Intest Res.
2020 Apr;18(2):229-237. 10.5217/ir.2019.09150.
Prototype single-balloon enteroscopy with passive bending and high force transmission improves depth of insertion in the small intestine
- Affiliations
-
- 1Department of Medicine, Shiga University of Medical Science, Otsu, Japan
- 2Division of Clinical Nutrition, Shiga University of Medical Science, Otsu, Japan
- 3Department of Comprehensive Internal Medicine, Shiga University of Medical Science, Otsu, Japan
- KMID: 2501388
- DOI: http://doi.org/10.5217/ir.2019.09150
Abstract
- Background/Aims
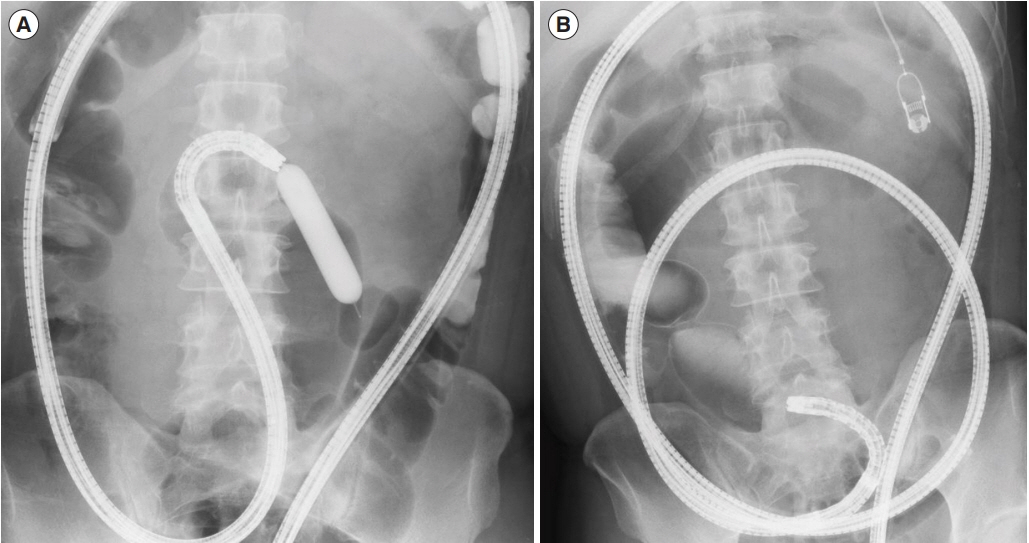
We retrospectively analyzed Crohn’s disease (CD) patients with small intestinal strictures who underwent single-balloon enteroscopy (SBE) to ascertain whether prototype SBEs with a passive bending mechanism and high force transmission insertion tube had better insertability in the small intestine than a conventional SBE.
Methods
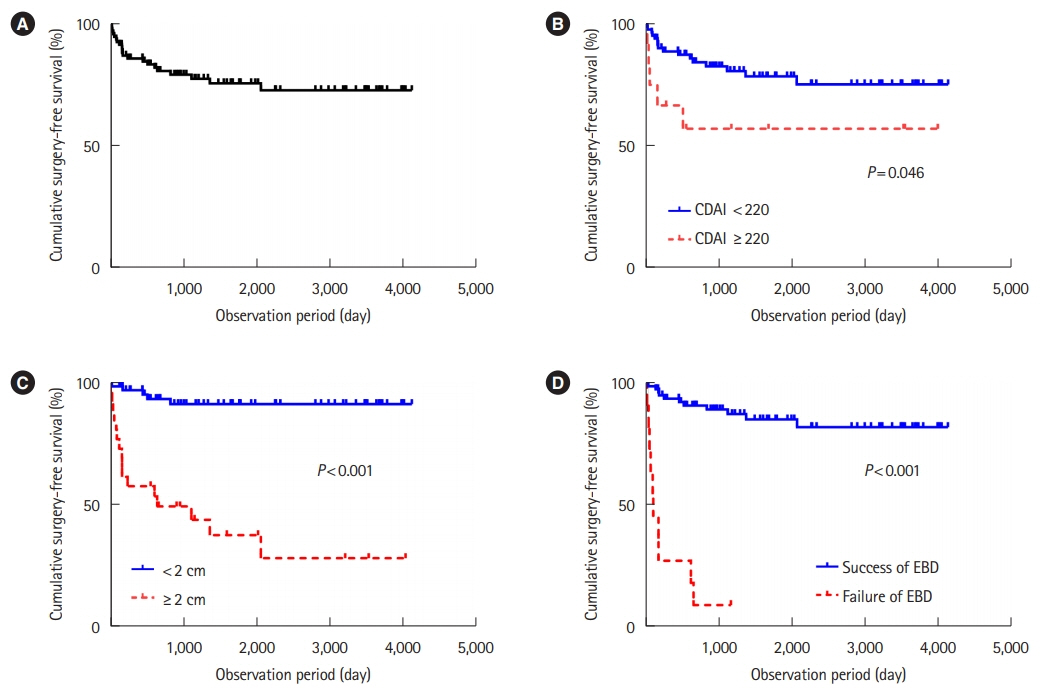
Among 253 CD patients who underwent SBE, we identified 94 CD patients who had undergone attempted endoscopic balloon dilatation (EBD) for small intestinal stenosis for inclusion in this study. We analyzed whether the type of scope used for their initial procedure affected the cumulative surgery-free rate. For the insertability analysis, patients who underwent SBE at least twice were divided into 3 groups according to the type of scope used: conventional SBE only, prototype SBE only, and both conventional and prototype SBEs. For each group, depth of insertion, procedure time, and number of EBDs were compared in the same patient at different time points.
Results
The success rate of EBD was 88.3%. The 5- and 10-year cumulative surgery-free rate was 75.7% and 72.8%, respectively. Cox regression analysis indicated that the factors contributing to surgery were long stricture (≥2 cm), EBD failure, and elevated Crohn’s Disease Activity Index, but not the type of scope used for EBD. The prototype SBEs significantly improved the depth of insertion (P=0.03, Wilcoxon’s signed-rank test).
Conclusions
In CD patients with small intestinal stenosis, the prototype SBEs with a passive bending mechanism and high force transmission insertion tube did not improve long-term EBD outcome but did improve deep insertability. (Clinical Trial Registration No. UMIN000037102)
Figure
Reference
-
1. Shi HY, Ng SC. The state of the art on treatment of Crohn’s disease. J Gastroenterol. 2018; 53:989–998.
Article2. Harper PH, Fazio VW, Lavery IC, et al. The long-term outcome in Crohn’s disease. Dis Colon Rectum. 1987; 30:174–179.
Article3. Munkholm P, Langholz E, Davidsen M, Binder V. Disease activity courses in a regional cohort of Crohn’s disease patients. Scand J Gastroenterol. 1995; 30:699–706.
Article4. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000; 231:38–45.
Article5. Greenstein AJ, Zhang LP, Miller AT, et al. Relationship of the number of Crohn’s strictures and strictureplasties to postoperative recurrence. J Am Coll Surg. 2009; 208:1065–1070.
Article6. Limketkai BN, Parian AM, Shah ND, Colombel JF. Short bowel syndrome and intestinal failure in Crohn’s disease. Inflamm Bowel Dis. 2016; 22:1209–1218.
Article7. Scimeca D, Mocciaro F, Cottone M, et al. Efficacy and safety of endoscopic balloon dilation of symptomatic intestinal Crohn’s disease strictures. Dig Liver Dis. 2011; 43:121–125.
Article8. Saunders BP, Brown GJ, Lemann M, Rutgeerts P. Balloon dilation of ileocolonic strictures in Crohn’s disease. Endoscopy. 2004; 36:1001–1007.
Article9. Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013; 62:1072–1084.
Article10. Bettenworth D, Gustavsson A, Atreja A, et al. A pooled analysis of efficacy, safety, and long-term outcome of endoscopic balloon dilation therapy for patients with stricturing Crohn’s disease. Inflamm Bowel Dis. 2017; 23:133–142.
Article11. Matsuoka K, Kobayashi T, Ueno F, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J Gastroenterol. 2018; 53:305–353.
Article12. Lian L, Stocchi L, Remzi FH, Shen B. Comparison of endoscopic dilation vs surgery for anastomotic stricture in patients with Crohn’s disease following ileocolonic resection. Clin Gastroenterol Hepatol. 2017; 15:1226–1231.
Article13. Nishida Y, Hosomi S, Yamagami H, et al. Analysis of the risk factors of surgery after endoscopic balloon dilation for small intestinal strictures in Crohn’s disease using double-balloon endoscopy. Intern Med. 2017; 56:2245–2252.
Article14. Sunada K, Shinozaki S, Nagayama M, et al. Long-term outcomes in patients with small intestinal strictures secondary to Crohn’s disease after double-balloon endoscopy-assisted balloon dilation. Inflamm Bowel Dis. 2016; 22:380–386.15. Hirai F, Beppu T, Sou S, Seki T, Yao K, Matsui T. Endoscopic balloon dilatation using double-balloon endoscopy is a useful and safe treatment for small intestinal strictures in Crohn’s disease. Dig Endosc. 2010; 22:200–204.
Article16. Hirai F, Beppu T, Takatsu N, et al. Long-term outcome of endoscopic balloon dilation for small bowel strictures in patients with Crohn’s disease. Dig Endosc. 2014; 26:545–551.
Article17. Okazaki N, Inokuchi T, Hiraoka S, et al. Findings of retrograde contrast study through double-balloon enteroscopy predict the risk of bowel resections in patients with Crohn’s disease with small bowel stenosis. Inflamm Bowel Dis. 2017; 23:2097–2103.
Article18. Sato K, Ito S, Shigiyama F, et al. A prospective randomized study on the benefits of a new small-caliber colonoscope. Endoscopy. 2012; 44:746–753.
Article19. Hosoe N, Ohtsuka K, Endo Y, et al. Insertability comparison of passive bending single-balloon prototype versus standard single-balloon enteroscopy: a multicenter randomized non-blinded trial. Endosc Int Open. 2018; 6:E1184–E1189.
Article20. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article21. May A, Nachbar L, Schneider M, Neumann M, Ell C. Pushand-pull enteroscopy using the double-balloon technique: method of assessing depth of insertion and training of the enteroscopy technique using the Erlangen Endo-Trainer. Endoscopy. 2005; 37:66–70.
Article22. Morar PS, Faiz O, Warusavitarne J, et al. Systematic review with meta-analysis: endoscopic balloon dilatation for Crohn’s disease strictures. Aliment Pharmacol Ther. 2015; 42:1137–1148.
Article23. Navaneethan U, Lourdusamy V, Njei B, Shen B. Endoscopic balloon dilation in the management of strictures in Crohn’s disease: a systematic review and meta-analysis of non-randomized trials. Surg Endosc. 2016; 30:5434–5443.
Article24. Mao R, Chen BL, He Y, Cui Y, Zeng ZR, Chen MH. Factors associated with progression to surgery in Crohn’s disease patients with endoscopic stricture. Endoscopy. 2014; 46:956–962.
Article25. Takenaka K, Ohtsuka K, Kitazume Y, et al. Comparison of magnetic resonance and balloon enteroscopic examination of the small intestine in patients with Crohn’s disease. Gastroenterology. 2014; 147:334–342.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does Single Balloon Enteroscopy Have Similar Efficacy and Endoscopic Performance Compared with Double Balloon Enteroscopy?
- A Case of Primary Small Bowel Melanoma Diagnosed by Single-Balloon Enteroscopy
- Deep Enteroscopy: Which Technique Will Survive?
- Small Bowel Stent-in-Stent Placement for Malignant Small Bowel Obstruction Using a Balloon-Assisted Overtube Technique
- Diagnostic and Therapeutic Capability of Double-Balloon Enteroscopy in Clinical Practice