Korean J Orthod.
2020 Sep;50(5):324-335. 10.4041/kjod.2020.50.5.324.
Positional changes in the mandibular proximal segment after intraoral vertical ramus osteotomy: Surgery-first approach versus conventional approach
- Affiliations
-
- 1Department of Dental Education, Yonsei University College of Dentistry, Seoul, Korea
- 2Department of Statistics, University of Seoul, Seoul, Korea
- 3Department of Oral and Maxillofacial Surgery, Ewha Womans University Medical Center, Seoul, Korea
- 4Department of Oral and Maxillofacial Surgery, Oral Science Research Center, Yonsei University College of Dentistry, Seoul, Korea
- 5Department of Orthodontics, Yonsei University College of Dentistry, Seoul, Korea
- KMID: 2506467
- DOI: http://doi.org/10.4041/kjod.2020.50.5.324
Abstract
Objective
To compare postoperative positional changes in the mandibular proximal segment between the conventional orthognathic surgery (CS) and the surgery-first approach (SF) using intraoral vertical ramus osteotomy (IVRO) in patients with Class III malocclusion.
Methods
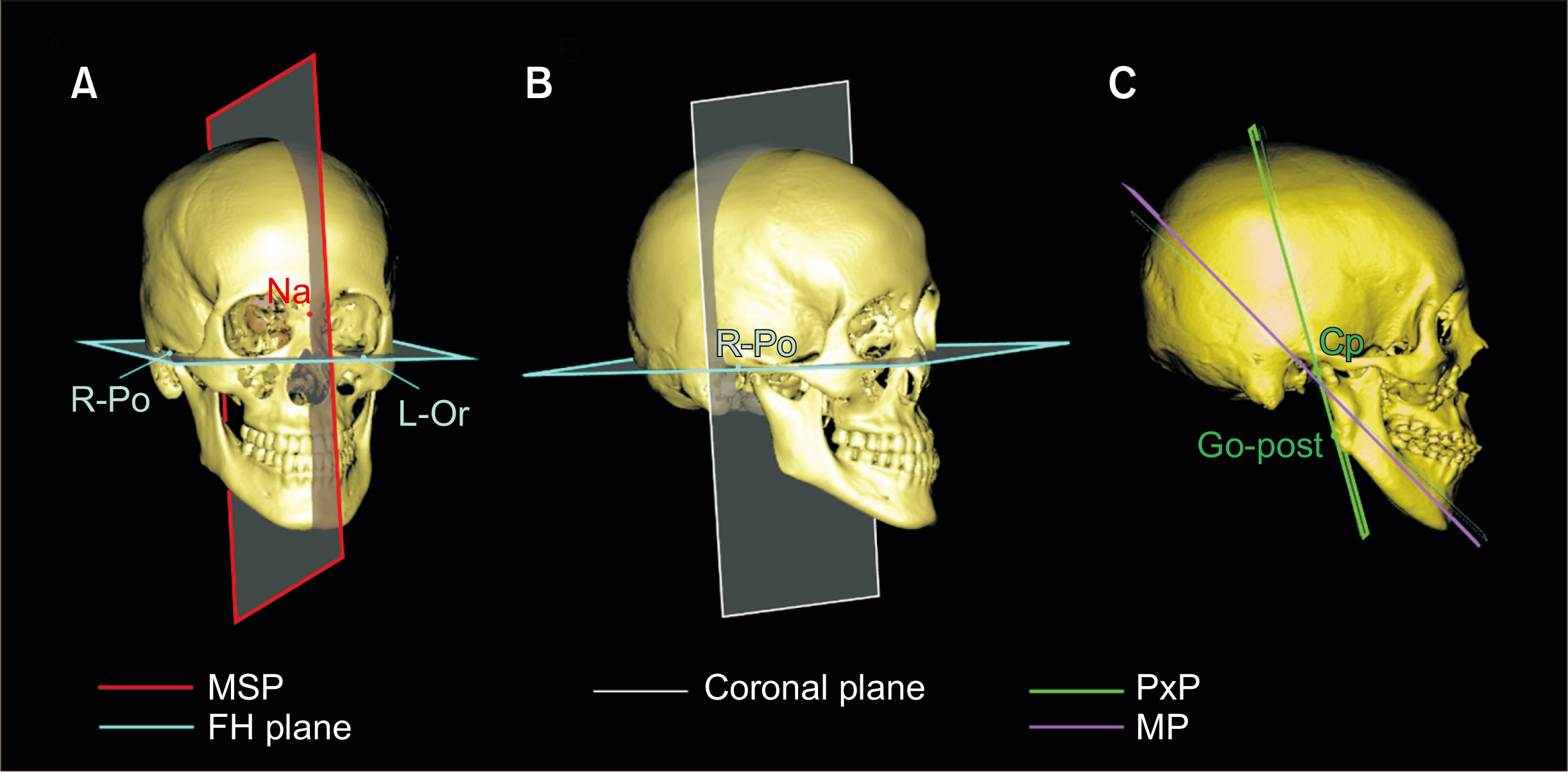
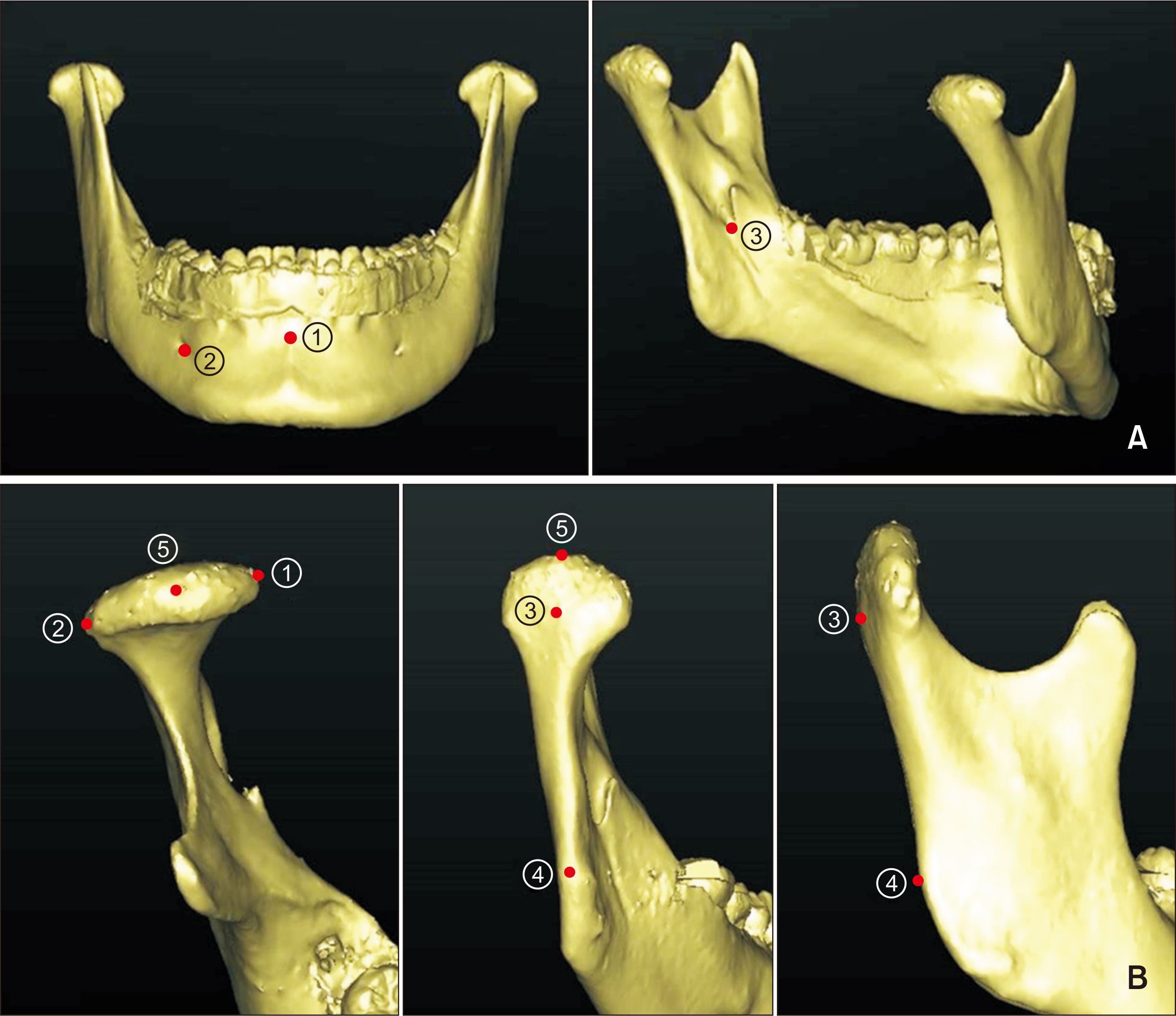
Thirty-eight patients with skeletal Class III malocclusion who underwent bimaxillary surgery were divided into two groups according to the use of preoperative orthodontic treatment: CS group (n = 18) and SF group (n = 20). Skeletal changes in both groups were measured using computed tomography before (T0), 2 days after (T1), and 1 year after (T2) the surgery. Three-dimensional (3D) angular changes in the mandibular proximal segment, condylar position, and maxillomandibular landmarks were assessed.
Results
The mean amounts of mandibular setback and maxillary posterior impaction were similar in both groups. At T2, the posterior portion of the mandible moved upward in both groups. In the SF group, the anterior portion of the mandible moved upward by a mean distance of 0.9 ± 1.0 mm, which was statistically significant (p < 0.001). There were significant between-group differences in occlusal changes (p < 0.001) as well as in overjet and overbite. However, there were no significant between-group differences in proximal segment variables. Conclusions: Despite postoperative occlusal changes, positional changes in the mandibular proximal segment and the position of the condyles were similar between CS and SF, which suggested that SF using IVRO achieved satisfactory postoperative stability. If active physiotherapy is conducted, the proximal segment can be adapted in the physiological position regardless of the occlusal changes.
Keyword
Figure
Cited by 1 articles
-
Incidence and management of condylar resorption after orthognathic surgery: An overview
Selene Barone, Giorgio Cosentini, Francesco Bennardo, Alessandro Antonelli, Amerigo Giudice
Korean J Orthod. 2022;52(1):29-41. doi: 10.4041/kjod.2022.52.1.29.
Reference
-
1. Jacobs JD, Sinclair PM. 1983; Principles of orthodontic mechanics in orthognathic surgery cases. Am J Orthod. 84:399–407. DOI: 10.1016/0002-9416(93)90003-P. PMID: 6579841.
Article2. Nagasaka H, Sugawara J, Kawamura H, Nanda R. 2009; "Surgery first" skeletal Class III correction using the Skeletal Anchorage System. J Clin Orthod. 43:97–105.3. Kim CS, Lee SC, Kyung HM, Park HS, Kwon TG. 2014; Stability of mandibular setback surgery with and without presurgical orthodontics. J Oral Maxillofac Surg. 72:779–87. DOI: 10.1016/j.joms.2013.09.033. PMID: 24268965.
Article4. Nihara J, Takeyama M, Takayama Y, Mutoh Y, Saito I. 2013; Postoperative changes in mandibular prognathism surgically treated by intraoral vertical ramus osteotomy. Int J Oral Maxillofac Surg. 42:62–70. DOI: 10.1016/j.ijom.2012.06.024. PMID: 22858240.
Article5. Ohba S, Nakao N, Awara K, Tobita T, Minamizato T, Kawasaki T, et al. 2015; The three-dimensional assessment of dynamic changes of the proximal segments after intraoral vertical ramus osteotomy. Cranio. 33:276–84. DOI: 10.1179/2151090314Y.0000000023. PMID: 26715130.
Article6. Jung HD, Jung YS, Park JH, Park HS. 2012; Recovery pattern of mandibular movement by active physical therapy after bilateral transoral vertical ramus osteotomy. J Oral Maxillofac Surg. 70:e431–7. DOI: 10.1016/j.joms.2012.02.033. PMID: 22698299.
Article7. Bell WH, Yamaguchi Y, Poor MR. 1990; Treatment of temporomandibular joint dysfunction by intraoral vertical ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 5:9–27. DOI: 10.1016/s0901-5027(99)80721-8. PMID: 2373914.8. Kim JY, Jung HD, Kim SY, Park HS, Jung YS. 2014; Postoperative stability for surgery-first approach using intraoral vertical ramus osteotomy: 12 month follow-up. Br J Oral Maxillofac Surg. 52:539–44. DOI: 10.1016/j.bjoms.2014.03.011. PMID: 24746355.
Article9. Ko EW, Lin SC, Chen YR, Huang CS. 2013; Skeletal and dental variables related to the stability of orthognathic surgery in skeletal Class III malocclusion with a surgery-first approach. J Oral Maxillofac Surg. 71:e215–23. DOI: 10.1016/j.joms.2012.12.025. PMID: 23455415.
Article10. Choi SH, Hwang CJ, Baik HS, Jung YS, Lee KJ. 2016; Stability of pre-orthodontic orthognathic surgery using intraoral vertical ramus osteotomy versus conventional treatment. J Oral Maxillofac Surg. 74:610–9. DOI: 10.1016/j.joms.2015.07.012. PMID: 26259691.
Article11. Jung HD, Jung YS, Kim SY, Kim DW, Park HS. 2013; Postoperative stability following bilateral intraoral vertical ramus osteotomy based on amount of setback. Br J Oral Maxillofac Surg. 51:822–6. DOI: 10.1016/j.bjoms.2013.02.001. PMID: 23484677.
Article12. Park SH, Yu HS, Kim KD, Lee KJ, Baik HS. 2006; A proposal for a new analysis of craniofacial morphology by 3-dimensional computed tomography. Am J Orthod Dentofacial Orthop. 129:600.e23–34. DOI: 10.1016/j.ajodo.2005.11.032. PMID: 16679198.
Article13. Kang SH, Kim MK, You TK, Lee JY. 2015; Modification of planned postoperative occlusion in orthognathic surgery, based on computer-aided design/computer-aided manufacturing-engineered preoperative surgical simulation. J Oral Maxillofac Surg. 73:134–51. DOI: 10.1016/j.joms.2014.07.021. PMID: 25315304.
Article14. Uribe F, Janakiraman N, Shafer D, Nanda R. 2013; Three-dimensional cone-beam computed tomography-based virtual treatment planning and fabrication of a surgical splint for asymmetric patients: surgery first approach. Am J Orthod Dentofacial Orthop. 144:748–58. DOI: 10.1016/j.ajodo.2012.10.029. PMID: 24182591.
Article15. Baek SH, Ahn HW, Kwon YH, Choi JY. 2010; Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: evaluation of surgical movement and postoperative orthodontic treatment. J Craniofac Surg. 21:332–8. DOI: 10.1097/SCS.0b013e3181cf5fd4. PMID: 20186090.16. Lee J, Kim YI, Hwang DS, Kim KB, Park SB. 2014; Effect of occlusal vertical dimension changes on postsurgical skeletal changes in a surgery-first approach for skeletal Class III deformities. Am J Orthod Dentofacial Orthop. 146:612–9. DOI: 10.1016/j.ajodo.2014.07.024. PMID: 25439212.
Article17. Alsafadi AS, Alabdullah MM, Saltaji H, Abdo A, Youssef M. 2016; Effect of molar intrusion with temporary anchorage devices in patients with anterior open bite: a systematic review. Prog Orthod. 17:9. DOI: 10.1186/s40510-016-0122-4. PMID: 26980200. PMCID: PMC4803715.
Article18. Arimoto S, Hasegawa T, Kaneko K, Tateishi C, Furudoi S, Shibuya Y, et al. 2013; Observation of osseous healing after intraoral vertical ramus osteotomy: focus on computed tomography values. J Oral Maxillofac Surg. 71:1602.e1–10. DOI: 10.1016/j.joms.2013.02.021. PMID: 23611606.
Article19. Ghali GE. 2000; Intraoral vertical ramus osteotomy as the preferred treatment for mandibular prognathism. J Oral Maxillofac Surg. 58:313–5. DOI: 10.1016/S0278-2391(00)90063-6. PMID: 10716115.
Article20. Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. 2001; Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restorative Dent. 21:9–19. PMID: 11829041.21. Wilcko MT, Wilcko WM, Pulver JJ, Bissada NF, Bouquot JE. 2009; Accelerated osteogenic orthodontics technique: a 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg. 67:2149–59. DOI: 10.1016/j.joms.2009.04.095. PMID: 19761908.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Skeletal relapse pattern after sagittal split ramus osteotomy of mandibular prognathic patient
- Morphologic and positional change of the proximal segments after intraoralvertical ramus osteotomy of the mandibular prognathism on submentovertex cephalogram
- Changes in facial width according to the ostectomy level of the proximal bone segment in intraoral vertical ramus osteotomy for mandibular prognathism
- Unilateral intraoral vertical ramus osteotomy and sagittal split ramus osteotomy for the treatment of asymmetric mandibles
- Surgical correction of maxillofacial deformity with fibrous-osseous lesion of mandible using the intraoral vertical ramus osteotomy