Korean Circ J.
2020 Jul;50(7):599-609. 10.4070/kcj.2019.0317.
The Clinical Course of Tuberculous Pericarditis in Immunocompetent Hosts Based on Serial Echocardiography
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Cardiovascular Diseases, Mayo Clinic College of Medicine, Rochester, MN, USA
- KMID: 2504219
- DOI: http://doi.org/10.4070/kcj.2019.0317
Abstract
- Background and Objectives
In East Asia, tuberculous pericarditis still occurs in immunocompetent patients. We aimed to investigate clinical course of tuberculous pericarditis and the trends of echocardiographic parameters for constrictive pericarditis.
Methods
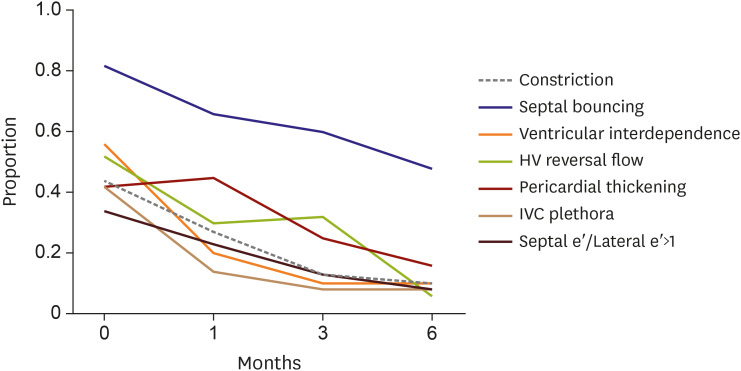
We retrospectively analyzed medical records of patients with tuberculous pericarditis between January 2010 and January 2017 in Samsung Medical Center. Treatment consists of the standard 4-drug anti-tuberculosis regimen for 6 months with or without corticosteroids. We performed echocardiography at initial diagnosis, 1, 3 and 6 months later.
Results
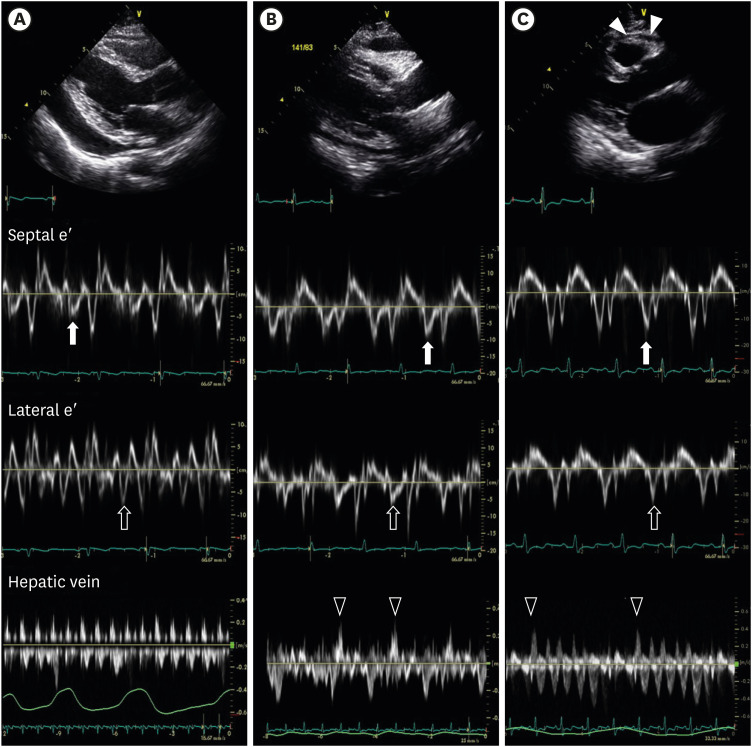
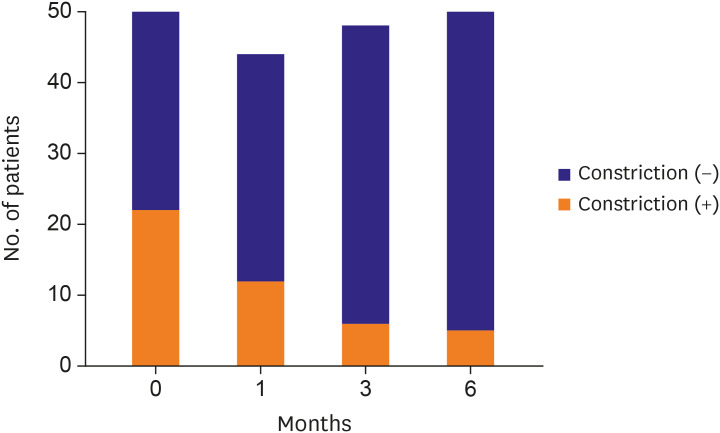
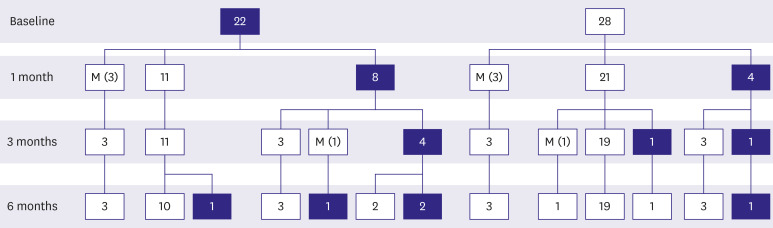
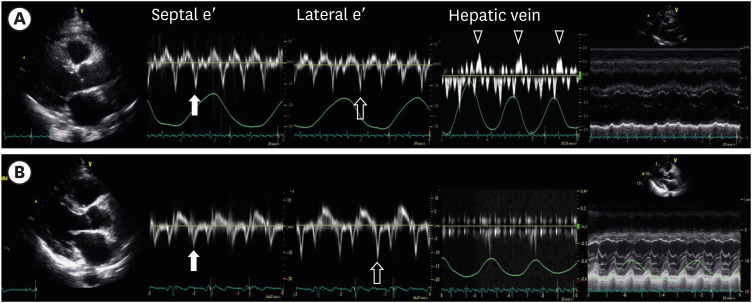
Total 50 cases with tuberculous pericarditis in immunocompetent patients were enrolled. Echocardiographic finding at initial diagnosis divided into 3 groups: 1) pericardial effusion only (n=28, 56.0%), 2) effusive constrictive pericarditis (n=10, 20.0%) and 3) constrictive pericarditis (n=12, 24.0%). The proportion of patients with constrictive pericarditis decreased gradually over time. After 6 months, only 5 patients still had constrictive pericarditis. Out of the 28 patients who initially presented with effusion alone, only one patient developed constrictive pericarditis. Echocardiographic parameters representing constrictive pericarditis gradually disappeared over the follow up period. Ventricular interdependency improved significantly from 1 month follow-up, whereas septal bounce and pericardial thickening were still observed after 6 months without significant constrictive physiology.
Conclusions
Tuberculous pericarditis with pericardial effusion without constrictive physiology is unlikely to develop into constrictive pericarditis in immunocompetent hosts, if treated with optimal anti-tuberculous medication and steroid therapy. Even though there were hemodynamic feature of constrictive pericarditis, more than 80% of the patients were improved from constrictive pericarditis.
Figure
Cited by 3 articles
-
Early Testing and Prompt Initiation of Proper Treatment: a Clever Strategy to Fight with Tuberculosis Pericarditis
Iksung Cho, William Dowon Kim
Korean Circ J. 2020;50(7):610-612. doi: 10.4070/kcj.2020.0179.Author's Reply to Septal Bounce or Ventricle Interdependence in Constrictive Pericarditis: Same or Different
Min Sun Kim, Sung-A Chang
Korean Circ J. 2020;50(7):630-631. doi: 10.4070/kcj.2020.1781.Septal Bounce or Ventricle Interdependence in Constrictive Pericarditis: Same or Different
Sourabh Agstam
Korean Circ J. 2020;50(7):628-629. doi: 10.4070/kcj.2020.0178.
Reference
-
1. Myers RB, Spodick DH. Constrictive pericarditis: clinical and pathophysiologic characteristics. Am Heart J. 1999; 138:219–232. PMID: 10426832.
Article2. Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC). G Ital Cardiol (Rome). 2015; 16:702–738. PMID: 26667949.3. Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005; 112:3608–3616. PMID: 16330703.
Article4. Harvey A, Whitehill M. Tuberculous pericarditis. Medicine. 1937; 16:45–94.
Article5. Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK. Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol. 2004; 43:271–275. PMID: 14736448.
Article6. Chang SA, Choi JY, Kim EK, et al. [18F]Fluorodeoxyglucose PET/CT predicts response to steroid therapy in constrictive pericarditis. J Am Coll Cardiol. 2017; 69:750–752. PMID: 28183513.7. Strang JI, Nunn AJ, Johnson DA, Casbard A, Gibson DG, Girling DJ. Management of tuberculous constrictive pericarditis and tuberculous pericardial effusion in Transkei: results at 10 years follow-up. QJM. 2004; 97:525–535. PMID: 15256610.
Article8. Strang JI. Rapid resolution of tuberculous pericardial effusions with high dose prednisone and anti-tuberculous drugs. J Infect. 1994; 28:251–254. PMID: 8089513.
Article9. Strang JI, Kakaza HH, Gibson DG, et al. Controlled clinical trial of complete open surgical drainage and of prednisolone in treatment of tuberculous pericardial effusion in Transkei. Lancet. 1988; 2:759–764. PMID: 2901610.
Article10. Chang SA. Tuberculous and infectious pericarditis. Cardiol Clin. 2017; 35:615–622. PMID: 29025551.
Article11. Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013; 26:965–1012.e15. PMID: 23998693.12. Ha JW, Oh JK, Ling LH, Nishimura RA, Seward JB, Tajik AJ. Annulus paradoxus: transmitral flow velocity to mitral annular velocity ratio is inversely proportional to pulmonary capillary wedge pressure in patients with constrictive pericarditis. Circulation. 2001; 104:976–978. PMID: 11524387.13. Maisch B, Seferović PM, Ristić AD, et al. Guidelines on the diagnosis and management of pericardial diseases. Executive summary. Rev Esp Cardiol. 2004; 57:1090–1114. PMID: 15544758.14. Wiysonge CS, Ntsekhe M, Thabane L, et al. Interventions for treating tuberculous pericarditis. Cochrane Database Syst Rev. 2017; 9:CD000526. PMID: 28902412.
Article15. Kadhiravan T, Deepanjali S. Role of corticosteroids in the treatment of tuberculosis: an evidence-based update. Indian J Chest Dis Allied Sci. 2010; 52:153–158. PMID: 20949734.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of tuberculous pericarditis presenting as pericardial mass compressing pulmonary artery
- The Characteristics and Related Factors with Severe Uremic Pericarditis
- Redefining Effusive-Constrictive Pericarditis with Echocardiography
- A Case of Tuberculous Pericarditis Diagnosed by Increased ADA Activity in Pericardial Fluid
- A Cases of Tuberculous Pericarditis Associated with Pseudoaneurysm of the Left Ventricle