Clin Endosc.
2020 Jan;53(1):90-93. 10.5946/ce.2019.036.
Acquired Hemophilia A with Gastrointestinal Bleeding
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea
- KMID: 2500910
- DOI: http://doi.org/10.5946/ce.2019.036
Abstract
- Peptic ulcer disease is the most common cause of acute gastrointestinal bleeding, followed by variceal bleeding, Mallory–Weiss syndrome, and malignancy. On the contrary, acquired hemophilia A is a very rare hemorrhagic disease, which usually manifests with musculocutaneous bleeding, caused by autoantibodies against coagulation factor VIII.
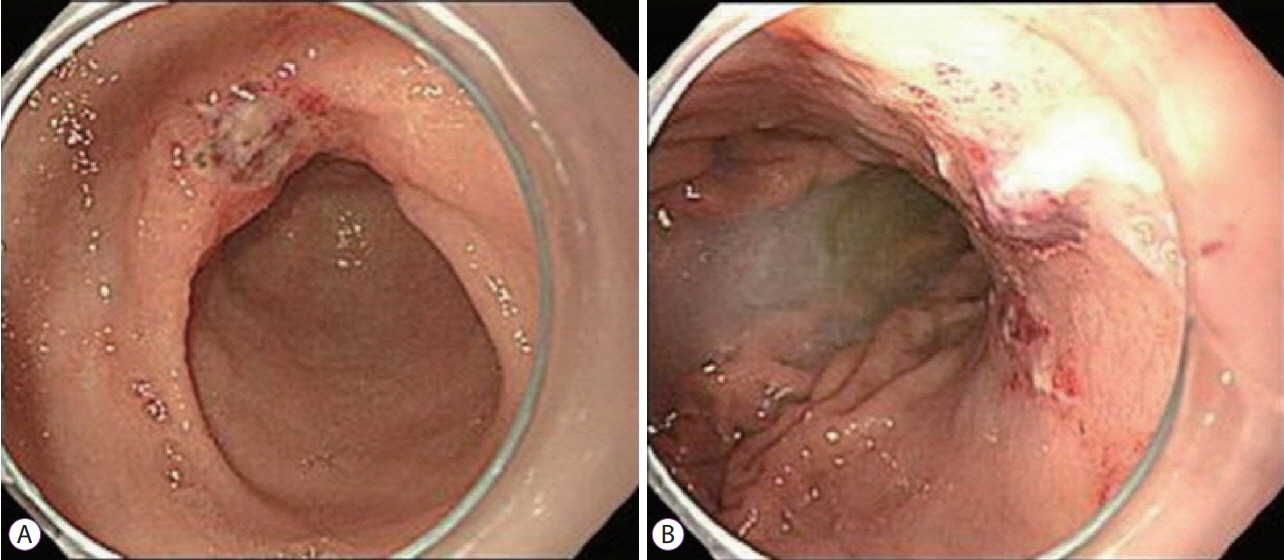
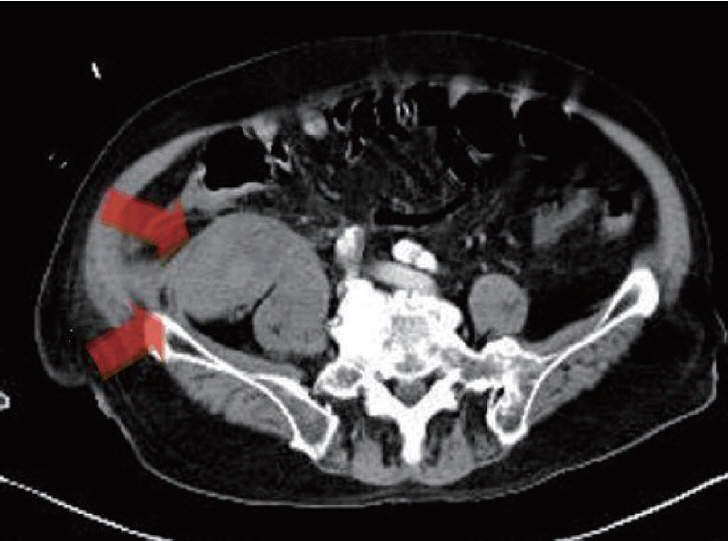
A 78-year-old man presented to the Emergency Department with melena. Dieulafoy’s lesions were observed on esophagogastroduodenoscopy, and endoscopic cauterization was performed. However, the patient complained of back pain and symptoms indicative of upper gastrointestinal bleeding. Abdominopelvic computed tomography was performed, and hematoma in the psoas muscle was detected. Antibodies against coagulation factor VIII were confirmed with a blood test, and the diagnosis of acquired hemophilia A was made. Here, we report a case of acquired hemophilia A presenting with upper gastrointestinal bleeding symptoms and present a brief review of literature.
Figure
Reference
-
1. Longstreth GF. Epidemiology of hospitalization for acute upper gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. 1995; 90:206–210.2. Czernichow P, Hochain P, Nousbaum JB, et al. Epidemiology and course of acute upper gastro-intestinal haemorrhage in four French geographical areas. Eur J Gastroenterol Hepatol. 2000; 12:175–181.
Article3. van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008; 22:209–224.
Article4. McCain S, Gull S, Ahmad J, Carey D. Acquired hemophilia A as a cause of acute upper gastrointestinal hemorrhage. BMJ Case Rep. 2014; 2014.
Article5. Kruse-Jarres R, Kempton CL, Baudo F, et al. Acquired hemophilia A: updated review of evidence and treatment guidance. Am J Hematol. 2017; 92:695–705.
Article6. Oldenburg J, Zeitler H, Pavlova A. Genetic markers in acquired haemophilia. Haemophilia. 2010; 16 Suppl 3:41–45.
Article7. Bitting RL, Bent S, Li Y, Kohlwes J. The prognosis and treatment of acquired hemophilia: a systematic review and meta-analysis. Blood Coagul Fibrinolysis. 2009; 20:517–523.
Article8. Franchini M, Gandini G, Di Paolantonio T, Mariani G. Acquired hemophilia A: a concise review. Am J Hematol. 2005; 80:55–63.
Article9. Delgado J, Jimenez-Yuste V, Hernandez-Navarro F, Villar A. Acquired haemophilia: review and meta-analysis focused on therapy and prognostic factors. Br J Haematol. 2003; 121:21–35.
Article10. Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician. 2007; 76:1005–1012.11. Kurata JH, Nogawa AN. Meta-analysis of risk factors for peptic ulcer. Nonsteroidal antiinflammatory drugs, Helicobacter pylori, and smoking. J Clin Gastroenterol. 1997; 24:2–17.12. Vreeburg EM, Snel P, de Bruijne JW, Bartelsman JF, Rauws EA, Tytgat GN. Acute upper gastrointestinal bleeding in the Amsterdam area: incidence, diagnosis, and clinical outcome. Am J Gastroenterol. 1997; 92:236–243.13. van Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003; 98:1494–1499.14. Barkun A, Sabbah S, Enns R, et al. The Canadian registry on nonvariceal upper gastrointestinal bleeding and endoscopy (RUGBE): endoscopic hemostasis and proton pump inhibition are associated with improved outcomes in a real-life setting. Am J Gastroenterol. 2004; 99:1238–1246.
Article15. Blatchford O, Davidson LA, Murray WR, Blatchford M, Pell J. Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study. BMJ. 1997; 315:510–514.
Article16. Cohen AJ, Kessler CM. Acquired inhibitors. Baillieres Clin Haematol. 1996; 9:331–354.17. Werwitzke S, Geisen U, Nowak-Göttl U, et al. Diagnostic and prognostic value of factor VIII binding antibodies in acquired hemophilia A: data from the GTH-AH 01/2010 study. J Thromb Haemost. 2016; 14:940–947.
Article18. Huth-Kühne A, Baudo F, Collins P, et al. International recommendations on the diagnosis and treatment of patients with acquired hemophilia A. Haematologica. 2009; 94:566–575.
Article19. Toh C-H, Alhamdi Y, Abrams ST. Current pathological and laboratory considerations in the diagnosis of disseminated intravascular coagulation. Ann Lab Med. 2016; 36:505–512.
Article20. Ma AD, Carrizosa D. Acquired factor VIII inhibitors: pathophysiology and treatment. Hematology Am Soc Hematol Educ Program. 2006; 432–437.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Knee Arthroplasty-associated Acquired Hemophilia: A Case Report
- Acquired Hemophilia: Successfully Treated with Plasma Exchange in a Patient with Hightiter Inhibitors
- Acquired Hemophilia in a Patient Presenting with Swollen Left Limb
- Emergency Department Visits in Hemophilia Patients
- The Effectiveness of Interventional Trans-Arterial Embolization to Control Active Bleeding Before Medical Treatment in Patients with Acquired Hemophilia Presenting as Retroperitoneal Hematoma and Hemothorax: A Case Report