Anesth Pain Med.
2017 Oct;12(4):402-407. 10.17085/apm.2017.12.4.402.
Severe respiratory depression precipitated by unrecognized gastric perforation during endoscopic submucosal dissection under deep sedation: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jiwon0715.choi@samsung.com
- KMID: 2405863
- DOI: http://doi.org/10.17085/apm.2017.12.4.402
Abstract
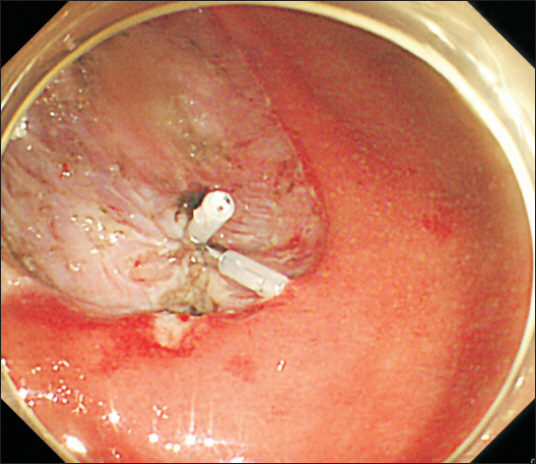
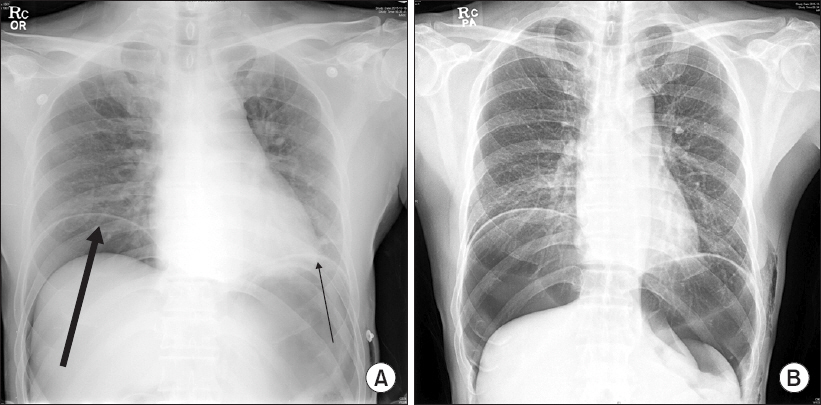
- Endoscopic submucosal dissection (ESD) is widely performed these days as the standard procedure for the treatment of early gastric cancer. During ESD, insertion and rotation of the scope, air insufflation, incision and hemostasis may provoke pain, which commonly requires either general anesthesia or moderate to deep sedation. Deep sedation precludes the need for general anesthesia, and can help endoscopists speed up the procedure compared to light sedation. But, there are risks of respiratory complication. We report a case of respiratory compromise caused by pneumoperitoneum from unrecognized gastric perforation during ESD under deep sedation.
MeSH Terms
Figure
Reference
-
1. Park YM, Cho E, Kang HY, Kim JM. The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer:a systematic review and metaanalysis. Surg Endosc. 2011; 25:2666–77. DOI: 10.1007/s00464-011-1627-z. PMID: 21424201.2. Yurtlu DA, Aslan F, Ayvat P, Isik Y, Karakus N, Ünsal B, et al. Propofol-based sedation versus general anesthesia for endoscopic submucosal dissection. Medicine (Baltimore). 2016; 95:e3680. DOI: 10.1097/MD.0000000000003680. PMID: 27196474. PMCID: PMC4902416.3. Park CH, Shin S, Lee SK, Lee H, Lee YC, Park JC, et al. Assessing the stability and safety of procedure during endoscopic submucosal dissection according to sedation methods:a randomized trial. PLoS One. 2015; 10:e0120529. DOI: 10.1371/journal.pone.0120529. PMID: 25803441. PMCID: PMC4372558.4. Kiriyama S, Gotoda T, Sano H, Oda I, Nishimoto F, Hirashima T, et al. Safe and effective sedation in endoscopic submucosal dissection for early gastric cancer:a randomized comparison between propofol continuous infusion and intermittent midazolam injection. J Gastroenterol. 2010; 45:831–7. DOI: 10.1007/s00535-010-0222-8. PMID: 20228999.5. Park CH, Min JH, Yoo YC, Kim H, Joh DH, Jo JH, et al. Sedation methods can determine performance of endoscopic submucosal dissection in patients with gastric neoplasia. Surg Endosc. 2013; 27:2760–7. DOI: 10.1007/s00464-013-2804-z. PMID: 23389074.6. Yoo YC, Park CH, Shin S, Park Y, Lee SK, Min KT. A comparison of sedation protocols for gastric endoscopic submucosal dissection:moderate sedation with analgesic supplementation vs analgesia targeted light sedation. Br J Anaesth. 2015; 115:84–8. DOI: 10.1093/bja/aeu555. PMID: 25631470.7. Sasaki T, Tanabe S, Azuma M, Sato A, Naruke A, Ishido K, et al. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection:a randomized prospective phase II clinical trial. Endoscopy. 2012; 44:584–9. DOI: 10.1055/s-0032-1306776. PMID: 22638779.8. Yoo JH, Shin SJ, Lee KM, Choi JM, Wi JO, Kim DH, et al. Risk factors for perforations associated with endoscopic submucosal dissection in gastric lesions:emphasis on perforation type. Surg Endosc. 2012; 26:2456–64. DOI: 10.1007/s00464-012-2211-x. PMID: 22398962.9. Angsuwatcharakon P, Rerknimitr R. Endoscopic closure of iatrogenic perforation. Gastrointest Interv. 2016; 5:15–21. DOI: 10.18528/gii150009.10. Lee DW, Jeon SW. Management of complications during gastric endoscopic submucosal dissection. Diagn Ther Endosc. 2012; 2012:624835.11. Symeonidis N, Ballas K, Pavlidis E, Psarras K, Pavlidis T, Sakantamis A. Tension pneumoperitoneum:a rare complication of upper gastrointestinal endoscopy. JSLS. 2012; 16:495–7. DOI: 10.4293/108680812X13462882736655. PMID: 23318083. PMCID: PMC3535805.12. Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013; 5:527–33. DOI: 10.4253/wjge.v5.i11.527. PMID: 24255744. PMCID: PMC3831194.13. Yamashita K, Shiwaku H, Ohmiya T, Shimaoka H, Okada H, Nakashima R, et al. Efficacy and safety of endoscopic submucosal dissection under general anesthesia. World J Gastrointest Endosc. 2016; 8:466–71. DOI: 10.4253/wjge.v8.i13.466. PMID: 27433293. PMCID: PMC4937162.14. Mirakhur RK. Sugammadex in clinical practice. Anaesthesia. 2009; 64(Suppl 1):45–54. DOI: 10.1111/j.1365-2044.2008.05870.x. PMID: 19222431.15. Cammu G, de Kam PJ, De Graeve K, van den Heuvel M, Suy K, Morias K, et al. Repeat dosing of rocuronium 1.2 mg/kg after reversal of neuromuscular block by sugammadex 4.0 mg/kg in anaesthetized healthy volunteers:a modelling-based pilot study. Br J Anaesth. 2010; 105:487–92. DOI: 10.1093/bja/aeq167. PMID: 20630888.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perforation of a Gastric Tear during Esophageal Endoscopic Submucosal Dissection under General Anesthesia
- Unexpected Delayed Colon Perforation after the Endoscopic Submucosal Dissection with Snaring of a Laterally Spreading Tumor
- General Anesthesia and Endoscopic Upper Gastrointestinal Tumor Resection
- A Case of Pneumorrhachis and Pneumoscrotum Following Colon Endoscopic Submucosal Dissection
- Treatment of Early Gastric Cancer: Endoscopic Submucosal Dissection with LASER