Neurointervention.
2020 Jul;15(2):67-73. 10.5469/neuroint.2020.00129.
Low-Dose Fluoroscopy Protocol for Diagnostic Cerebral Angiography
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Radiologic Technology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Advanced Therapies, Siemens Healthineers Ltd., Seoul, Korea
- KMID: 2503391
- DOI: http://doi.org/10.5469/neuroint.2020.00129
Abstract
- Purpose
We applied a low-dose fluoroscopic protocol in routine diagnostic cerebral angiography and evaluated the feasibility of the protocol.
Materials and Methods
We retrospectively reviewed a total of 60 patients who underwent diagnostic cerebral angiography for various neurovascular diseases from September to November 2019. Routine protocols were used for patients in the first phase and low-dose protocols in the second phase. We compared radiation dose, fluoroscopy time, and complications between groups.
Results
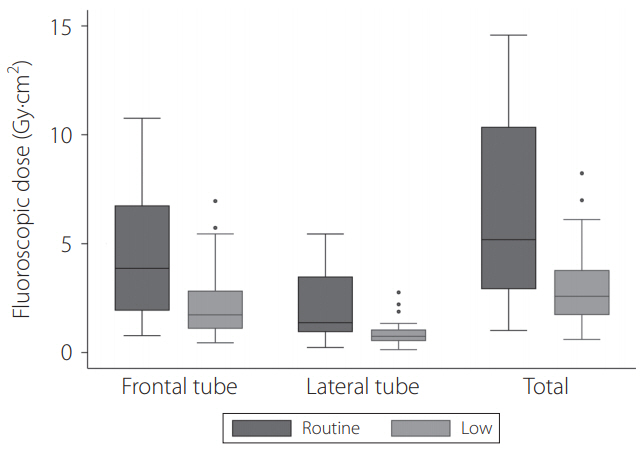
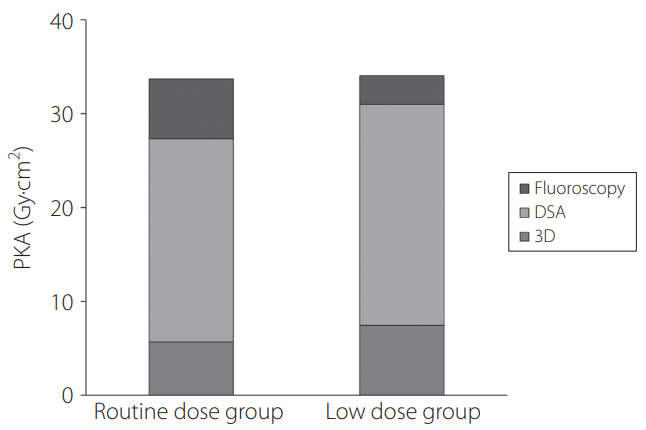
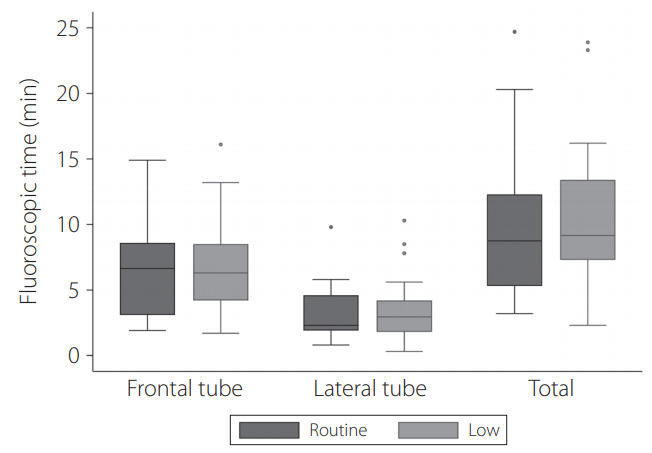
Age, diseases, and operators were not significantly different between the two groups. The mean fluoroscopy dose significantly decreased by 52% in the low-dose group (3.09 vs. 6.38 Gy·cm2 ); however, the total dose was not significantly different between the two groups (34.07 vs. 33.70 Gy·cm2 ). The total fluoroscopic time was slightly longer in the low-dose group, but the difference was not statistically significant (12.2. vs. 12.5 minutes). In all patients, angiography was successfully performed without complications.
Conclusion
The low-dose fluoroscopy protocol is feasible to apply for diagnostic cerebral angiography in that this protocol could significantly reduce the fluoroscopic dose.
Keyword
Figure
Cited by 1 articles
-
Recent Radiation Reduction Strategies for Neurointerventionists
Jae Ho Shin
Neurointervention. 2020;15(3):167-170. doi: 10.5469/neuroint.2020.00346.
Reference
-
1. Song Y, Kim Y, Han S, Kim TI, Choi JH, Maeng JY, et al. Estimated radiation dose according to the craniocaudal angle in cerebral digital subtraction angiography: patient and phantom study. J Neuroradiol. 2019; 46:345–350.
Article2. Maeng JY, Song Y, Sung YS, Kim TI, Lee DH, Kim TH. Feasibility of ultra-low radiation dose digital subtraction angiography: preliminary study in a simplified cerebral angiography phantom. Interv Neuroradiol. 2019; 25:589–595.
Article3. Ihn YK, Kim BS, Byun JS, Suh SH, Won YD, Lee DH, et al. Patient radiation exposure during diagnostic and therapeutic procedures for intracranial aneurysms: a multicenter study. Neurointervention. 2016; 11:78–85.
Article4. Riabroi K, Khanungwanitkul K, Wattanapongpitak P, Krisanachinda A, Hongsakul K. Patient radiation dose in neurointerventional radiologic procedure: a tertiary care experience. Neurointervention. 2018; 13:110–116.
Article5. Yi HJ, Sung JH, Lee DH, Kim SW, Lee SW. Analysis of radiation doses and dose reduction strategies during cerebral digital subtraction angiography. World Neurosurg. 2017; 100:216–223.
Article6. Schneider T, Wyse E, Pearl MS. Analysis of radiation doses incurred during diagnostic cerebral angiography after the implementation of dose reduction strategies. J Neurointerv Surg. 2017; 9:384–388.
Article7. Kim DJ, Park MK, Jung DE, Kang JH, Kim BM. Radiation dose reduction without compromise to image quality by alterations of filtration and focal spot size in cerebral angiography. Korean J Radiol. 2017; 18:722–728.
Article8. Honarmand AR, Shaibani A, Pashaee T, Syed FH, Hurley MC, Sammet CL, et al. Subjective and objective evaluation of image quality in biplane cerebral digital subtraction angiography following significant acquisition dose reduction in a clinical setting. J Neurointerv Surg. 2017; 9:297–301.
Article9. Kahn EN, Gemmete JJ, Chaudhary N, Thompson BG, Chen K, Christodoulou EG, et al. Radiation dose reduction during neurointerventional procedures by modification of default settings on biplane angiography equipment. J Neurointerv Surg. 2016; 8:819–823.
Article10. Pearl MS, Torok C, Wang J, Wyse E, Mahesh M, Gailloud P. Practical techniques for reducing radiation exposure during cerebral angiography procedures. J Neurointerv Surg. 2015; 7:141–145.
Article11. Alexander MD, Oliff MC, Olorunsola OG, Brus-Ramer M, Nickoloff EL, Meyers PM. Patient radiation exposure during diagnostic and therapeutic interventional neuroradiology procedures. J Neurointerv Surg. 2010; 2:6–10.
Article12. Plank F, Stowasser B, Till D, Schgör W, Dichtl W, Hintringer F, et al. Reduction of fluoroscopy dose for cardiac electrophysiology procedures: a feasibility and safety study. Eur J Radiol. 2019; 110:105–111.
Article13. Crowhurst J, Haqqani H, Wright D, Whitby M, Lee A, Betts J, et al. Ultra-low radiation dose during electrophysiology procedures using optimized new generation fluoroscopy technology. Pacing Clin Electrophysiol. 2017; 40:947–954.
Article14. Attanasio P, Mirdamadi M, Wielandts JY, Pieske B, Blaschke F, Boldt LH, et al. Safety and efficacy of applying a low-dose radiation fluoroscopy protocol in device implantations. Europace. 2017; 19:1364–1368.
Article15. Lee SY, Kim J, Lee SH, Choi JH, Kim JS, Park YH, et al. Reduction of radiation exposure during catheter ablation for paroxysmal supraventricular tachycardia: the effect of a low frame rate of digital pulsed fluoroscopy. Int J Cardiol. 2014; 177:573–574.
Article16. Wildgruber M, Köhler M, Brill R, Goessmann H, Uller W, MüllerWille R, et al. Impact of low dose settings on radiation exposure during pediatric fluoroscopic guided interventions. Eur J Radiol. 2018; 100:1–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patient Radiation Dose in Diagnostic and Interventional Procedures for Intracranial Aneurysms: Experience at a Single Center
- Safety and Effectiveness of the Novel Catheter 3.0 System for Diagnostic Cerebral Angiography: A Pilot Study
- Review of National Diagnostic Reference Levels for Interventional Procedures
- Is a Low Dose Computed Tomography Angiography Protocol Feasible in Terms of Maintaining Adequate Diagnostic Image Quality for TAVR Candidates?
- Transient Cortical Blindness following Cerebral Angiography : Case Report