Intest Res.
2020 Apr;18(2):210-218. 10.5217/ir.2019.00091.
Histologically confirmed upper gastrointestinal Crohn’s disease: is it rare or are we just not searching hard enough?
- Affiliations
-
- 1Department of Pediatrics, King Abdulaziz University Faculty of Medicine, Jeddah, Saudi Arabia
- 2Inflammatory Bowel Disease Research Group, King Abdulaziz University, Jeddah, Saudi Arabia
- 3Department of Medicine, King Abdulaziz University Faculty of Medicine, Jeddah, Saudi Arabia
- 4Clinical Research Support Facility, Methodological and Statistical Unit, University Hospital of Nancy, Nancy, France
- 5Department of Pathology, King Abdulaziz University Faculty of Medicine, Jeddah, Saudi Arabia
- KMID: 2501386
- DOI: http://doi.org/10.5217/ir.2019.00091
Abstract
- Background/Aims
Crohn’s disease (CD) may involve the upper parts of the gastrointestinal (GI) tract including the esophagus, stomach, and duodenum. Clinical features of upper GI CD (UGICD) are not well characterized in the Gulf region. We therefore aimed to assess the prevalence and clinical characteristics of patients diagnosed with UGICD.
Methods
We performed a retrospective analysis of all patients diagnosed with CD who underwent upper GI endoscopy between 2012 and 2017 at King Abdulaziz University Hospital, irrespective of age. Patients who had endoscopy of the upper GI tract at baseline and had histologically confirmed UGICD were included. Data on patients’ demographics, clinical characteristics, extraintestinal manifestations and complications were reviewed.
Results
We identified 78 CD patients who underwent upper GI endoscopy from our medical records. The mean age was 17.2±8.7 years and 55.1% were males. Of the total, 19 out of 78 patients (24.4%) had histologically confirmed UGICD (3 esophageal, 16 gastric, and 9 duodenal), of which 52.6% were symptomatic. Disease distribution was ileal in 57.8%, colonic in 21.1% and ileo-colonic in 21.1%. A non-stricturing and non-penetrating phenotype was reported in 89.4%, stricturing in 5.3%, and penetrating in 5.3%. Perianal disease was found in 10.5%. UGICD was complicated by stricture formation in 2 patients (esophageal and gastric).
Conclusions
The prevalence of UGICD is considered high among CD Saudi patients who undergo upper GI endoscopy at baseline, and is asymptomatic in 47.4% of patients. This reported prevalence is not dissimilar from reports originating from Western countries.
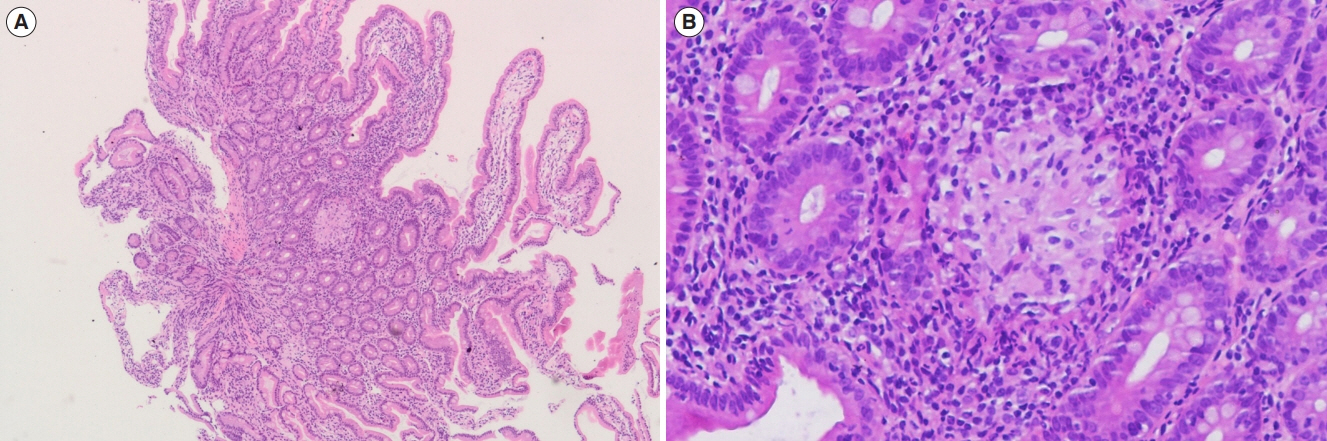
Figure
Reference
-
1. Kaser A, Zeissig S, Blumberg RS. Inflammatory bowel disease. Annu Rev Immunol. 2010; 28:573–621.
Article2. Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019; 13:144–164.
Article3. Schwartzberg DM, Brandstetter S, Grucela AL. Crohn’s disease of the esophagus, duodenum, and stomach. Clin Colon Rectal Surg. 2019; 32:231–242.
Article4. Goodhand J, Dawson R, Hefferon M, et al. Inflammatory bowel disease in young people: the case for transitional clinics. Inflamm Bowel Dis. 2010; 16:947–952.5. Ramaswamy K, Jacobson K, Jevon G, Israel D. Esophageal Crohn disease in children: a clinical spectrum. J Pediatr Gastroenterol Nutr. 2003; 36:454–458.
Article6. Levine YY, Koletzko J, Turner D. ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. Zhonghua Er Ke Za Zhi. 2016; 54:728–732.
Article7. Horjus Talabur Horje CS, Meijer J, Rovers L, van Lochem EG, Groenen MJ, Wahab PJ. Prevalence of upper gastrointestinal lesions at primary diagnosis in adults with inflammatory bowel disease. Inflamm Bowel Dis. 2016; 22:1896–1901.
Article8. Alcántara M, Rodriguez R, Potenciano JL, Carrobles JL, Muñoz C, Gomez R. Endoscopic and bioptic findings in the upper gastrointestinal tract in patients with Crohn’s disease. Endoscopy. 1993; 25:282–286.
Article9. Wagtmans MJ, van Hogezand RA, Griffioen G, Verspaget HW, Lamers CB. Crohn’s disease of the upper gastrointestinal tract. Neth J Med. 1997; 50:S2–S7.
Article10. Witte AM, Veenendaal RA, Van Hogezand RA, Verspaget HW, Lamers CB. Crohn’s disease of the upper gastrointestinal tract: the value of endoscopic examination. Scand J Gastroenterol Suppl. 1998; 225:100–105.11. Korelitz BI, Waye JD, Kreuning J, et al. Crohn’s disease in endoscopic biopsies of the gastric antrum and duodenum. Am J Gastroenterol. 1981; 76:103–109.12. Song XM, Gao X, Li MZ, et al. Clinical features and risk factors for primary surgery in 205 patients with Crohn’s disease: analysis of a South China cohort. Dis Colon Rectum. 2011; 54:1147–1154.
Article13. Magro F, Langner C, Driessen A, et al. European consensus on the histopathology of inflammatory bowel disease. J Crohns Colitis. 2013; 7:827–851.
Article14. Feakins RM; British Society of Gastroenterology. Inflammatory bowel disease biopsies: updated British Society of Gastroenterology reporting guidelines. J Clin Pathol. 2013; 66:1005–1026.
Article15. Geboes K, Janssens J, Rutgeerts P, Vantrappen G. Crohn’s disease of the esophagus. J Clin Gastroenterol. 1986; 8:31–37.
Article16. Ammoury RF, Pfefferkorn MD. Significance of esophageal Crohn disease in children. J Pediatr Gastroenterol Nutr. 2011; 52:291–294.
Article17. Crocco S, Martelossi S, Giurici N, Villanacci V, Ventura A. Upper gastrointestinal involvement in paediatric onset Crohn’s disease: prevalence and clinical implications. J Crohns Colitis. 2012; 6:51–55.
Article18. Renault M, Goodier A, Subramony C, Hood B, Bishop P, Nowicki M. Age-related differences in granulomatous gastritis: a retrospective, clinicopathological analysis. J Clin Pathol. 2010; 63:347–350.
Article19. Goldstein NS, Lewin KJ, Doty JE. Gastrointestinal tract. Pathology (Phila). 1996; 3:349–365.20. Kefalas CH. Gastroduodenal Crohn’s disease. Proc (Bayl Univ Med Cent). 2003; 16:147–151.
Article21. Reynolds HL Jr, Stellato TA. Crohn’s disease of the foregut. Surg Clin North Am. 2001; 81:117–135.
Article22. Yamamoto T, Bain IM, Connolly AB, Keighley MR. Gastroduodenal fistulas in Crohn’s disease: clinical features and management. Dis Colon Rectum. 1998; 41:1287–1292.23. Isaacs KL. Upper gastrointestinal tract endoscopy in inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2002; 12:451–462.
Article24. Pichney LS, Fantry GT, Graham SM. Gastrocolic and duodenocolic fistulas in Crohn’s disease. J Clin Gastroenterol. 1992; 15:205–211.
Article25. De Felice KM, Katzka DA, Raffals LE. Crohn’s disease of the esophagus: clinical features and treatment outcomes in the biologic era. Inflamm Bowel Dis. 2015; 21:2106–2113.26. Decker GA, Loftus EV Jr, Pasha TM, Tremaine WJ, Sandborn WJ. Crohn’s disease of the esophagus: clinical features and outcomes. Inflamm Bowel Dis. 2001; 7:113–119.
Article27. Mashako MN, Cezard JP, Navarro J, et al. Crohn’s disease lesions in the upper gastrointestinal tract: correlation between clinical, radiological, endoscopic, and histological features in adolescents and children. J Pediatr Gastroenterol Nutr. 1989; 8:442–446.28. Ruuska T, Vaajalahti P, Arajärvi P, Mäki M. Prospective evaluation of upper gastrointestinal mucosal lesions in children with ulcerative colitis and Crohn’s disease. J Pediatr Gastroenterol Nutr. 1994; 19:181–186.
Article29. Yamamoto T, Fazio VW, Tekkis PP. Safety and efficacy of strictureplasty for Crohn’s disease: a systematic review and metaanalysis. Dis Colon Rectum. 2007; 50:1968–1986.
Article30. Murray JJ, Schoetz DJ Jr, Nugent FW, Coller JA, Veidenheimer MC. Surgical management of Crohn’s disease involving the duodenum. Am J Surg. 1984; 147:58–65.
Article