Int J Stem Cells.
2020 Mar;13(1):93-103. 10.15283/ijsc18146.
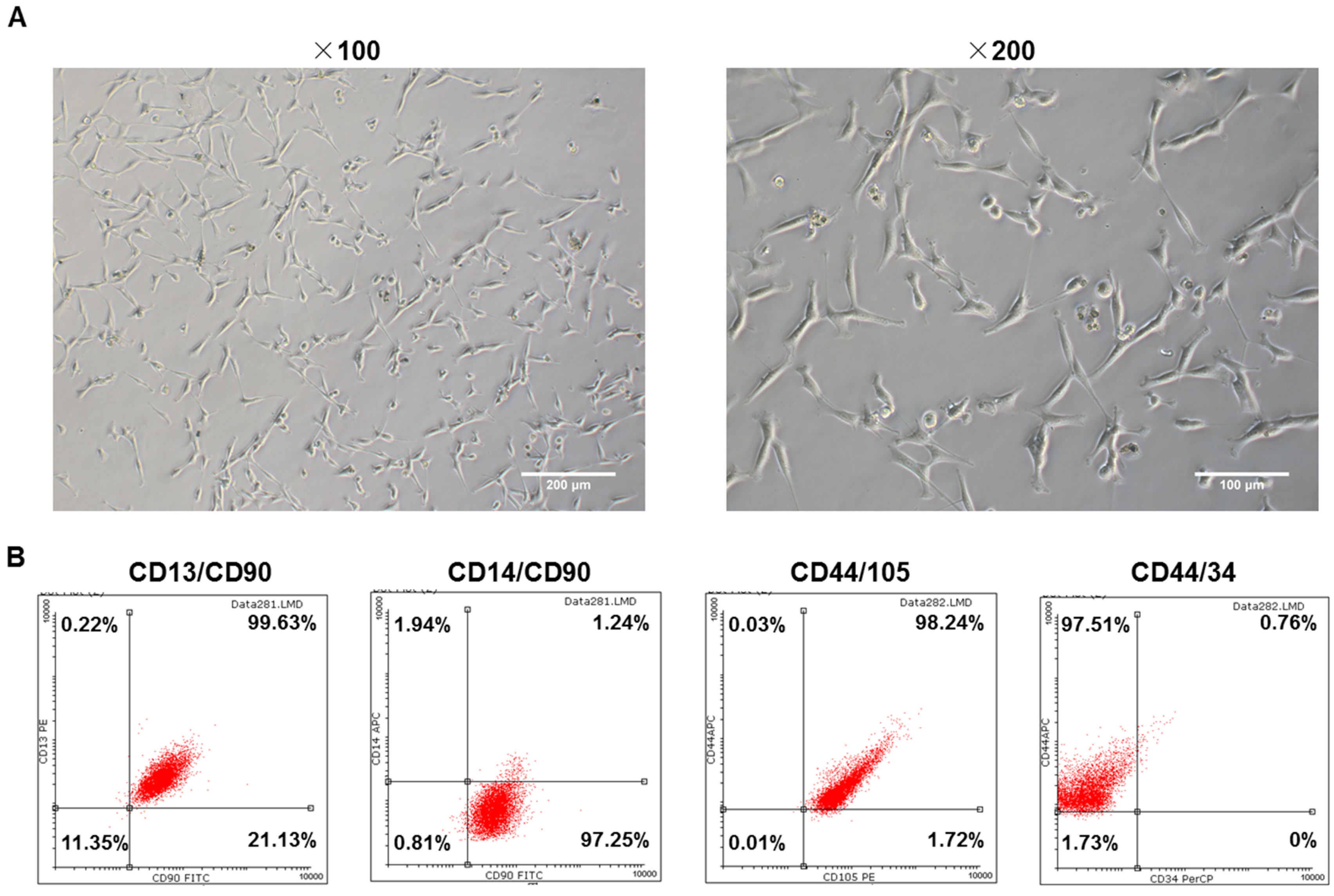
The Overexpression of Epidermal Growth Factor (EGF) in HaCaT Cells Promotes the Proliferation, Migration, Invasion and Transdifferentiation to Epidermal Stem Cell Immunophenotyping of Adipose-Derived Stem Cells (ADSCs)
- Affiliations
-
- 1Department of Dermatology, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
- 2Department of Dermatology, The Third Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- KMID: 2500569
- DOI: http://doi.org/10.15283/ijsc18146
Abstract
- Background and Objectives
The application of adipose derived stem cells (ADSCs) in skin repair has attracted much attention nowadays. Epidermal growth factor (EGF) participates in the progress of skin proliferation, differentiation and so forth. We aimed to explore the role of EGF in the proliferation, invasion, migration and transdifferentiation into epidermal cell phenotypes of ADSCs.
Methods and Results
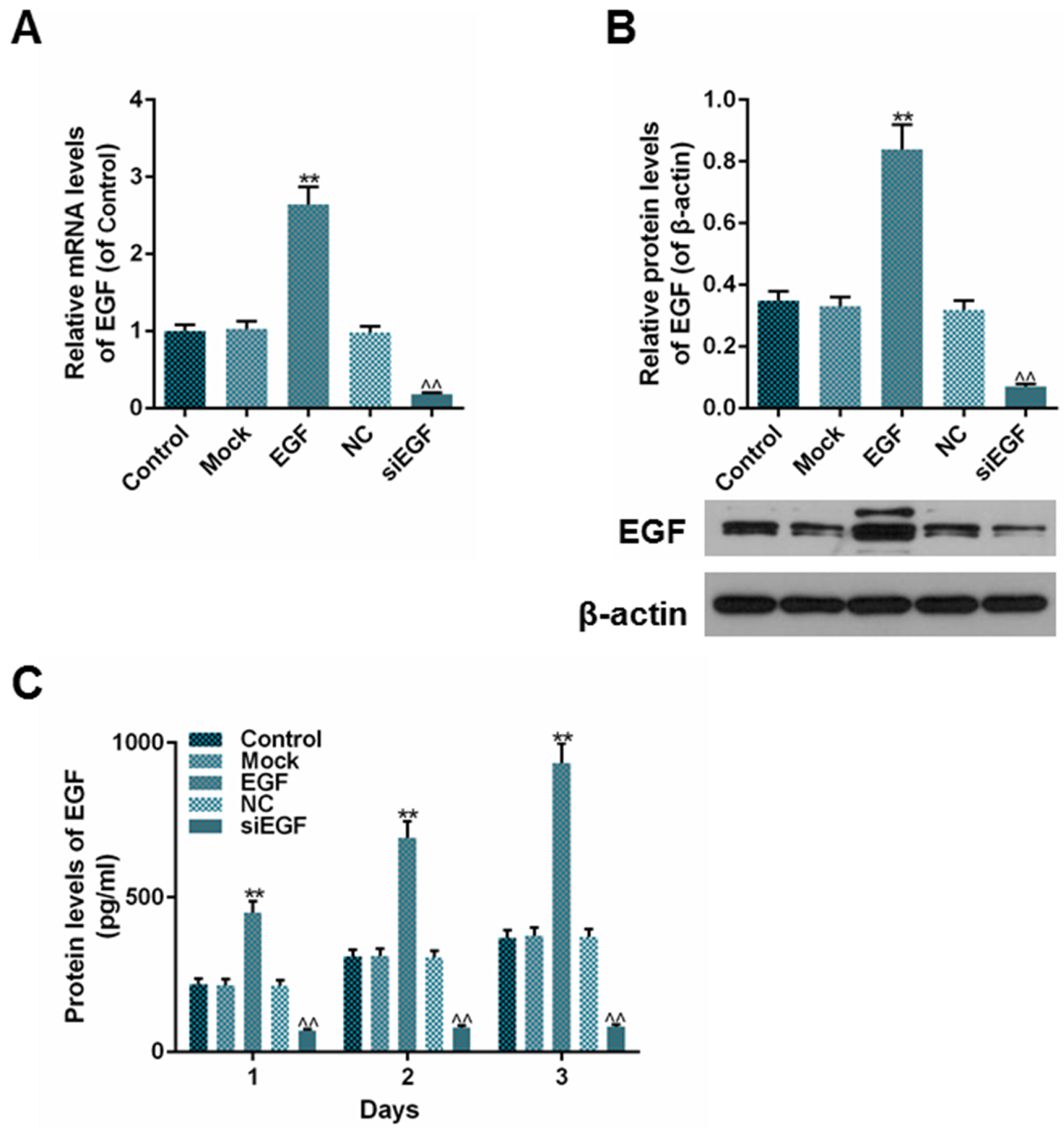
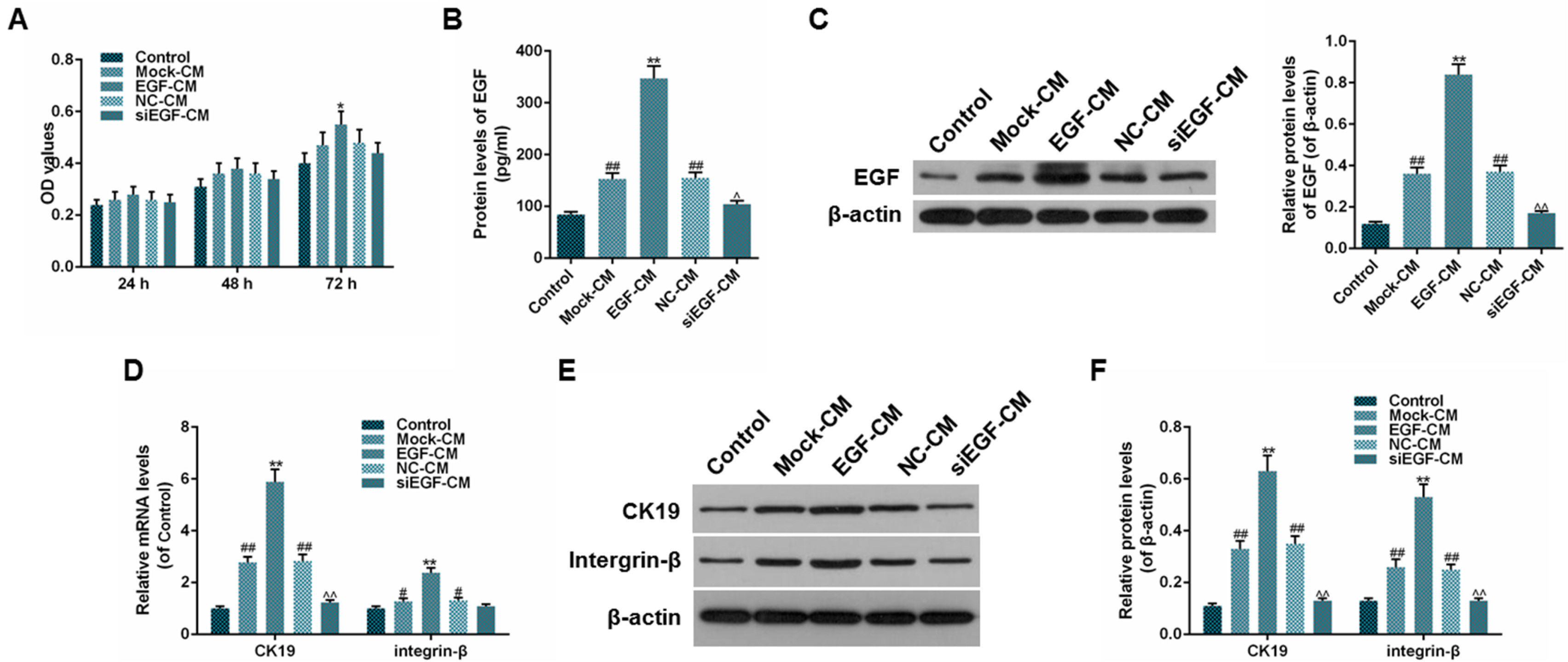
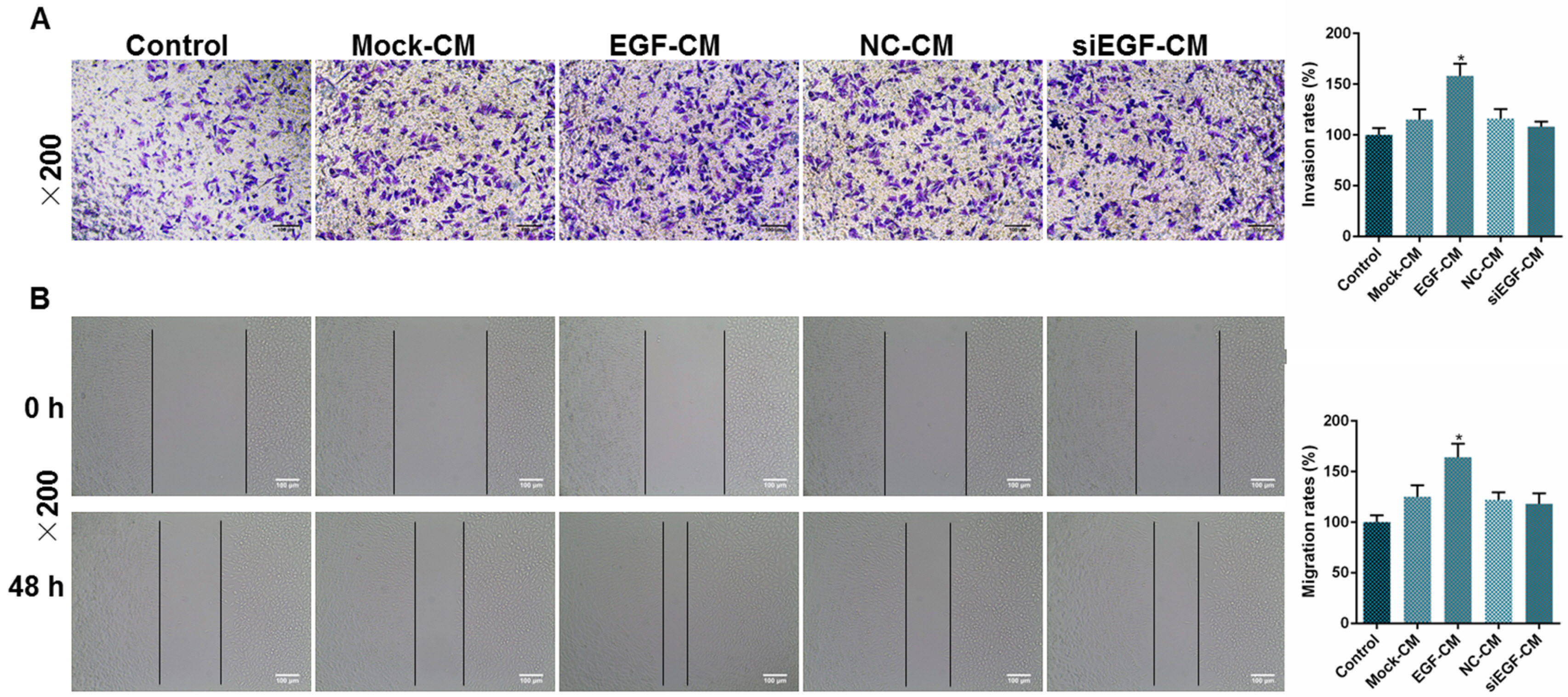
ADSCs were extracted from adipose tissues from patient. Immunophenotyping was determined by flow cytometry. Overexpressed EGF or siEGF was transfected by lentiviruses. EGF was determined by enzyme linked immunosorbent assay (ELISA) or western blot. ADSCs and HaCaT cells were co-cultured by Transwell chambers. Conditioned medium (CM) was obtained from cultured HaCaT cells and used for the culturing of ADSCs. Cell viability was tested by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. Invasion rate was measured by Transwell invasion assay and migration rate by wound healing test. mRNA and protein levels were measured by qPCR and western blot respectively. The extracted cells from adipose tissues were identified as ADSCs by morphology and immunophenotyping. The expression of EGF was up or down regulated constantly in HaCaT cell line after transfection. EGF overexpression upregulated the proliferation, migration and invasion rates of ADSCs, and EGF expression regulated the expression of cytokeratin-19 (CK19) and integrin-β as well.
Conclusions
EGF could be served as a stimulus to promote the proliferation, migration, and invasion as well as the transdifferentiation into epidermal stem cell immunophenotyping of ADSCs. The results showed that EGF had a promising effect on the repair of skin wound.
Keyword
Figure
Reference
-
References
1. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. 2015; Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centred approach. Update to a position statement of the American Diabetes Association and the European Association for the study of diabetes. Diabetologia. 58:429–442. DOI: 10.1007/s00125-014-3460-0. PMID: 25583541.
Article2. Takeo M, Lee W, Ito M. 2015; Wound healing and skin regeneration. Cold Spring Harb Perspect Med. 5:a023267. DOI: 10.1101/cshperspect.a023267. PMID: 25561722. PMCID: PMC4292081.
Article3. Sharma RR, Pollock K, Hubel A, McKenna D. 2014; Mesenchymal stem or stromal cells: a review of clinical applications and manufacturing practices. Transfusion. 54:1418–1437. DOI: 10.1111/trf.12421. PMID: 24898458. PMCID: PMC6364749.
Article4. Skubis A, Gola J, Sikora B, Hybiak J, Paul-Samojedny M, Mazurek U, Łos MJ. 2017; Impact of antibiotics on the proliferation and differentiation of human adipose-derived mesenchymal stem cells. Int J Mol Sci. 18:E2522. DOI: 10.3390/ijms18122522. PMID: 29186789. PMCID: PMC5751125.
Article5. Naderi N, Combellack EJ, Griffin M, Sedaghati T, Javed M, Findlay MW, Wallace CG, Mosahebi A, Butler PE, Seifalian AM, Whitaker IS. 2017; The regenerative role of adipose-derived stem cells (ADSC) in plastic and reconstructive surgery. Int Wound J. 14:112–124. DOI: 10.1111/iwj.12569. PMID: 26833722.
Article6. Brzoska M, Geiger H, Gauer S, Baer P. 2005; Epithelial differentiation of human adipose tissue-derived adult stem cells. Biochem Biophys Res Commun. 330:142–150. DOI: 10.1016/j.bbrc.2005.02.141. PMID: 15781243.
Article7. Yao YM, Yan H, Zhang ZM, Wu CF, Zhang L, Yang BB. 2016; [Effects of rabbit adipose-derived mesenchymal stem cells on the healing of skin deep partial-thickness scald wound of rabbit]. Zhonghua Shao Shang Za Zhi. 32:402–407. DOI: 10.3760/cma.j.issn.1009-2587.2016.07.004. PMID: 27464630. Chinese.8. Swindle CS, Tran KT, Johnson TD, Banerjee P, Mayes AM, Griffith L, Wells A. 2001; Epidermal growth factor (EGF)-like repeats of human tenascin-C as ligands for EGF receptor. J Cell Biol. 154:459–468. DOI: 10.1083/jcb.200103103. PMID: 11470832. PMCID: PMC2150768.
Article9. Alexandrescu DT, Kauffman CL, Dasanu CA. 2009; The cutaneous epidermal growth factor network: can it be translated clinically to stimulate hair growth? Dermatol Online J. 15:1. PMID: 19379645.
Article10. Long JL, Zuk P, Berke GS, Chhetri DK. 2010; Epithelial differentiation of adipose-derived stem cells for laryngeal tissue engineering. Laryngoscope. 120:125–131. DOI: 10.1002/lary.20719. PMID: 19856398.
Article11. Li H, Xu Y, Fu Q, Li C. 2012; Effects of multiple agents on epithelial differentiation of rabbit adipose-derived stem cells in 3D culture. Tissue Eng Part A. 18:1760–1770. DOI: 10.1089/ten.tea.2011.0424. PMID: 22497213. PMCID: PMC3432900.
Article12. Fève B. 2005; Adipogenesis: cellular and molecular aspects. Best Pract Res Clin Endocrinol Metab. 19:483–499. DOI: 10.1016/j.beem.2005.07.007. PMID: 16311213.
Article13. Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble JM. 2013; Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy. 15:641–648. DOI: 10.1016/j.jcyt.2013.02.006. PMID: 23570660. PMCID: PMC3979435.
Article14. Jiang A, Li M, Duan W, Dong Y, Wang Y. 2015; Improvement of the survival of human autologous fat transplantation by adipose-derived stem-cells-assisted lipotransfer combined with bFGF. ScientificWorldJournal. 2015:968057. DOI: 10.1155/2015/968057. PMID: 25695105. PMCID: PMC4324956.
Article15. Schoop VM, Mirancea N, Fusenig NE. 1999; Epidermal organization and differentiation of HaCaT keratinocytes in organotypic coculture with human dermal fibroblasts. J Invest Dermatol. 112:343–353. DOI: 10.1046/j.1523-1747.1999.00524.x. PMID: 10084313.
Article16. Tao K, Bai XZ, Zhang ZF, Shi JH, Hu XL, Tang CW, Hu DH, Han JT. 2013; Construction of the tissue engineering seed cell (HaCaT-EGF) and analysis of its biological characteristics. Asian Pac J Trop Med. 6:893–896. DOI: 10.1016/S1995-7645(13)60159-5. PMID: 24083586.
Article17. Hu DH, Zhang ZF, Zhang YG, Zhang WF, Wang HT, Cai WX, Bai XZ, Zhu HY, Shi JH, Tang CW. 2012; A potential skin substitute constructed with hEGF gene modified HaCaT cells for treatment of burn wounds in a rat model. Burns. 38:702–712. DOI: 10.1016/j.burns.2011.12.014. PMID: 22360951.
Article18. Paschos NK, Brown WE, Eswaramoorthy R, Hu JC, Athanasiou KA. 2015; Advances in tissue engineering through stem cell-based co-culture. J Tissue Eng Regen Med. 9:488–503. DOI: 10.1002/term.1870. PMID: 24493315.
Article19. Pawitan JA. 2014; Prospect of stem cell conditioned medium in regenerative medicine. Biomed Res Int. 2014:965849. DOI: 10.1155/2014/965849. PMID: 25530971. PMCID: PMC4229962.
Article20. Sugitani S, Tsuruma K, Ohno Y, Kuse Y, Yamauchi M, Egashira Y, Yoshimura S, Shimazawa M, Iwama T, Hara H. 2013; The potential neuroprotective effect of human adipose stem cells conditioned medium against light-induced retinal damage. Exp Eye Res. 116:254–264. DOI: 10.1016/j.exer.2013.09.013. PMID: 24076412.
Article21. Satarian L, Javan M, Kiani S, Hajikaram M, Mirnajafi-Zadeh J, Baharvand H. 2013; Engrafted human induced pluripotent stem cell-derived anterior specified neural progenitors protect the rat crushed optic nerve. PLoS One. 8:e71855. DOI: 10.1371/journal.pone.0071855. PMID: 23977164. PMCID: PMC3747054.
Article22. Mvula B, Moore TJ, Abrahamse H. 2010; Effect of low-level laser irradiation and epidermal growth factor on adult human adipose-derived stem cells. Lasers Med Sci. 25:33–39. DOI: 10.1007/s10103-008-0636-1. PMID: 19172344.
Article23. Jia YY, Zhou JY, Chang Y, An F, Li XW, Xu XY, Sun XL, Xiong CY, Wang JL. 2018; Effect of optimized concentrations of basic fibroblast growth factor and epidermal growth factor on proliferation of fibroblasts and expression of collagen: related to pelvic floor tissue regeneration. Chin Med J (Engl). 131:2089–2096. DOI: 10.4103/0366-6999.239301. PMID: 30127219. PMCID: PMC6111681.
Article24. Suzuki Y, Yanagisawa M, Yagi H, Nakatani Y, Yu RK. 2010; Involvement of beta1-integrin up-regulation in basic fibroblast growth factor- and epidermal growth factor-induced proliferation of mouse neuroepithelial cells. J Biol Chem. 285:18443–18451. DOI: 10.1074/jbc.M110.114645. PMID: 20371608. PMCID: PMC2881770.
Article25. Watt FM. 1998; Epidermal stem cells: markers, patterning and the control of stem cell fate. Philos Trans R Soc Lond B Biol Sci. 353:831–837. DOI: 10.1098/rstb.1998.0247. PMID: 9684280. PMCID: PMC1692275.
Article26. Michel M, Török N, Godbout MJ, Lussier M, Gaudreau P, Royal A, Germain L. 1996; Keratin 19 as a biochemical marker of skin stem cells in vivo and in vitro: keratin 19 expressing cells are differentially localized in function of anatomic sites, and their number varies with donor age and culture stage. J Cell Sci. 109(Pt 5):1017–1028. PMID: 8743949.
Article27. Adelsman MA, McCarthy JB, Shimizu Y. 1999; Stimulation of beta1-integrin function by epidermal growth factor and heregulin-beta has distinct requirements for erbB2 but a similar dependence on phosphoinositide 3-OH kinase. Mol Biol Cell. 10:2861–2878. DOI: 10.1091/mbc.10.9.2861. PMID: 10473632. PMCID: PMC25524.
Article28. Yoneda N, Sato Y, Kitao A, Ikeda H, Sawada-Kitamura S, Miyakoshi M, Harada K, Sasaki M, Matsui O, Nakanuma Y. 2011; Epidermal growth factor induces cytokeratin 19 expression accompanied by increased growth abilities in human hepatocellular carcinoma. Lab Invest. 91:262–272. DOI: 10.1038/labinvest.2010.161. PMID: 20856226.
Article29. Makarova G, Bette M, Schmidt A, Jacob R, Cai C, Rodepeter F, Betz T, Sitterberg J, Bakowsky U, Moll R, Neff A, Sesterhenn A, Teymoortash A, Ocker M, Werner JA, Mandic R. 2013; Epidermal growth factor-induced modulation of cytokeratin expression levels influences the morphological phenotype of head and neck squamous cell carcinoma cells. Cell Tissue Res. 351:59–72. DOI: 10.1007/s00441-012-1500-y. PMID: 23111772.
Article30. Chen R, Jin G, Li W, McIntyre TM. 2018; Epidermal Growth Factor (EGF) autocrine activation of human platelets promotes EGF receptor-dependent oral squamous cell carcinoma invasion, migration, and epithelial mesenchymal transition. J Immunol. 201:2154–2164. DOI: 10.4049/jimmunol.1800124. PMID: 30150285. PMCID: PMC6143412.
Article31. Tumur Z, Katebzadeh S, Guerra C, Bhushan L, Alkam T, Henson BS. 2015; RhoC mediates epidermal growth factor-stimulated migration and invasion in head and neck squamous cell carcinoma. Neoplasia. 17:141–151. DOI: 10.1016/j.neo.2014.12.002. PMID: 25622907. PMCID: PMC4309735.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Beta-Catenin Downregulation Contributes to Epidermal Growth Factor-induced Migration and Invasion of MDAMB231 Cells
- Hypoxia Pretreatment Promotes Chondrocyte Differentiation of Human Adipose-Derived Stem Cells via Vascular Endothelial Growth Factor
- Study on the Effects of Epidermal Growth Factor on Epidermal and Hair Growth in the Mouse
- Adipose-Derived Stem Cell Coculturing Stimulates Integrin-Mediated Extracellular Matrix Adhesion of Melanocytes by Upregulating Growth Factors
- In Vitro Study of Adipose-Derived Mesenchymal Stem Cells Transduced with Lentiviral Vector Carrying the Brain-Derived Neurotrophic Factor Gene