Anesth Pain Med.
2020 Jul;15(3):383-387. 10.17085/apm.20034.
Invisible perforation during an endoscopic procedure of the esophagus under general anesthesia - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Presbyterian Medical Center, Jeonju, Korea
- KMID: 2504903
- DOI: http://doi.org/10.17085/apm.20034
Abstract
- Background
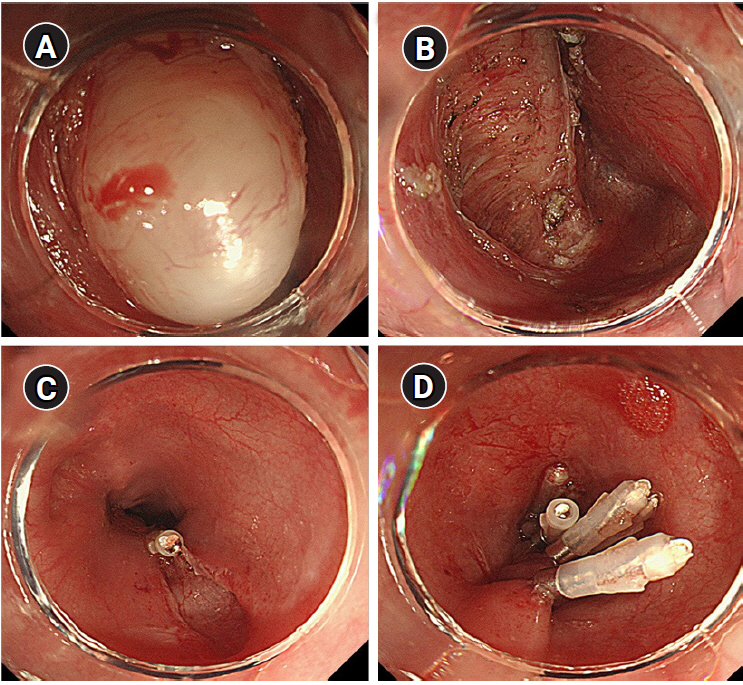
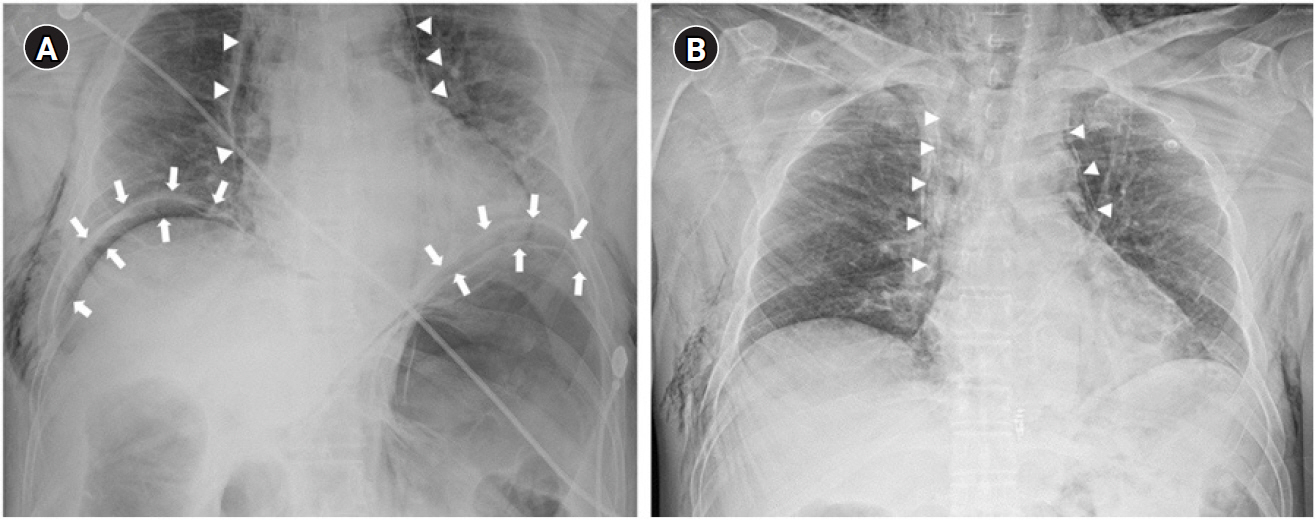
Endoscopic procedures of the esophagus are more complicated than those of other regions of the gastrointestinal tract. They have a relatively long procedure time and high risk of complications, such as perforation and bleeding. Perforations that occur during the procedure can accompany pneumoperitoneum and pneumomediastinum through leakage of insufflation air and cause severe ventilatory impairment. Case: A 58-year-old male patient underwent enucleation of leiomyoma in the esophagus using endoscopy under general anesthesia. Ventilatory impairment occurred 15 min after commencement of the procedure. Subsequently, subcutaneous emphysema and severe abdominal distension were observed. We suggested the possibility of microperforation during the procedure to the endoscopist, and he performed endoscopic clipping around the excision site of leiomyoma.
Conclusions
Providing anesthetic care by anesthesiologists during endoscopic procedures is considered necessary for patient safety. Complications of endoscopic procedures can be detected and managed early without sequelae during anesthetic care.
Figure
Reference
-
1. Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006; 41:929–42.2. Chung IK, Lee JH, Lee SH, Kim SJ, Cho JY, Cho WY, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009; 69:1228–35.3. Kim JJ, Lee JH, Jung HY, Lee GH, Cho JY, Ryu CB, et al. EMR for early gastric cancer in Korea: a multicenter retrospective study. Gastrointest Endosc. 2007; 66:693–700.4. Sasaki T, Tanabe S, Ishido K, Azuma M, Katada C, Higuchi K, et al. Recommended sedation and intraprocedural monitoring for gastric endoscopic submucosal dissection. Dig Endosc. 2013; 25 Suppl 1:79–85.5. Yoo YC, Park CH, Shin S, Park Y, Lee SK, Min KT. A comparison of sedation protocols for gastric endoscopic submucosal dissection: moderate sedation with analgesic supplementation vs analgesia targeted light sedation. Br J Anaesth. 2015; 115:84–8.6. Sasaki T, Tanabe S, Azuma M, Sato A, Naruke A, Ishido K, et al. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection: a randomized prospective phase II clinical trial. Endoscopy. 2012; 44:584–9.7. Yamashita K, Shiwaku H, Ohmiya T, Shimaoka H, Okada H, Nakashima R, et al. Efficacy and safety of endoscopic submucosal dissection under general anesthesia. World J Gastrointest Endosc. 2016; 8:466–71.8. Kim GE, Lee SH, Chung IS, Lee E, Shin HS, Choi JW. Severe respiratory depression precipitated by unrecognized gastric perforation during endoscopic submucosal dissection under deep sedation - a case report -. Anesth Pain Med. 2017; 12:402–7.9. Yagi Kuwata N, Gotoda T, Suzuki S, Mukai S, Itoi T, Moriyasu F. Reasonable decision of anesthesia methods in patients who underwent endoscopic submucosal dissection for superficial esophageal carcinoma: a retrospective analysis in a single Japanese institution. Turk J Gastroenterol. 2016; 27:91–6.10. Bona D, Saino GI, Medda M, Panizzo V, Micheletto G. Cardiac tamponade occurred after endoscopic submucosal dissection: conservative management of the esophagopericardial fistula. Clin Case Rep. 2017; 5:1966–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perforation of a Gastric Tear during Esophageal Endoscopic Submucosal Dissection under General Anesthesia
- The safety of endoscopic esophageal procedures under general anesthesia
- Severe respiratory depression precipitated by unrecognized gastric perforation during endoscopic submucosal dissection under deep sedation: A case report
- Esophageal Perforation with Delayed Detection of a Foreign Body: A Case Report
- Iatrogenic esophageal perforation in a newborn: A case report