J Educ Eval Health Prof.
2019;16:30. 10.3352/jeehp.2019.16.30.
Dreyfus scale-based feedback increased medical students’ satisfaction with the complex cluster part of a interviewing and physical examination course and improved skills readiness in Taiwan
- Affiliations
-
- 1Department of Medicine, National Yang-Ming University, Taipei, Taiwan
- 2Bali Psychiatric Center, Ministry of Health and Welfare, Taipei, Taiwan
- 3Division of Clinical Skills Training, Department of Medical Education, Taipei Veterans General Hospital, Taipei, Taiwan
- 4Division of General Medicine, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan
- 5Office of Medical Education, University of New South Wales Australia, Sydney, Australia
- KMID: 2502170
- DOI: http://doi.org/10.3352/jeehp.2019.16.30
Abstract
- Purpose
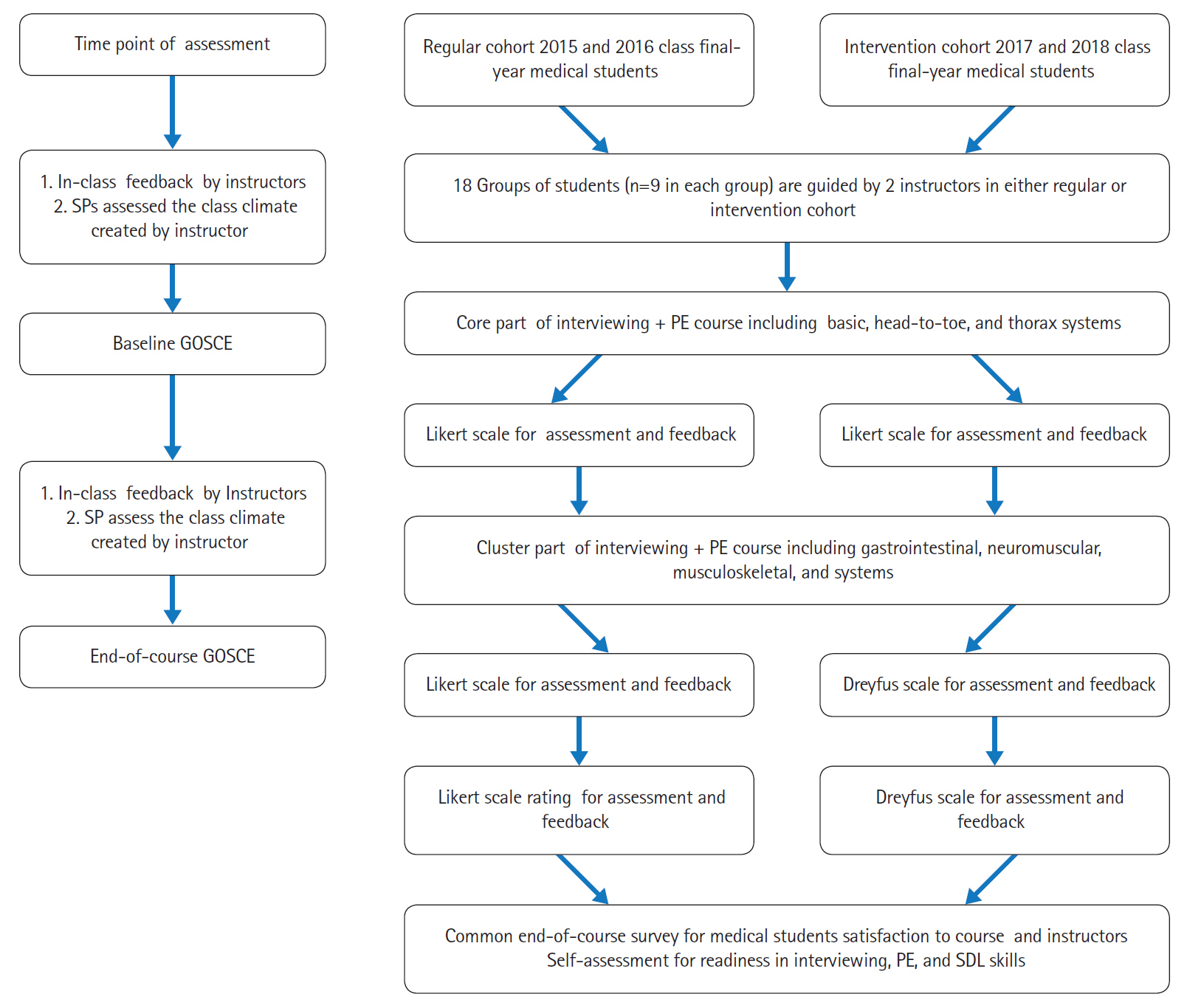
In contrast to the core part of the clinical interviewing and physical examination (PE) skills course, corresponding to the basic, head-to-toe, and thoracic systems, learners need structured feedback in the cluster part of the course, which includes the abdominal, neuromuscular, and musculoskeletal systems. This study evaluated the effects of using Dreyfus scale-based feedback, which has elements of continuous professional development, instead of Likert scale-based feedback in the cluster part of training in Taiwan.
Methods
Instructors and final-year medical students in the 2015–2016 classes of National Yang-Ming University, Taiwan comprised the regular cohort, whereas those in the 2017–2018 classes formed the intervention cohort. In the intervention cohort, Dreyfus scale-based feedback, rather than Likert scale-based feedback, was used in the cluster part of the course.
Results
In the cluster part of the course in the regular cohort, pre-trained standardized patients rated the class climate as poor, and students expressed low satisfaction with the instructors and course and low self-assessed readiness. In comparison with the regular cohort, improved end-of-course group objective structured clinical examination scores after the cluster part were noted in the intervention cohort. In other words, the implementation of Dreyfus scale-based feedback in the intervention cohort for the cluster part improved the deficit in this section of the course.
Conclusion
The implementation of Dreyfus scale-based feedback helped instructors to create a good class climate in the cluster part of the clinical interviewing and PE skills course. Simultaneously, this new intervention achieved the goal of promoting medical students’ readiness for interviewing, PE, and self-directed learning.
Keyword
Figure
Reference
-
References
1. Haring CM, Cools BM, van der Meer JW, Postma CT. Student performance of the general physical examination in internal medicine: an observational study. BMC Med Educ. 2014; 14:73. https://doi.org/10.1186/1472-6920-14-73.
Article2. Gowda D, Blatt B, Fink MJ, Kosowicz LY, Baecker A, Silvestri RC. A core physical exam for medical students: results of a national survey. Acad Med. 2014; 89:436–442. https://doi.org/10.1097/ACM.0000000000000137.
Article3. Ramani S, Ring BN, Lowe R, Hunter D. A pilot study assessing knowledge of clinical signs and physical examination skills in incoming medicine residents. J Grad Med Educ. 2010; 2:232–235. https://doi.org/10.4300/JGME-D-09-00107.1.
Article4. Krautter M, Diefenbacher K, Schultz JH, Maatouk I, Herrmann-Werner A, Koehl-Hackert N, Herzog W, Nikendei C. Physical examination skills training: faculty staff vs. patient instructor feedback: a controlled trial. PLoS One. 2017; 12:e0180308. https://doi.org/10.1371/journal.pone.0180308.
Article5. Danielson AR, Venugopal S, Mefford JM, Clarke SO. How do novices learn physical examination skills?: a systematic review of the literature. Med Educ Online. 2019; 24:1608142. https://doi.org/10.1080/10872981.2019.1608142.
Article6. Pena A. The Dreyfus model of clinical problem-solving skills acquisition: a critical perspective. Med Educ Online. 2010; 15:4846. https://doi.org/10.3402/meo.v15i0.4846.
Article7. Park J. Proposal for a Modified Dreyfus and Miller Model with simplified competency level descriptions for performing self-rated surveys. J Educ Eval Health Prof. 2015; 12:54. https://doi.org/10.3352/jeehp.2015.12.54.
Article8. Amatari VO. The instructional process: a review of Flanders’ interaction analysis in a classroom setting. Int J Second Educ. 2015; 3:43–49. https://doi.org/10.11648/j.ijsedu.20150305.11.
Article9. Miles S, Kellett J, Leinster SJ. Medical graduates' preparedness to practice: a comparison of undergraduate medical school training. BMC Med Educ. 2017; 17:33. https://doi.org/10.1186/s12909-017-0859-6.
Article10. Kern DH, Mainous AG 3rd, Carey M, Beddingfield A. Simulation-based teaching to improve cardiovascular exam skills performance among third-year medical students. Teach Learn Med. 2011; 23:15–20. https://doi.org/10.1080/10401334.2011.536753.
Article11. Yang YY, Lee FY, Hsu HC, Huang CC, Chen JW, Lee WS, Chuang CL, Chang CC, Chen HM, Huang CC. A core competence-based objective structured clinical examination (OSCE) in evaluation of clinical performance of postgraduate year-1 (PGY1) residents. J Chin Med Assoc. 2011; 74:198–204. https://doi.org/10.1016/j.jcma.2011.03.003.
Article12. Peitzman SJ, Cuddy MM. Performance in physical examination on the USMLE step 2 clinical skills examination. Acad Med. 2015; 90:209–213. https://doi.org/10.1097/ACM.0000000000000570.
Article13. Yoon MH, Blatt BC, Greenberg LW. Medical students’ professional development as educators revealed through reflections on their teaching following a students-as-teachers course. Teach Learn Med. 2017; 29:411–419. https://doi.org/10.1080/10401334.2017.1302801.
Article14. Lyon LJ. Development of teaching expertise viewed through the Dreyfus model of skill acquisition. J Scholarsh Teach Learn. 2015; 15:88–105. https://doi.org/10.14434/josotl.v15i1.12866.
Article15. Embo MP, Driessen EW, Valcke M, van der Vleuten CP. Assessment and feedback to facilitate self-directed learning in clinical practice of Midwifery students. Med Teach. 2010; 32:e263–e269. https://doi.org/10.3109/0142159X.2010.490281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Computer-Assisted, Real-Time Feedback System for Medical Students as a Tool for Web-Based Learning
- Providing Effective Feedback within Pharmacy Practice Education
- Medical Students' Change of Thought after a Two Year Course on Medical Interview Skills
- Motivational Interviewing Training Using Role Play in Dental Hygiene Students
- Formative feedback from the first-person perspective using Google Glass in a family medicine objective structured clinical examination station in the United States