas. Gastroenterology. 2009; 136:1134–1144. PMID: 19245868.2. Russo MW, Wei JT, Thiny MT, Gangarosa LM, Brown A, Ringel Y, et al. Digestive and liver diseases statistics, 2004. Gastroenterology. 2004; 126:1448–1453. PMID: 15131804.3. Ryoo I, Lee JM, Park HS, Han JK, Choi BI. Preoperative assessment of longitudinal extent of bile duct cancers using MDCT with multiplanar reconstruction and minimum intensity projections: comparison with MR cholangiography. Eur J Radiol. 2012; 81:2020–2026. PMID: 21715117.4. Denecke T, Degutyte E, Stelter L, Lehmkuhl L, Valencia R, Lopez-Hänninen E, et al. Minimum intensity projections of the biliary system using 16-channel multidetector computed tomography in patients with biliary obstruction: comparison with MRCP. Eur Radiol. 2006; 16:1719–1726. PMID: 16514467.5. Griffin N, Wastle ML, Dunn WK, Ryder SD, Beckingham IJ. Magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in the diagnosis of choledocholithiasis. Eur J Gastroenterol Hepatol. 2003; 15:809–813. PMID: 12811312.6. Ausch C, Hochwarter G, Taher M, Holzer B, Rosen HR, Urban M, Sebesta C, et al. Improving the safety of laparoscopic cholecystectomy: the routine use of preoperative magnetic resonance cholangiography. Surg Endosc. 2005; 19:574–580. PMID: 15759179.7. Zhang C, Yin M, Liu Q. The guidance impact of preoperative magnetic resonance cholangiopancreatography on laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2015; 25:720–723. PMID: 26262763.8. Bahram M, Gaballa G. The value of pre-operative magnetic resonance cholangiopancreatography (MRCP) in management of patients with gall stones. Int J Surg. 2010; 8:342–345. PMID: 20450989.9. Jendresen MB, Thorbøll JE, Adamsen S, Nielsen H, Grønvall S, Hart-Hansen O. Preoperative routine magnetic resonance cholangiopancreatography before laparoscopic cholecystectomy: a prospective study. Eur J Surg. 2002; 168:690–694. PMID: 15362577.10. Nebiker CA, Baierlein SA, Beck S, von Flüe M, Ackermann C, Peterli R. Is routine MR cholangiopancreatography (MRCP) justified prior to cholecystectomy? Langenbecks Arch Surg. 2009; 394:1005–1010. PMID: 19084990.11. Qiu Y, Yang Z, Li Z, Zhang W, Xue D. Is preoperative MRCP necessary for patients with gallstones? An analysis of the factors related to missed diagnosis of choledocholithiasis by preoperative ultrasound. BMC Gastroenterol. 2015; 15:158. PMID: 26577949.12. Shaw MJ, Dorsher PJ, Vennes JA. Cystic duct anatomy: an endoscopic perspective. Am J Gastroenterol. 1993; 88:2102–2106. PMID: 8249981.13. Mortelé KJ, Rocha TC, Streeter JL, Taylor AJ. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006; 26:715–731. PMID: 16702450.14. Ording AG, Sørensen HT. Concepts of comorbidities, multiple morbidities, complications, and their clinical epidemiologic analogs. Clin Epidemiol. 2013; 5:199–203. PMID: 23861599.15. Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009; 7:357–363. PMID: 19597174.16. Murphy MM, Ng SC, Simons JP, Csikesz NG, Shah SA, Tseng JF. Predictors of major complications after laparoscopic cholecystectomy: surgeon, hospital, or patient? J Am Coll Surg. 2010; 211:73–80. PMID: 20610252.17. Strömberg J, Sandblom G. Impact of comorbidity and prescription drugs on haemorrhage in cholecystectomy. World J Surg. 2017; 41:1985–1992. PMID: 28265728.18. Inoue K, Ueno T, Douchi D, Shima K, Goto S, Takahashi M, et al. Risk factors for difficulty of laparoscopic cholecystectomy in grade II acute cholecystitis according to the Tokyo guidelines 2013. BMC Surg. 2017; 17:114. PMID: 29183352.19. Kim MS, Kwon HJ, Park HW, Park JY, Chung EC, Park HJ, et al. Preoperative prediction model for conversion of laparoscopic to open cholecystectomy in patient with acute cholecystitis: based on clinical, laboratory, and CT parameters. J Comput Assist Tomogr. 2014; 38:727–732. PMID: 24887577.20. McMahon AJ, Fischbacher CM, Frame SH, MacLeod MC. Impact of laparoscopic cholecystectomy: a population-based study. Lancet. 2000; 356:1632–1637. PMID: 11089821.21. Lee EK, Park E, Oh WO, Shin NM. Comparison of the outcomes of robotic cholecystectomy and laparoscopic cholecystectomy. Ann Surg Treat Res. 2017; 93:27–34. PMID: 28706888.22. Richard F, Boustany M, Britt LD. Accuracy of magnetic resonance cholangiopancreatography for diagnosing stones in the common bile duct in patients with abnormal intraoperative cholangiograms. Am J Surg. 2013; 205:371–373. PMID: 23518180.23. Scaffidi MG, Luigiano C, Consolo P, Pellicano R, Giacobbe G, Gaeta M, et al. Magnetic resonance cholangio-pancreatography versus endoscopic retrograde cholangio-pancreatography in the diagnosis of common bile duct stones: a prospective comparative study. Minerva Med. 2009; 100:341–348. PMID: 19910887.24. Sonnenberg A, Enestvedt BK, Bakis G. Management of suspected choledocholithiasis: a decision analysis for choosing the optimal imaging modality. Dig Dis Sci. 2016; 61:603–609. PMID: 26399621.25. Möller M, Gustafsson U, Rasmussen F, Persson G, Thorell A. Natural course vs interventions to clear common bile duct stones: data from the Swedish Registry for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks). JAMA Surg. 2014; 149:1008–1013. PMID: 25133326.26. McPartland KJ, Pomposelli JJ. Iatrogenic biliary injuries: classification, identification, and management. Surg Clin North Am. 2008; 88:1329–1343. PMID: 18992598.27. Sicklick JK, Camp MS, Lillemoe KD, Melton GB, Yeo CJ, Campbell KA, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg. 2005; 241:786–792. PMID: 15849514.28. Epelboym I, Winner M, Allendorf JD. MRCP is not a cost-effective strategy in the management of silent common bile duct stones. J Gastrointest Surg. 2013; 17:863–871. PMID: 23515912.29. ASGE Standards of Practice Committee. Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010; 71:1–9. PMID: 20105473.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Value of Preoperative Magnetic Resonance Cholangiopancreatography (MRCP) in Patients Who will be Performed Laparoscopic Cholecystectomy
- The Management of Common Bile Duct Stones
- Relationship between the risk of bile duct injury during laparoscopic cholecystectomy and the types of preoperative magnetic resonance cholangiopancreatiocography (MRCP)
- Indications and Timing of ERCP and Cholecystectomy for Biliary Pancreatitis
- Impact of scheduled laparoscopic cholecystectomy in patients with acute cholecystitis, following percutaneous transhepatic gallbladder drainage