J Neurocrit Care.
2020 Jun;13(1):65-68. 10.18700/jnc.190115.
Favorable clinical course after early-intensive immunotherapy for new-onset refractory status epilepticus
- Affiliations
-
- 1Department of Neurology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Republic of Korea
- 2Department of Neurology, Pusan National University Hospital, Busan, Republic of Korea
- KMID: 2503388
- DOI: http://doi.org/10.18700/jnc.190115
Abstract
- Background
New-onset refractory status epilepticus (NORSE) refers to the newly established concept of a disease characterized by refractory status epilepticus without an identifiable etiology. Recent reports have indicated the importance of immunotherapy for NORSE.
Case Report
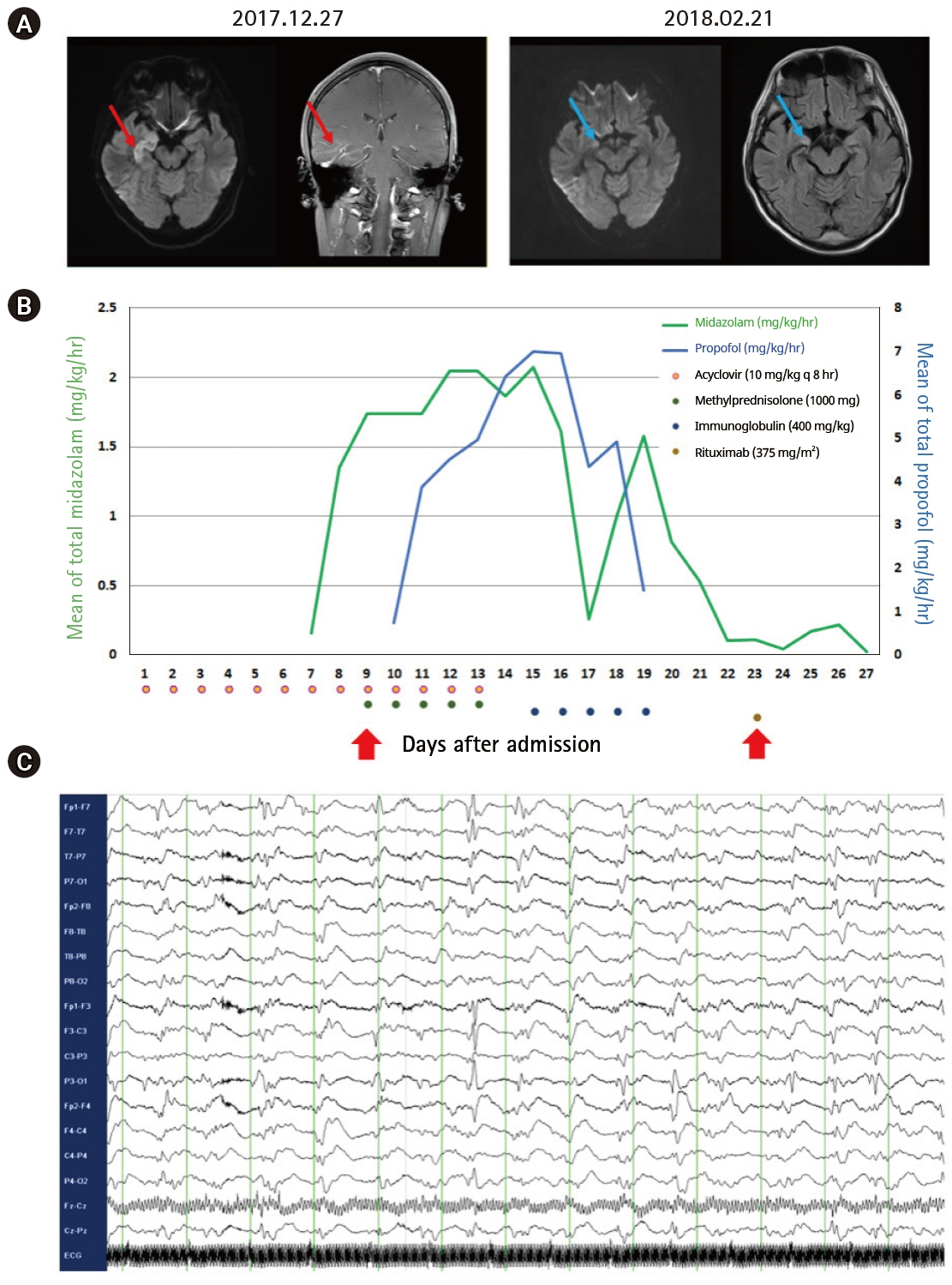
A 37-year-old man with no past history of epilepsy was admitted for a presenting complaint of confusion. He was treated with intravenous acyclovir and an antiepileptic drug (AED), following a preliminary diagnosis of herpes encephalitis. He developed generalized tonic-clonic seizures on day 6 of admission that worsened progressively despite treatment with multiple AEDs. NORSE was considered to be a probable diagnosis at this stage and immunotherapy with intravenous methylprednisolone and immunoglobulin was scheduled. However, persistent seizure activity was observed on the electroencephalogram after the completion of initial immunotherapy. Subsequently, rituximab was administered for 4 weeks. He eventually regained consciousness and was able to resume social activity.
Conclusion
Our patient exhibited a favorable outcome with early-intensive immunotherapy and subsequent rituximab treatment for NORSE.
Figure
Reference
-
1. Mayer SA, Claassen J, Lokin J, Mendelsohn F, Dennis LJ, Fitzsimmons BF. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol. 2002; 59:205–10.2. Hocker SE, Britton JW, Mandrekar JN, Wijdicks EF, Rabinstein AA. Predictors of outcome in refractory status epilepticus. JAMA Neurol. 2013; 70:72–7.
Article3. Gaspard N, Hirsch LJ, Sculier C, Loddenkemper T, van Baalen A, Lancrenon J, et al. New-onset refractory status epilepticus (NORSE) and febrile infection-related epilepsy syndrome (FIRES): state of the art and perspectives. Epilepsia. 2018; 59:745–52.
Article4. Shin JW, Koo YS, Kim YS, Kim DW, Kim KK, Lee SY, et al. Clinical characterization of unknown/cryptogenic status epilepticus suspected as encephalitis: a multicenter cohort study. J Neuroimmunol. 2018; 315:1–8.
Article5. Hermetter C, Fazekas F, Hochmeister S. Systematic review: syndromes, early diagnosis, and treatment in autoimmune encephalitis. Front Neurol. 2018; 9:706.
Article6. Gaspard N, Foreman BP, Alvarez V, Cabrera Kang C, Probasco JC, Jongeling AC, et al. New-onset refractory status epilepticus: etiology, clinical features, and outcome. Neurology. 2015; 85:1604–13.7. Dalakas MC. B cells as therapeutic targets in autoimmune neurological disorders. Nat Clin Pract Neurol. 2008; 4:557–67.
Article8. Lee WJ, Lee ST, Byun JI, Sunwoo JS, Kim TJ, Lim JA, et al. Rituximab treatment for autoimmune limbic encephalitis in an institutional cohort. Neurology. 2016; 86:1683–91.
Article9. Whittam DH, Tallantyre EC, Jolles S, Huda S, Moots RJ, Kim HJ, et al. Rituximab in neurological disease: principles, evidence and practice. Pract Neurol. 2019; 19:5–20.
Article10. Kirmani BF, Barr D, Robinson DM, Pranske Z, Fonkem E, Benge J, et al. Management of autoimmune status epilepticus. Front Neurol. 2018; 9:259.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Status Epilepticus and Beyond: A Clinical Review of Status Epilepticus and an Update on Current Management Strategies in Super-refractory Status Epilepticus
- Sevoflurane for the Management of Refractory Status Epilepticus : A case report
- Management strategies for refractory status epilepticus
- Consciousness Recovery by Rituximab after Seizure Control in Cryptogenic New-Onset Refractory Status Epilepticus
- Febrile Infection-Related Epilepsy Syndrome: Refractory Status Epilepticus and Management Strategies