Restor Dent Endod.
2020 May;45(2):e11. 10.5395/rde.2020.45.e11.
Micro-computed tomographic evaluation of the flow and filling ability of endodontic materials using different test models
- Affiliations
-
- 1Department of Restorative Dentistry, São Paulo State University (UNESP), School of Dentistry, Araraquara, SP, Brazil
- KMID: 2503508
- DOI: http://doi.org/10.5395/rde.2020.45.e11
Abstract
Objectives
This study compared the flow and filling of several retrograde filling materials using new different test models.
Materials and Methods
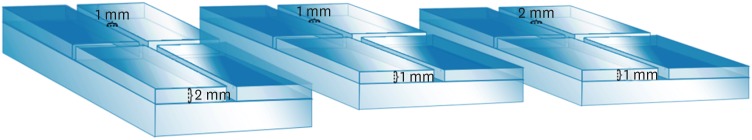
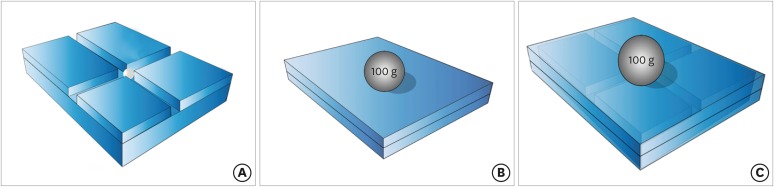
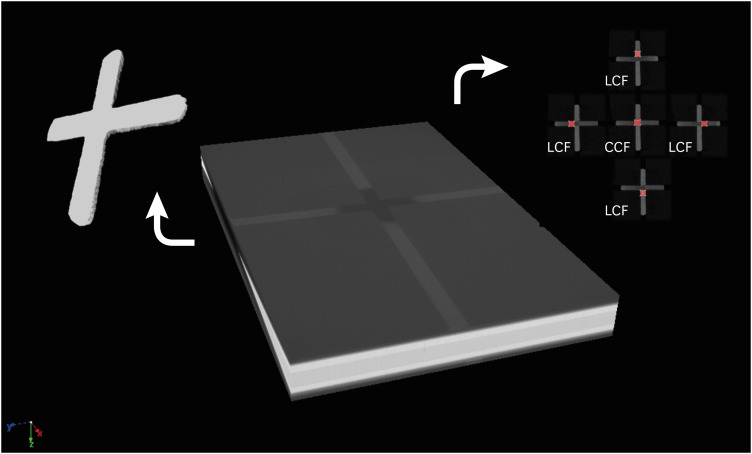
Glass plates were manufactured with a central cavity and 4 grooves in the horizontal and vertical directions. Grooves with the dimensions used in the previous study (1 × 1 × 2 mm; length, width, and height respectively) were compared with grooves measuring 1 × 1 × 1 and 1 × 2 × 1 mm. Biodentine, intermediate restorative material (IRM), and mineral trioxide aggregate (MTA) were evaluated. Each material was placed in the central cavity, and then another glass plate and a metal weight were placed over the cement. The glass plate/material set was scanned using micro-computed tomography. Flow was calculated by linear measurements in the grooves. Central filling was calculated in the central cavity (mm3) and lateral filling was measured up to 2 mm from the central cavity.
Results
Biodentine presented the least flow and better filling than IRM when evaluated in the 1 × 1 × 2 model. In a comparison of the test models, MTA had the most flow in the 1 × 1 × 2 model. All materials had lower lateral filling when the 1 × 1 × 2 model was used.
Conclusions
Flow and filling were affected by the size of the test models. Higher grooves and materials with greater flow resulted in lower filling capacity. The test model measuring 1 × 1 × 2 mm showed a better ability to differentiate among the materials.
Keyword
Figure
Cited by 2 articles
-
How do imaging protocols affect the assessment of root-end fillings?
Fernanda Ferrari Esteves Torres, Reinhilde Jacobs, Mostafa EzEldeen, Karla de Faria-Vasconcelos, Juliane Maria Guerreiro-Tanomaru, Bernardo Camargo dos Santos, Mário Tanomaru-Filho
Restor Dent Endod. 2021;47(1):e2. doi: 10.5395/rde.2022.47.e2.A micro-computed tomographic study using a novel test model to assess the filling ability and volumetric changes of bioceramic root repair materials
Fernanda Ferrari Esteves Torres, Jader Camilo Pinto, Gabriella Oliveira Figueira, Juliane Maria Guerreiro-Tanomaru, Mario Tanomaru-Filho
Restor Dent Endod. 2020;46(1):e2. doi: 10.5395/rde.2021.46.e2.
Reference
-
1. Adl A, Sadat Shojaee N, Pourhatami N. Evaluation of the dislodgement resistance of a new pozzolan-based cement (EndoSeal MTA) compared to ProRoot MTA and Biodentine in the presence and absence of blood. Scanning. 2019; 2019:3863069. PMID: 31210836.
Article2. Küçükkaya Eren S, Aksel H, Serper A. Effect of placement technique on the push-out bond strength of calcium-silicate based cements. Dent Mater J. 2016; 35:742–747. PMID: 27546860.3. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review--Part I: chemical, physical, and antibacterial properties. J Endod. 2010; 36:16–27. PMID: 20003930.
Article4. Alcalde MP, Vivan RR, Marciano MA, Duque JA, Fernandes SL, Rosseto MB, Duarte MA. Effect of ultrasonic agitation on push-out bond strength and adaptation of root-end filling materials. Restor Dent Endod. 2018; 43:e23. PMID: 29765903.
Article5. Küçükkaya Eren S, Parashos P. Adaptation of mineral trioxide aggregate to dentine walls compared with other root-end filling materials: a systematic review. Aust Endod J. 2019; 45:111–121. PMID: 29450937.
Article6. Saxena P, Gupta SK, Newaskar V. Biocompatibility of root-end filling materials: recent update. Restor Dent Endod. 2013; 38:119–127. PMID: 24010077.
Article7. Akbulut MB, Arpaci PU, Eldeniz AU. Effects of four novel root-end filling materials on the viability of periodontal ligament fibroblasts. Restor Dent Endod. 2018; 43:e24. PMID: 30135845.
Article8. Kohli MR, Berenji H, Setzer FC, Lee SM, Karabucak B. Outcome of endodontic surgery: a meta-analysis of the literature-part 3: comparison of endodontic microsurgical techniques with 2 different root-end filling materials. J Endod. 2018; 44:923–931. PMID: 29681480.
Article9. Al-Haddad A, Abu Kasim NH, Che Ab Aziz ZA. Interfacial adaptation and thickness of bioceramic-based root canal sealers. Dent Mater J. 2015; 34:516–521. PMID: 26235718.
Article10. Song YS, Choi Y, Lim MJ, Yu MK, Hong CU, Lee KW, Min KS. In vitro evaluation of a newly produced resin-based endodontic sealer. Restor Dent Endod. 2016; 41:189–195. PMID: 27508160.11. Almeida JF, Gomes BP, Ferraz CC, Souza-Filho FJ, Zaia AA. Filling of artificial lateral canals and microleakage and flow of five endodontic sealers. Int Endod J. 2007; 40:692–699. PMID: 17608677.
Article12. Tanomaru-Filho M, Torres FF, Bosso-Martelo R, Chávez-Andrade GM, Bonetti-Filho I, Guerreiro-Tanomaru JM. A novel model for evaluating the flow of endodontic materials using micro-computed tomography. J Endod. 2017; 43:796–800. PMID: 28268019.
Article13. International Organization for Standardization. ISO 6876: Dental root canal sealing materials. Geneva: International Organization for Standardization;2012.14. Kim K, Kim DV, Kim SY, Yang S. A micro-computed tomographic study of remaining filling materials of two bioceramic sealers and epoxy resin sealer after retreatment. Restor Dent Endod. 2019; 44:e18. PMID: 31149616.
Article15. Jang JH, Lee HW, Cho KM, Shin HW, Kang MK, Park SH, Kim E. In vitro characterization of human dental pulp stem cells isolated by three different methods. Restor Dent Endod. 2016; 41:283–295. PMID: 27847750.16. Duarte MA, Ordinola-Zapata R, Bernardes RA, Bramante CM, Bernardineli N, Garcia RB, de Moraes IG. Influence of calcium hydroxide association on the physical properties of AH Plus. J Endod. 2010; 36:1048–1051. PMID: 20478463.
Article17. Kim J, Song YS, Min KS, Kim SH, Koh JT, Lee BN, Chang HS, Hwang IN, Oh WM, Hwang YC. Evaluation of reparative dentin formation of ProRoot MTA, Biodentine and BioAggregate using micro-CT and immunohistochemistry. Restor Dent Endod. 2016; 41:29–36. PMID: 26877988.
Article18. Oltra E, Cox TC, LaCourse MR, Johnson JD, Paranjpe A. Retreatability of two endodontic sealers, EndoSequence BC Sealer and AH Plus: a micro-computed tomographic comparison. Restor Dent Endod. 2017; 42:19–26. PMID: 28194360.
Article19. Torres FF, Guerreiro-Tanomaru JM, Bosso-Martelo R, Chavez-Andrade GM, Tanomaru Filho M. Solubility, porosity and fluid uptake of calcium silicate-based cements. J Appl Oral Sci. 2018; 26:e20170465. PMID: 29791569.
Article20. Torres FF, Guerreiro-Tanomaru JM, Bosso-Martelo R, Espir CG, Camilleri J, Tanomaru-Filho M. Solubility, porosity, dimensional and volumetric change of endodontic sealers. Braz Dent J. 2019; 30:368–373. PMID: 31340227.
Article21. Yanpiset K, Banomyong D, Chotvorrarak K, Srisatjaluk RL. Bacterial leakage and micro-computed tomography evaluation in round-shaped canals obturated with bioceramic cone and sealer using matched single cone technique. Restor Dent Endod. 2018; 43:e30. PMID: 30135849.
Article22. Peralta SL, Leles SB, Dutra AL, Guimarães VB, Piva E, Lund RG. Evaluation of physical-mechanical properties, antibacterial effect, and cytotoxicity of temporary restorative materials. J Appl Oral Sci. 2018; 26:e20170562. PMID: 30133673.
Article23. Tsesis I, Elbahary S, Venezia NB, Rosen E. Bacterial colonization in the apical part of extracted human teeth following root-end resection and filling: a confocal laser scanning microscopy study. Clin Oral Investig. 2018; 22:267–274.
Article24. Aksel H, Küçükkaya Eren S, Askerbeyli Õrs S, Karaismailoğlu E. Surface and vertical dimensional changes of mineral trioxide aggregate and biodentine in different environmental conditions. J Appl Oral Sci. 2018; 27:e20180093. PMID: 30540071.
Article25. Biočanin V, Antonijević Đ, Poštić S, Ilić D, Vuković Z, Milić M, Fan Y, Li Z, Brković B, Đurić M. Marginal gaps between 2 calcium silicate and glass ionomer cements and apical root dentin. J Endod. 2018; 44:816–821. PMID: 29336880.
Article26. Akbulut MB, Bozkurt DA, Terlemez A, Akman M. The push-out bond strength of BIOfactor mineral trioxide aggregate, a novel root repair material. Restor Dent Endod. 2019; 44:e5. PMID: 30834227.
Article27. Küçükkaya Eren S, Aksel H, Askerbeyli Örs S, Serper A, Koçak Y, Ocak M, Çelik HH. Obturation quality of calcium silicate-based cements placed with different techniques in teeth with perforating internal root resorption: a micro-computed tomographic study. Clin Oral Investig. 2019; 23:805–811.
Article28. Torres FF, Bosso-Martelo R, Espir CG, Cirelli JA, Guerreiro-Tanomaru JM, Tanomaru-Filho M. Evaluation of physicochemical properties of root-end filling materials using conventional and Micro-CT tests. J Appl Oral Sci. 2017; 25:374–380. PMID: 28877275.
Article29. Tang JJ, Shen ZS, Qin W, Lin Z. A comparison of the sealing abilities between Biodentine and MTA as root-end filling materials and their effects on bone healing in dogs after periradicular surgery. J Appl Oral Sci. 2019; 27:e20180693. PMID: 31596370.
Article30. Yilmaz A, Helvacioglu-Yigit D, Gur C, Ersev H, Kiziltas Sendur G, Avcu E, Baydemir C, Abbott PV. Evaluation of dentin defect formation during retreatment with hand and rotary instruments: a micro-CT study. Scanning. 2017; 2017:4868603. PMID: 29109814.
Article31. Camilleri J, Sorrentino F, Damidot D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, Biodentine and MTA Angelus. Dent Mater. 2013; 29:580–593. PMID: 23537569.
Article32. Ber BS, Hatton JF, Stewart GP. Chemical modification of proroot mta to improve handling characteristics and decrease setting time. J Endod. 2007; 33:1231–1234. PMID: 17889696.
Article33. Hsieh SC, Teng NC, Lin YC, Lee PY, Ji DY, Chen CC, Ke ES, Lee SY, Yang JC. A novel accelerator for improving the handling properties of dental filling materials. J Endod. 2009; 35:1292–1295. PMID: 19720234.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A micro-computed tomographic study using a novel test model to assess the filling ability and volumetric changes of bioceramic root repair materials
- Micro-computed tomographic evaluation of a new system for root canal filling using calcium silicatebased root canal sealers
- Retreatability of two endodontic sealers, EndoSequence BC Sealer and AH Plus: a micro-computed tomographic comparison
- A micro-computed tomographic study of remaining filling materials of two bioceramic sealers and epoxy resin sealer after retreatment
- A micro-computed tomographic evaluation of root canal filling with a single gutta-percha cone and calcium silicate sealer