Clin Exp Otorhinolaryngol.
2020 Aug;13(3):215-224. 10.21053/ceo.2020.01053.
Surgical Algorithm for Obstructive Sleep Apnea: An Update
- Affiliations
-
- 1Division of Sleep Surgery, Department of Otolaryngology-Head and Neck Surgery, Stanford University School of Medicine, Stanford Hospital and Clinics, Stanford, CA, USA
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2504915
- DOI: http://doi.org/10.21053/ceo.2020.01053
Abstract
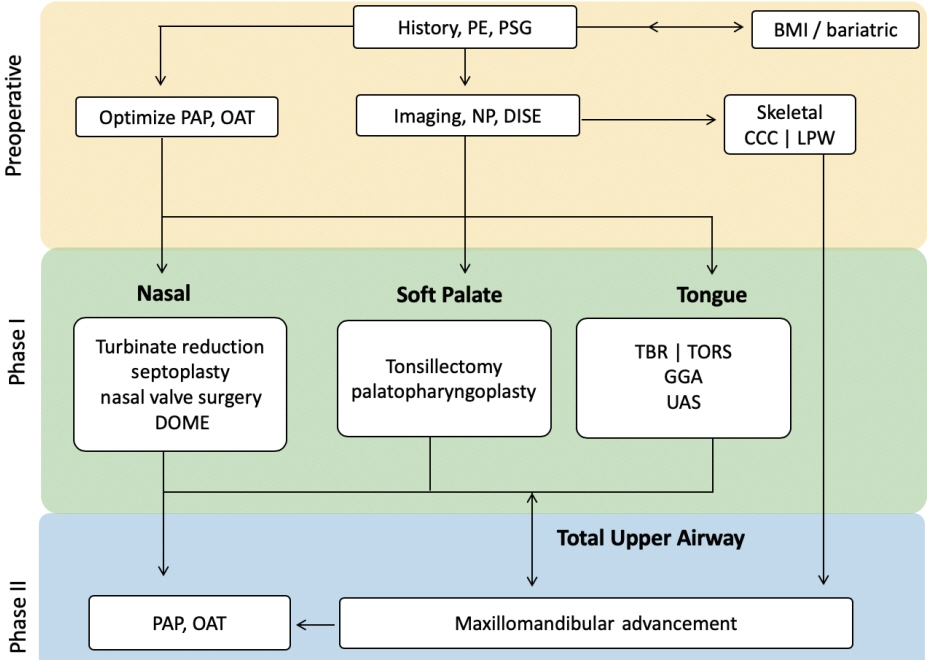
- Sleep surgery is part of a continuum of care for obstructive sleep apnea (OSA) that involves medical, pharmacologic, and behavioral therapy. Upper airway surgery for OSA can significantly improve stability by way of modulating the critical negative closing pressure. This is the same mechanism of action as positive airway pressure or oral appliance therapy. The updated surgical algorithm in this review adds precision in three areas: patient selection, identification of previously unaddressed anatomic phenotypes with associated treatment modality, and improved techniques of previously established procedures. While the original Riley and Powell phase 1 and 2 approach to sleep surgery has focused on individual surgical success rate, this algorithm strives for an overall treatment success with multi-modal and patient-centric treatments.
Keyword
Figure
Cited by 1 articles
-
Effect of Obstructive Sleep Apnea on Immunity in Cases of Chronic Rhinosinusitis With Nasal Polyps
Dong-Kyu Kim, Byeong Chan Lee, Ki Joon Park, Gil Myeong Son
Clin Exp Otorhinolaryngol. 2021;14(4):390-398. doi: 10.21053/ceo.2020.02250.
Reference
-
1. Riley RW, Powell NB, Guilleminault C. Obstructive sleep apnea syndrome: a surgical protocol for dynamic upper airway reconstruction. J Oral Maxillofac Surg. 1993; Jul. 51(7):742–9.
Article2. Powell N, Riley R, Guilleminault C, Troell R. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep. 1996; Sep. 19(7):593–9.
Article3. Riley RW, Powell NB, Guilleminault C, Nino-Murcia G. Maxillary, mandibular, and hyoid advancement: an alternative to tracheostomy in obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 1986; Jun. 94(5):584–8.
Article4. Riley RW, Powell NB, Guilleminault C. Maxillofacial surgery and nasal CPAP: a comparison of treatment for obstructive sleep apnea syndrome. Chest. 1990; Dec. 98(6):1421–5.5. Decker M, Yamauchi M, Strohl KP. Keep the airway open and let the brain sleep. Am J Respir Crit Care Med. 2014; Dec. 190(11):1207–9.
Article6. Liu SY, Awad M, Riley R, Capasso R. The role of the revised Stanford protocol in today’s precision medicine. Sleep Med Clin. 2019; Mar. 14(1):99–107.
Article7. Liu SY, Powell NB, Riley RW. Algorithm for multilevel treatment: the Riley, Powell, and Liu Stanford experience. In : Friedman M, Jacobowitz O, editors. Sleep apnea and snoring: surgical and non-surgical therapy. 2nd ed. Edinburgh: Elsevier;2020. p. 104–9.8. Zozula R, Rosen R. Compliance with continuous positive airway pressure therapy: assessing and improving treatment outcomes. Curr Opin Pulm Med. 2001; Nov. 7(6):391–8.
Article9. Chervin RD, Theut S, Bassetti C, Aldrich MS. Compliance with nasal CPAP can be improved by simple interventions. Sleep. 1997; Apr. 20(4):284–9.
Article10. Torre C, Capasso R, Zaghi S, Williams R, Liu SY. High incidence of posterior nasal cavity obstruction in obstructive sleep apnea patients. Sleep Sci Pract. 2017; Mar. 1(1):8.
Article11. Camacho M, Zaghi S, Certal V, Abdullatif J, Means C, Acevedo J, et al. Inferior turbinate classification system, grades 1 to 4: development and validation study. Laryngoscope. 2015; Feb. 125(2):296–302.
Article12. Terris DJ, Hanasono MM, Liu YC. Reliability of the Muller maneuver and its association with sleep-disordered breathing. Laryngoscope. 2000; Nov. 110(11):1819–23.
Article13. Huynh NT, Morton PD, Rompre PH, Papadakis A, Remise C. Associations between sleep-disordered breathing symptoms and facial and dental morphometry, assessed with screening examinations. Am J Orthod Dentofacial Orthop. 2011; Dec. 140(6):762–70.
Article14. Kim JH, Guilleminault C. The nasomaxillary complex, the mandible, and sleep-disordered breathing. Sleep Breath. 2011; May. 15(2):185–93.
Article15. Williams R, Patel V, Chen YF, Tangbumrungtham N, Thamboo A, Most SP, et al. The upper airway nasal complex: structural contribution to persistent nasal obstruction. Otolaryngol Head Neck Surg. 2019; Jul. 161(1):171–7.
Article16. Goldberg AN. Obstructive sleep apnea: decision making and treatment algorithm. In : Friedman M, Jacobowitz O, editors. Sleep apnea and snoring E-Book: surgical and non-surgical therapy. Philadelphia (PA): Elsevier;2008. p. 45.17. Punjabi NM, Newman AB, Young TB, Resnick HE, Sanders MH. Sleep-disordered breathing and cardiovascular disease: an outcomebased definition of hypopneas. Am J Respir Crit Care Med. 2008; May. 177(10):1150–5.18. Kendzerska T, Gershon AS, Hawker G, Leung RS, Tomlinson G. Obstructive sleep apnea and risk of cardiovascular events and allcause mortality: a decade-long historical cohort study. PLoS Med. 2014; Feb. 11(2):e1001599.
Article19. Aurora RN, Swartz R, Punjabi NM. Misclassification of OSA severity with automated scoring of home sleep recordings. Chest. 2015; Mar. 147(3):719–27.
Article20. Kapoor M, Greenough G. Home sleep tests for Obstructive Sleep Apnea (OSA). J Am Board Fam Med. 2015; Jul-Aug. 28(4):504–9.
Article21. Nerfeldt P, Aoki F, Friberg D. Polygraphy vs. polysomnography: missing OSAs in symptomatic snorers: a reminder for clinicians. Sleep Breath. 2014; May. 18(2):297–303.22. Watson NF. Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. J Clin Sleep Med. 2016; Aug. 12(8):1075–7.
Article23. Scannone A, Tosta M, Suarez A, Otero L. Cephalometric and dental measures as diagnostic tools for the obstructive sleep apnea. J Sleep Disor Treat Care. 2017; Jan. 6(4):
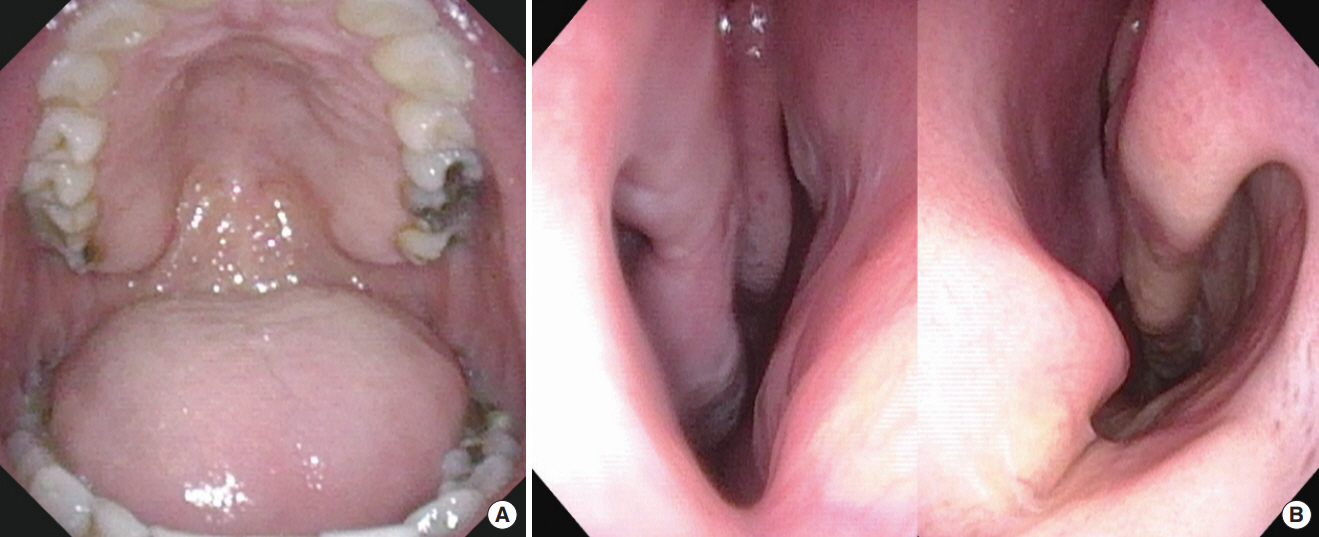
Article24. Torre C, Zaghi S, Camacho M, Capasso R, Liu SY. Hypopharyngeal evaluation in obstructive sleep apnea with awake flexible laryngoscopy: validation and updates to Cormack-Lehane and modified Cormack-Lehane scoring systems. Clin Otolaryngol. 2018; Jun. 43(3):823–7.
Article25. Kim JW, Kim J, Kim T, Lee K, Kim S, Bae M. Extraction of acoustic biomarkers from PSG to detect OSA. Sleep Med. 2017; Dec. 40:e160.
Article26. Kim WY, Hong SN, Yang SK, Nam KJ, Lim KH, Hwang SJ, et al. The effect of body position on airway patency in obstructive sleep apnea: CT imaging analysis. Sleep Breath. 2019; Sep. 23(3):911–6.
Article27. Huon LK, Liu SY, Shih TT, Chen YJ, Lo MT, Wang PC. Dynamic upper airway collapse observed from sleep MRI: BMI-matched severe and mild OSA patients. Eur Arch Otorhinolaryngol. 2016; Nov. 273(11):4021–6.
Article28. Soose RJ. Novel surgical approaches for the treatment of obstructive sleep apnea. Sleep Med Clin. 2016; Jun. 11(2):189–202.
Article29. Kent DT, Rogers R, Soose RJ. Drug-induced sedation endoscopy in the evaluation of OSA patients with incomplete oral appliance therapy response. Otolaryngol Head Neck Surg. 2015; Aug. 153(2):302–7.
Article30. Vroegop AV, Vanderveken OM, Verbraecken JA. Drug-induced sleep endoscopy: evaluation of a selection tool for treatment modalities for obstructive sleep apnea. Respiration. 2020; 99(5):451–7.
Article31. Glen JB. The development of ‘Diprifusor’: a TCI system for propofol. Anaesthesia. 1998; Apr. 53 Suppl 1:13–21.
Article32. Hillman DR, Walsh JH, Maddison KJ, Platt PR, Kirkness JP, Noffsinger WJ, et al. Evolution of changes in upper airway collapsibility during slow induction of anesthesia with propofol. Anesthesiology. 2009; Jul. 111(1):63–71.
Article33. Eastwood PR, Platt PR, Shepherd K, Maddison K, Hillman DR. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology. 2005; Sep. 103(3):470–7.
Article34. Chattopadhyay U, Mallik S, Ghosh S, Bhattacharya S, Bisai S, Biswas H. Comparison between propofol and dexmedetomidine on depth of anesthesia: a prospective randomized trial. J Anaesthesiol Clin Pharmacol. 2014; Oct. 30(4):550–4.
Article35. Charakorn N, Kezirian EJ. Drug-induced sleep endoscopy. Otolaryngol Clin North Am. 2016; Dec. 49(6):1359–72.
Article36. Croft CB, Pringle M. Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci. 1991; Oct. 16(5):504–9.37. Kezirian EJ, Hohenhorst W, de Vries N. Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol. 2011; Aug. 268(8):1233–6.
Article38. Friedman M, Ibrahim H, Bass L. Clinical staging for sleep-disordered breathing. Otolaryngol Head Neck Surg. 2002; Jul. 127(1):13–21.
Article39. Iwanaga K, Hasegawa K, Shibata N, Kawakatsu K, Akita Y, Suzuki K, et al. Endoscopic examination of obstructive sleep apnea syndrome patients during drug-induced sleep. Acta Otolaryngol Suppl. 2003; (550):36–40.
Article40. Vicini C, de Vito A, Benazzo M, Frassineti S, Campanini A, Frasconi P, et al. The nose oropharynx hypopharynx and larynx (NOHL) classification: a new system of diagnostic standardized examination for OSAHS patients. Eur Arch Otorhinolaryngol. 2012; Apr. 269(4):1297–300.
Article41. Vroegop AV, Vanderveken OM, Boudewyns AN, Scholman J, Saldien V, Wouters K, et al. Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope. 2014; Mar. 124(3):797–802.
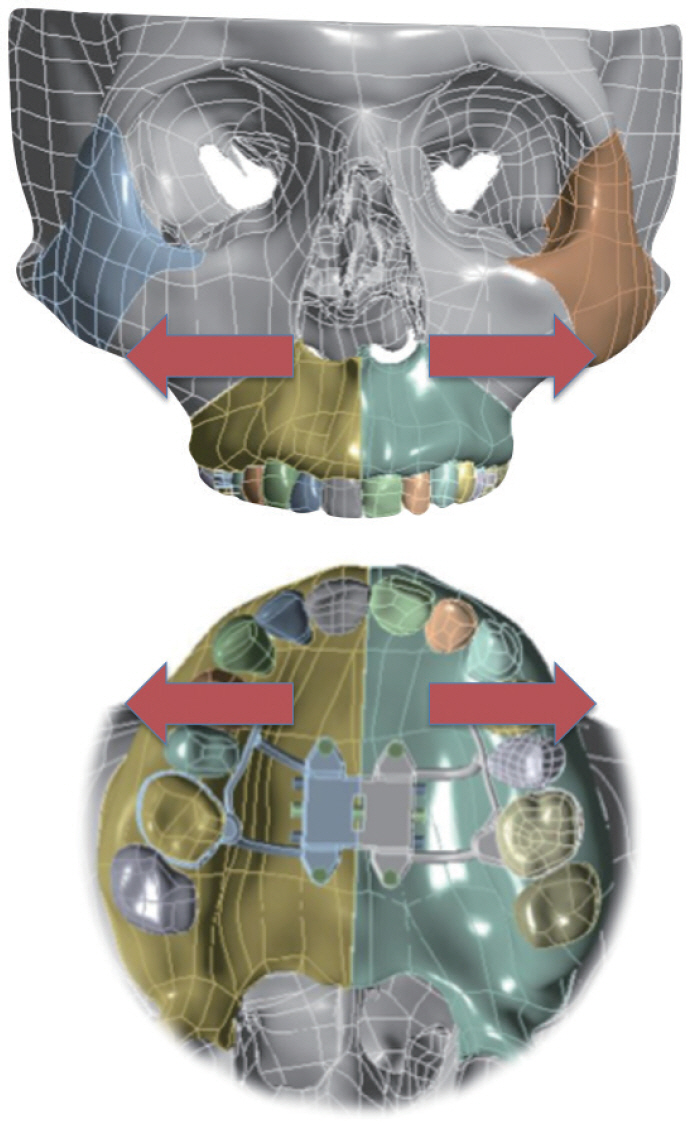
Article42. Ravesloot MJ, de Vries N. One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation. Laryngoscope. 2011; Dec. 121(12):2710–6.
Article43. Vanderveken OM, Maurer JT, Hohenhorst W, Hamans E, Lin HS, Vroegop AV, et al. Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J Clin Sleep Med. 2013; May. 9(5):433–8.
Article44. Zhang P, Ye J, Pan C, Sun N, Kang D. The role of obstruction length and height in predicting outcome of velopharyngeal surgery. Otolaryngol Head Neck Surg. 2015; Jul. 153(1):144–9.
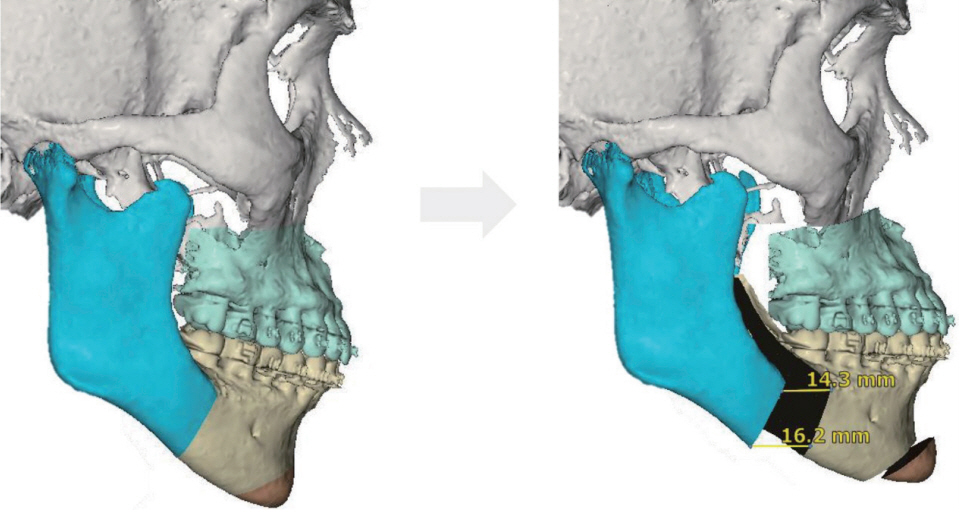
Article45. Liu SY, Huon LK, Iwasaki T, Yoon A, Riley R, Powell N, et al. Efficacy of maxillomandibular advancement examined with drug-induced sleep endoscopy and computational fluid dynamics airflow modeling. Otolaryngol Head Neck Surg. 2016; Jan. 154(1):189–95.
Article46. Lavie P. Rediscovering the importance of nasal breathing in sleep or, shut your mouth and save your sleep. J Laryngol Otol. 1987; Jun. 101(6):558–63.
Article47. Busaba NY. The nose in snoring and obstructive sleep apnea. Curr Opin Otolaryngol Head Neck Surg. 1999; Feb. 7(1):11.
Article48. Olsen KD, Kern EB, Westbrook PR. Sleep and breathing disturbance secondary to nasal obstruction. Otolaryngol Head Neck Surg. 1981; Sep-Oct. 89(5):804–10.
Article49. Cole P, Haight JS. Mechanisms of nasal obstruction in sleep. Laryngoscope. 1984; Dec. 94(12 Pt 1):1557–9.
Article50. Verse T, Maurer JT, Pirsig W. Effect of nasal surgery on sleep-related breathing disorders. Laryngoscope. 2002; Jan. 112(1):64–8.
Article51. Camacho M, Riaz M, Capasso R, Ruoff CM, Guilleminault C, Kushida CA, et al. The effect of nasal surgery on continuous positive airway pressure device use and therapeutic treatment pressures: a systematic review and meta-analysis. Sleep. 2015; Feb. 38(2):279–86.
Article52. Trindade SH, Tagliarini JV, Elly I, Trindade K, Weber SA. Nasal septoplasty in patients with obstructive sleep apnea syndrome: effects on polysomnographic parameters. J Sleep Med Disord. 2017; Jun. 4(2):1077.53. Elhabashy M, Abdelfatah A, Abdelaziz A, Omar H, Abdelwhab S. Effectiveness of septoplasty with or without inferior turbinate reduction in patients with obstructive sleep apnea. Eur Respir J. 2019; 54(Suppl 63):PA4163.
Article54. Friedman M, Salapatas AM. Algorithm for multilevel treatment: Friedman experience. In : Friedman M, Jacobowitz O, editors. Sleep apnea and snoring: surgical and non-surgical therapy. 2nd ed. Edinburgh: Elsevier;2020. p. 120–6.55. Abdelwahab M, Yoon A, Okland T, Poomkonsarn S, Gouveia C, Liu SY. Impact of distraction osteogenesis maxillary expansion on the internal nasal valve in obstructive sleep apnea. Otolaryngol Head Neck Surg. 2019; Aug. 161(2):362–7.
Article56. Iwasaki T, Yoon A, Guilleminault C, Yamasaki Y, Liu SY. How does distraction osteogenesis maxillary expansion (DOME) reduce severity of obstructive sleep apnea? Sleep Breath. 2020; Mar. 24(1):287–96.
Article57. Liu SY, Guilleminault C, Huon LK, Yoon A. Distraction Osteogenesis Maxillary Expansion (DOME) for adult obstructive sleep apnea patients with high arched palate. Otolaryngol Head Neck Surg. 2017; Aug. 157(2):345–8.
Article58. Yoon A, Guilleminault C, Zaghi S, Liu SY. Distraction Osteogenesis Maxillary Expansion (DOME) for adult obstructive sleep apnea patients with narrow maxilla and nasal floor. Sleep Med. 2020; Jan. 65:172–6.
Article59. Camacho M, Chang ET, Song SA, Abdullatif J, Zaghi S, Pirelli P, et al. Rapid maxillary expansion for pediatric obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope. 2017; Jul. 127(7):1712–9.
Article60. Iwasaki T, Saitoh I, Takemoto Y, Inada E, Kanomi R, Hayasaki H, et al. Improvement of nasal airway ventilation after rapid maxillary expansion evaluated with computational fluid dynamics. Am J Orthod Dentofacial Orthop. 2012; Mar. 141(3):269–78.
Article61. Iwasaki T, Takemoto Y, Inada E, Sato H, Suga H, Saitoh I, et al. The effect of rapid maxillary expansion on pharyngeal airway pressure during inspiration evaluated using computational fluid dynamics. Int J Pediatr Otorhinolaryngol. 2014; Aug. 78(8):1258–64.
Article62. Villa MP, Malagola C, Pagani J, Montesano M, Rizzoli A, Guilleminault C, et al. Rapid maxillary expansion in children with obstructive sleep apnea syndrome: 12-month follow-up. Sleep Med. 2007; Mar. 8(2):128–34.
Article63. Ishman SL, Ishii LE, Gourin CG. Temporal trends in sleep apnea surgery: 1993-2010. Laryngoscope. 2014; 124(5):1251–8.
Article64. Camacho M, Nesbitt NB, Lambert E, Song SA, Chang ET, Liu SY, et al. Laser-assisted uvulopalatoplasty for obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2017; Mar. 40(3):
Article65. Thaler ER, Rassekh CH, Lee JM, Weinstein GS, O’Malley BW Jr. Outcomes for multilevel surgery for sleep apnea: obstructive sleep apnea, transoral robotic surgery, and uvulopalatopharyngoplasty. Laryngoscope. 2016; Jan. 126(1):266–9.
Article66. Lin HC, Friedman M, Chang HW, Gurpinar B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope. 2008; May. 118(5):902–8.
Article67. Li HY. Palatal surgery for obstructive sleep apnea: from ablation to reconstruction. Sleep Med Clin. 2019; Mar. 14(1):51–8.68. Awad M, Gouveia C, Capasso R, Liu SY. Tonsillectomy and pharyngoplasty: tissue-preserving techniques. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):17–22.69. Camacho M, Zaghi S, Piccin O, Certal V. Expansion sphincter pharyngoplasty for obstructive sleep apnea: an update to the recent meta-analysis. Eur Arch Otorhinolaryngol. 2016; Sep. 273(9):2857–8.
Article70. Vicini C, Hendawy E, Campanini A, Eesa M, Bahgat A, AlGhamdi S, et al. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study: “we are on the giant’s shoulders”. Eur Arch Otorhinolaryngol. 2015; Oct. 272(10):3065–70.
Article71. Pang KP, Plaza G, Baptista J PM, O’Connor Reina C, Chan YH, Pang KA, et al. Palate surgery for obstructive sleep apnea: a 17-year meta-analysis. Eur Arch Otorhinolaryngol. 2018; Jul. 275(7):1697–707.
Article72. Hsu YS, Jacobowitz O. Does sleep endoscopy staging pattern correlate with outcome of advanced palatopharyngoplasty for moderate to severe obstructive sleep apnea? J Clin Sleep Med. 2017; Oct. 13(10):1137–44.
Article73. Pang KP, Woodson BT. Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007; Jul. 137(1):110–4.
Article74. Cahali MB, Formigoni GG, Gebrim EM, Miziara ID. Lateral pharyngoplasty versus uvulopalatopharyngoplasty: a clinical, polysomnographic and computed tomography measurement comparison. Sleep. 2004; Aug. 27(5):942–50.
Article75. Woodson BT, Robinson S, Lim HJ. Transpalatal advancement pharyngoplasty outcomes compared with uvulopalatopharygoplasty. Otolaryngol Head Neck Surg. 2005; Aug. 133(2):211–7.
Article76. Jacobowitz O. Algorithm for surgery: palatopharyngoplasty first and foremost. In : Friedman M, Jacobowitz O, editors. Sleep apnea and snoring: surgical and non-surgical therapy. 2nd ed. Edinburgh: Elsevier;2020. p. 99–103.77. Liu SY, Hutz MJ, Poomkonsarn S, Chang CP, Awad M, Capasso R. Palatopharyngoplasty resolves concentric collapse in patients ineligible for upper airway stimulation. Laryngoscope. 2020; Feb. 28. [Epub]. https://doi.org/10.1002/lary.28595.
Article78. Campanini A, Canzi P, de Vito A, Dallan I, Montevecchi F, Vicini C. Awake versus sleep endoscopy: personal experience in 250 OSAHS patients. Acta Otorhinolaryngol Ital. 2010; Apr. 30(2):73–7.79. Friedman M, Soans R, Gurpinar B, Lin HC, Joseph N. Evaluation of submucosal minimally invasive lingual excision technique for treatment of obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2008; Sep. 139(3):378–85.
Article80. Li HY, Lee LA, Kezirian EJ. Coblation endoscopic lingual lightening (CELL) for obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2016; Jan. 273(1):231–6.
Article81. Montevecchi F, Cammaroto G, Meccariello G, Hoff PT, Corso RM, Galletti C, et al. Transoral robotic surgery (TORS): a new tool for high risk tracheostomy decannulation. Acta Otorhinolaryngol Ital. 2017; Feb. 37(1):46–50.
Article82. Cammaroto G, Meccariello G, Costantini M, Stomeo F, Hoff P, Montevecchi F, et al. Trans-oral robotic tongue reduction for OSA: does lingual anatomy influence the surgical outcome? J Clin Sleep Med. 2018; Aug. 14(8):1347–51.
Article83. Camacho M, Certal V, Capasso R. Comprehensive review of surgeries for obstructive sleep apnea syndrome. Braz J Otorhinolaryngol. 2013; Nov-Dec. 79(6):780–8.
Article84. Justin GA, Chang ET, Camacho M, Brietzke SE. Transoral robotic surgery for obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2016; May. 154(5):835–46.85. Vicini C, Montevecchi F, Meccariello G, Cammaroto G. Base of tongue surgery. In : Salman SO, editor. Modern management of obstructive sleep apnea. 1st ed. Cham: Springer;2019. p. 59–68.86. Chan JY, Wong EW, Tsang RK, Holsinger FC, Tong MC, Chiu PW, et al. Early results of a safety and feasibility clinical trial of a novel single-port flexible robot for transoral robotic surgery. Eur Arch Otorhinolaryngol. 2017; Nov. 274(11):3993–6.
Article87. Chan JY, Holsinger FC, Liu S, Sorger JM, Azizian M, Tsang RK. Augmented reality for image guidance in transoral robotic surgery. J Robot Surg. 2020; Aug. 14:579–83.
Article88. Song SA, Chang ET, Certal V, Del Do M, Zaghi S, Liu SY, et al. Genial tubercle advancement and genioplasty for obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope. 2017; Apr. 127(4):984–92.
Article89. Riley RW, Powell NB, Guilleminault C. Obstructive sleep apnea syndrome: a review of 306 consecutively treated surgical patients. Otolaryngol Head Neck Surg. 1993; Feb. 108(2):117–25.
Article90. Liu SY, Huon LK, Zaghi S, Riley R, Torre C. An accurate method of designing and performing individual-specific genioglossus advancement. Otolaryngol Head Neck Surg. 2017; Jan. 156(1):194–7.
Article91. Cheng A. Genioglossus and genioplasty advancement. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):23–8.
Article92. Oliven A, Odeh M, Geitini L, Oliven R, Steinfeld U, Schwartz AR, et al. Effect of coactivation of tongue protrusor and retractor muscles on pharyngeal lumen and airflow in sleep apnea patients. J Appl Physiol (1985). 2007; Nov. 103(5):1662–8.
Article93. Dedhia RC, Strollo PJ, Soose RJ. Upper airway stimulation for obstructive sleep apnea: past, present, and future. Sleep. 2015; Jun. 38(6):899–906.
Article94. Strollo PJ Jr, Soose RJ, Maurer JT, de Vries N, Cornelius J, Froymovich O, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014; Jan. 370(2):139–49.
Article95. Costantino A, Rinaldi V, Moffa A, Luccarelli V, Bressi F, Cassano M, et al. Hypoglossal nerve stimulation long-term clinical outcomes: a systematic review and meta-analysis. Sleep Breath. 2020; Jun. 24(2):399–411.
Article96. Hofauer B, Steffen A, Knopf A, Hasselbacher K, Heiser C. Adherence to upper-airway stimulation in the treatment of OSA. Chest. 2018; Feb. 153(2):574–5.
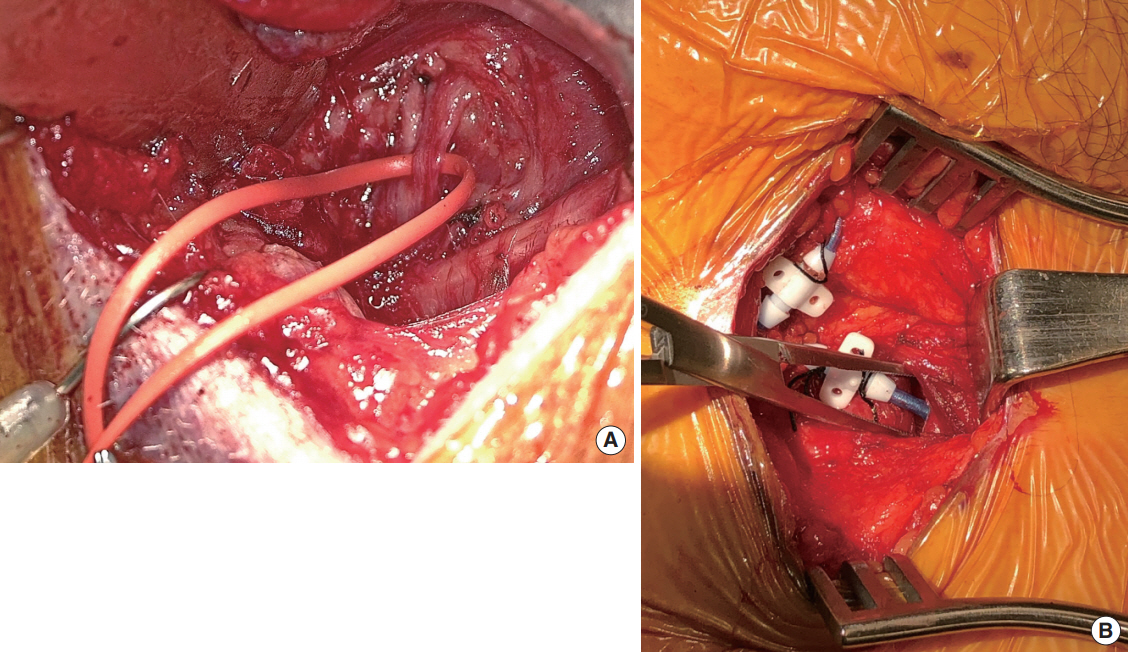
Article97. Bohorquez D, Mahmoud AF, Yu JL, Thaler ER. Upper airway stimulation therapy and sleep architecture in patients with obstructive sleep apnea. Laryngoscope. 2020; Apr. 130(4):1085–9.
Article98. Powell N, Riley RW. A surgical protocol for sleep disordered breathing. Oral Maxillofac Surg Clin North Am. 1995; May. 7(3):345–56.
Article99. Riley RW, Powell NB. Maxillofacial surgery and obstructive sleep apnea syndrome. Otolaryngol Clin North Am. 1990; Aug. 23(4):809–26.100. Riley RW, Powell NB, Guilleminault C. Maxillary, mandibular, and hyoid advancement for treatment of obstructive sleep apnea: a review of 40 patients. J Oral Maxillofac Surg. 1990; Jan. 48(1):20–6.
Article101. Vicini C, Dallan I, Campanini A, de Vito A, Barbanti F, Giorgiomarrano G, et al. Surgery vs ventilation in adult severe obstructive sleep apnea syndrome. Am J Otolaryngol. 2010; Jan-Feb. 31(1):14–20.
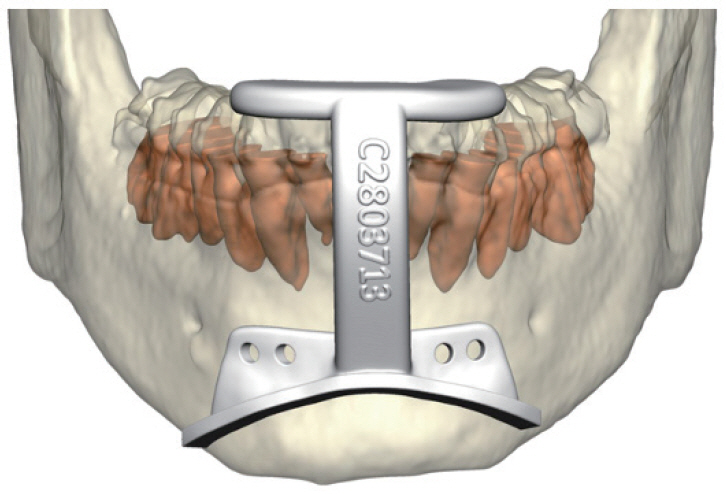
Article102. Camacho M, Liu SY, Certal V, Capasso R, Powell NB, Riley RW. Large maxillomandibular advancements for obstructive sleep apnea: an operative technique evolved over 30 years. J Craniomaxillofac Surg. 2015; Sep. 43(7):1113–8.103. Liu SY, Awad M, Riley RW. Maxillomandibular advancement: contemporary approach at Stanford. Atlas Oral Maxillofac Surg Clin North Am. 2019; Mar. 27(1):29–36.104. Boyd SB. Management of obstructive sleep apnea by maxillomandibular advancement. Oral Maxillofac Surg Clin North Am. 2009; Nov. 21(4):447–57.
Article105. Liu SY, Huon LK, Powell NB, Riley R, Cho HG, Torre C, et al. Lateral pharyngeal wall tension after maxillomandibular advancement for obstructive sleep apnea is a marker for surgical success: observations from drug-induced sleep endoscopy. J Oral Maxillofac Surg. 2015; Aug. 73(8):1575–82.
Article106. Chen YF, Ko EC, Zaghi S, Yoon A, Williams R, Riley R, et al. Optimizing mandibular sagittal split of large maxillomandibular advancements for obstructive sleep apnea: patient and surgical factors. Clin Oral Investig. 2020; Mar. 24(3):1359–67.
Article107. Holty JE, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2010; Oct. 14(5):287–97.
Article108. Zaghi S, Holty JE, Certal V, Abdullatif J, Guilleminault C, Powell NB, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016; Jan. 142(1):58–66.109. Riley RW, Powell NB, Li KK, Troell RJ, Guilleminault C. Surgery and obstructive sleep apnea: long-term clinical outcomes. Otolaryngol Head Neck Surg. 2000; Mar. 122(3):415–21.
Article110. Vigneron A, Tamisier R, Orset E, Pepin JL, Bettega G. Maxillomandibular advancement for obstructive sleep apnea syndrome treatment: long-term results. J Craniomaxillofac Surg. 2017; Feb. 45(2):183–91.
Article111. Boyd SB, Chigurupati R, Cillo JE Jr, Eskes G, Goodday R, Meisami T, et al. Maxillomandibular advancement improves multiple health-related and functional outcomes in patients with obstructive sleep apnea: a multicenter study. J Oral Maxillofac Surg. 2019; Feb. 77(2):352–70.
Article112. Green KK, Kent DT, D’Agostino MA, Hoff PT, Lin HS, Soose RJ, et al. Drug-induced sleep endoscopy and surgical outcomes: a multicenter cohort study. Laryngoscope. 2019; Mar. 129(3):761–70.
Article113. Soares D, Sinawe H, Folbe AJ, Yoo G, Badr S, Rowley JA, et al. Lateral oropharyngeal wall and supraglottic airway collapse associated with failure in sleep apnea surgery. Laryngoscope. 2012; Feb. 122(2):473–9.
Article114. Liu SY, Riley RW. Continuing the original Stanford Sleep Surgery Protocol from upper airway reconstruction to upper airway stimulation: our first successful case. J Oral Maxillofac Surg. 2017; Jul. 75(7):1514–8.
Article