Ann Clin Microbiol.
2020 Sep;23(3):177-184. 10.5145/ACM.2020.23.3.1.
Performance Evaluation of STANDARD F Strep A Ag FIA for Diagnosis of Group A Streptococcal Pharyngitis
- Affiliations
-
- 1Department of Laboratory Medicine, Daewoo General Hospital, Geoje, Korea
- 2Department of Pediatrics, Changwon Fatima Hospital, Changwon, Korea
- 3Department of Laboratory Medicine, Gyeongsang National University Changwon Hospital, Changwon, Korea
- 4Gyeongsang National University, Gyeongsang Institute of Health Sciences, Jinju, Korea
- KMID: 2506554
- DOI: http://doi.org/10.5145/ACM.2020.23.3.1
Abstract
- Background
Pharyngitis is one of the most common conditions encountered in primary health care facilities. Accurate differentiation of group A streptococcus (GAS) infection from viral infection is difficult. The STANDARD F Strep A Ag FIA (SD BIOSENSOR, Korea) is a rapid antigen detection test (RADT) that has been recently developed for diagnosing GAS pharyngitis. In this study, we evaluated the diagnostic performance of the STANDARD F Strep A Ag FIA and compared the results between the RADT and conventional throat culture.
Methods
Throat swab samples were obtained from a total of 372 children presenting pharyngitis symptoms in five pediatric clinics in Changwon, Korea from July 2018 to October 2019. A comparative study between STANDARD F Strep A Ag FIA and Sofia Strep A FIA (Quidel, USA) was performed. Two throat swabs were taken simultaneously from each patient for RADT. The third throat swab was stored in a transport tube containing Stuart's transport medium for culture. Performance and kappa index of STANDARD F Strep A Ag FIA were evaluated.
Results
GAS infection was detected in 29.3% (109/372) patients, using the STANDARD F Strep A Ag FIA. The sensitivity, specificity, positive predictive value, and negative predictive value were 95.0%, 95.2%, 88.1%, and 98.1%, respectively. The STANDARD F Strep A Ag FIA showed an excellent concordance rate of 96.5% and a kappa value of 0.89 compared to Sofia Strep A FIA.
Conclusion
The STANDARD F Strep A Ag FIA demonstrated an excellent performance along with Sofia Strep A FIA for the diagnosis of GAS pharyngitis.
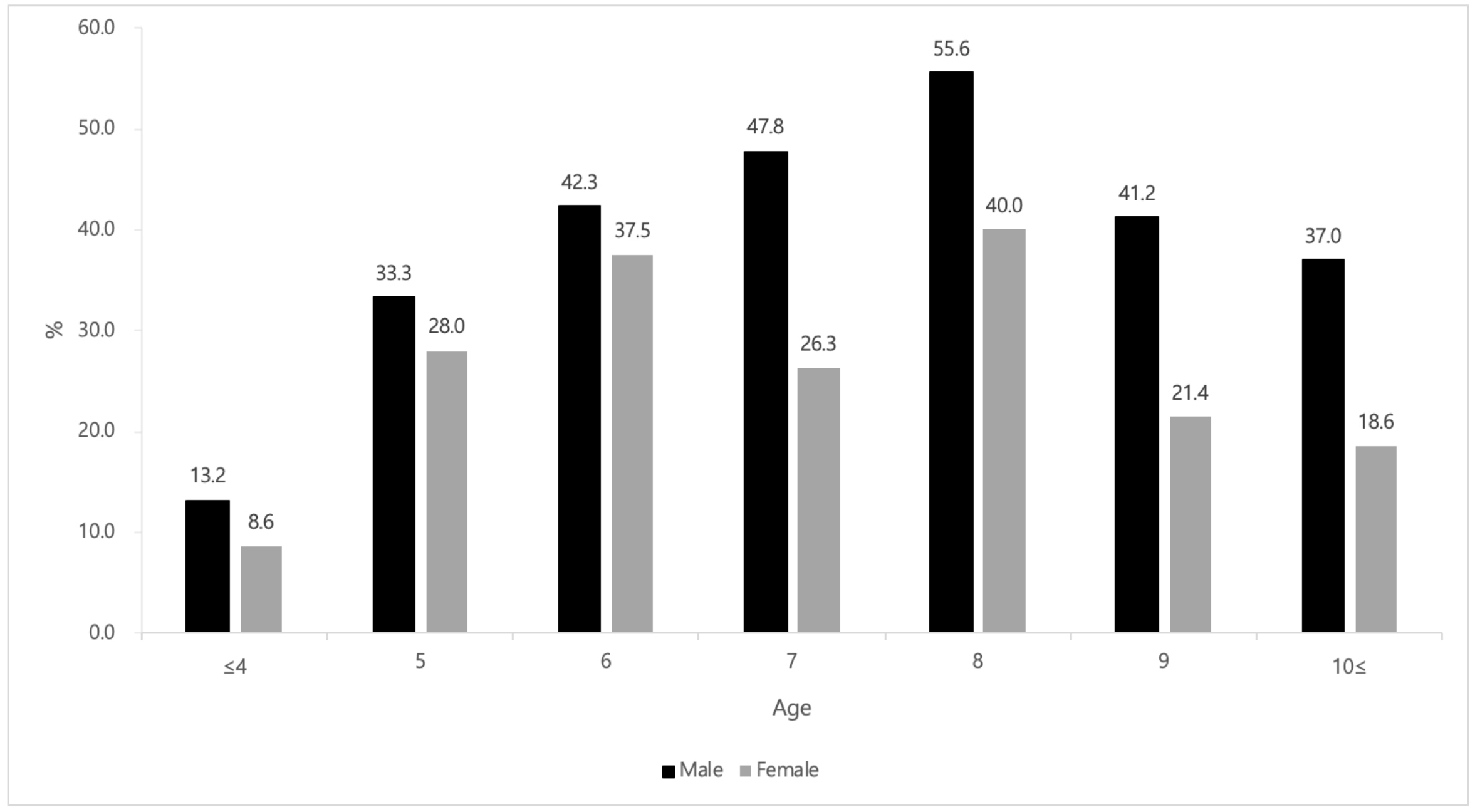
Figure
Reference
-
1. Lean WL, Arnup S, Danchin M, Steer AC. Rapid diagnostic tests for group A streptococcal pharyngitis: a meta-analysis. Pediatrics 2014;134:771-81.2. Wessels MR. Clinical practice. Streptococcal pharyngitis. N Engl J Med 2011;364:648-55.3. Cohen JF, Bertille N, Cohen R, Chalumeau M. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Cochrane Database Syst Rev 2016;7:CD010502.4. Shaikh N, Swaminathan N, Hooper EG. Accuracy and precision of the signs and symptoms of streptococcal pharyngitis in children: a systematic review. J Pediatr 2012;160:487-93.5. Vazquez MN and Sanders JE. Diagnosis and management of group A streptococcal pharyngitis and associated complications. Pediatr Emerg Med Pract 2017;14:1-20.6. Ebell MH, Smith MA, Barry HC, Ives K, Carey M. The rational clinical examination. Does this patient have strep throat? JAMA 2000;284:2912-8.7. Kalra MG, Higgins KE, Perez ED. Common questions about streptococcal pharyngitis. Am Fam Physician 2016;94:24-31.8. Del Mar CB, Glasziou PP, Spinks AB. Antibiotics for sore throat. Cochrane Database Syst Rev 2006;4:CD000023.9. Bisno AL. Acute pharyngitis. N Engl J Med 2001;344:205-11.10. Gieseker KE, Mackenzie T, Roe MH, Todd JK. Comparison of two rapid Streptococcus pyogenes diagnostic tests with a rigorous culture standard. Pediatr Infect Dis J 2002;21:922-7.11. Gerber MA and Shulman ST. Rapid diagnosis of pharyngitis caused by group A streptococci. Clin Microbiol Rev 2004;17:571-80.12. Fox JW, Marcon MJ, Bonsu BK. Diagnosis of streptococcal pharyngitis by detection of Streptococcus pyogenes in posterior pharyngeal versus oral cavity specimens. J Clin Microbiol 2006;44:2593-4.13. Kim HN, Kim J, Jang WS, Nam J, Lim CS. Performance evaluation of three rapid antigen tests for the diagnosis of group A Streptococci. BMJ Open 2019;9:e025438.14. Ma SH, Choi WH, Park HW, Kim SJ. Evaluation of the SD bioline strep A ultra test in relation with number of colony forming units and color intensity. Ann Lab Med 2019;39:31-5.15. Kose E, Sirin Kose S, Akca D, Yildiz K, Elmas C, Baris M, et al. The effect of rapid antigen detection test on antibiotic prescription decision of clinicians and reducing antibiotic costs in children with acute pharyngitis. J Trop Pediatr 2016;62:308-15.16. Edmonson MB and Farwell KR. Relationship between the clinical likelihood of group a streptococcal pharyngitis and the sensitivity of a rapid antigen-detection test in a pediatric practice. Pediatrics 2005;115:280-5.17. Randel A. IDSA updates guideline for managing group A streptococcal pharyngitis. Am Fam Physician 2013;88:338-40.18. Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 2012;55:1279-82.19. Kucuk O, Bicer S, Giray T, Col D, Erdag GC, Gurol Y, et al. Validity of rapid antigen detection testing in group A beta-hemolytic streptococcal tonsillopharyngitis. Indian J Pediatr 2014;81:138-42.20. Penney C, Porter R, O'Brien M, Daley P. Operator influence on blinded diagnostic accuracy of point-of-care antigen testing for group A streptococcal pharyngitis. Can J Infect Dis Med Microbiol 2016;2016:1710561.21. Lacroix L, Cherkaoui A, Schaller D, Manzano S, Galetto-Lacour A, Pfeifer U, et al. Improved diagnostic performance of an immunofluorescence-based rapid antigen detection test for group A streptococci in children with pharyngitis. Pediatr Infect Dis J 2018;37:206-11.22. Vakkila J, Koskinen JO, Brandt A, Muotiala A, Liukko V, Soittu S, et al. Detection of group A streptococcus from pharyngeal swab samples by bacterial culture is challenged by a vovel mariPOC point-of-care test. J Clin Microbiol 2015;53:2079-83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of SD Bioline Strep A for Rapid Antigen Testing in Elementary Schoolchildren
- Clinical Manifestations of Group A Streptococcal Pharyngitis and Comparison of Usefulness of Two Rapid Streptococcal Antigen Tests
- Clinical Availability of Rapid Strep Test in Children with Group A Streptococcal Pharyngotonsilitis
- Evaluation of the SD Bioline Strep A Ultra Test in Relation With Number of Colony Forming Units and Color Intensity
- Comparative Evaluation of the STANDARD F Influenza A/B FIA Test with the Sofia Influenza A+B FIA and SD BIOLINE Influenza Ag A/B/A(H1N1) tests for Influenza A Virus Detection